- Wiley Online Library
Anuncio
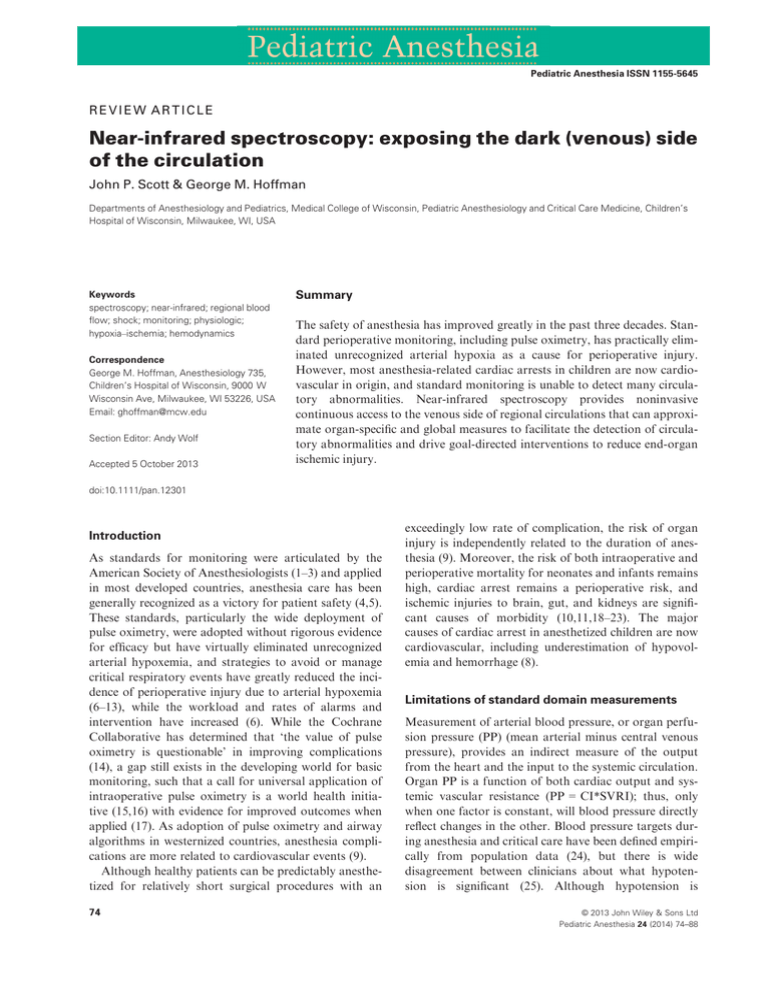
Pediatric Anesthesia ISSN 1155-5645 REVIEW ARTICLE Near-infrared spectroscopy: exposing the dark (venous) side of the circulation John P. Scott & George M. Hoffman Departments of Anesthesiology and Pediatrics, Medical College of Wisconsin, Pediatric Anesthesiology and Critical Care Medicine, Children’s Hospital of Wisconsin, Milwaukee, WI, USA Keywords spectroscopy; near-infrared; regional blood flow; shock; monitoring; physiologic; hypoxia–ischemia; hemodynamics Correspondence George M. Hoffman, Anesthesiology 735, Children’s Hospital of Wisconsin, 9000 W Wisconsin Ave, Milwaukee, WI 53226, USA Email: ghoffman@mcw.edu Section Editor: Andy Wolf Accepted 5 October 2013 Summary The safety of anesthesia has improved greatly in the past three decades. Standard perioperative monitoring, including pulse oximetry, has practically eliminated unrecognized arterial hypoxia as a cause for perioperative injury. However, most anesthesia-related cardiac arrests in children are now cardiovascular in origin, and standard monitoring is unable to detect many circulatory abnormalities. Near-infrared spectroscopy provides noninvasive continuous access to the venous side of regional circulations that can approximate organ-specific and global measures to facilitate the detection of circulatory abnormalities and drive goal-directed interventions to reduce end-organ ischemic injury. doi:10.1111/pan.12301 Introduction As standards for monitoring were articulated by the American Society of Anesthesiologists (1–3) and applied in most developed countries, anesthesia care has been generally recognized as a victory for patient safety (4,5). These standards, particularly the wide deployment of pulse oximetry, were adopted without rigorous evidence for efficacy but have virtually eliminated unrecognized arterial hypoxemia, and strategies to avoid or manage critical respiratory events have greatly reduced the incidence of perioperative injury due to arterial hypoxemia (6–13), while the workload and rates of alarms and intervention have increased (6). While the Cochrane Collaborative has determined that ‘the value of pulse oximetry is questionable’ in improving complications (14), a gap still exists in the developing world for basic monitoring, such that a call for universal application of intraoperative pulse oximetry is a world health initiative (15,16) with evidence for improved outcomes when applied (17). As adoption of pulse oximetry and airway algorithms in westernized countries, anesthesia complications are more related to cardiovascular events (9). Although healthy patients can be predictably anesthetized for relatively short surgical procedures with an 74 exceedingly low rate of complication, the risk of organ injury is independently related to the duration of anesthesia (9). Moreover, the risk of both intraoperative and perioperative mortality for neonates and infants remains high, cardiac arrest remains a perioperative risk, and ischemic injuries to brain, gut, and kidneys are significant causes of morbidity (10,11,18–23). The major causes of cardiac arrest in anesthetized children are now cardiovascular, including underestimation of hypovolemia and hemorrhage (8). Limitations of standard domain measurements Measurement of arterial blood pressure, or organ perfusion pressure (PP) (mean arterial minus central venous pressure), provides an indirect measure of the output from the heart and the input to the systemic circulation. Organ PP is a function of both cardiac output and systemic vascular resistance (PP = CI*SVRI); thus, only when one factor is constant, will blood pressure directly reflect changes in the other. Blood pressure targets during anesthesia and critical care have been defined empirically from population data (24), but there is wide disagreement between clinicians about what hypotension is significant (25). Although hypotension is © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 J.P. Scott and G.M. Hoffman common (26), the incidence of hypotension is highly dependent on the definition (27) and reporting is related to the occurrence of complications (28). There is little evidence that moderate hypotension is harmful and a lower safe limit could not be determined (29) except in the extreme (30). Conversely, serious hemorrhage and organ hypoperfusion can occur without significant change in blood pressure, even in anesthetized patients (31,32), and moderate hypotension may even improve outcome in resuscitation from shock (33). Inferences about blood flow from measures of blood pressure are unreliable (34) and may be counterintuitive (35). As measures of the relationship between blood pressure and organ perfusion reveal large inter- and intra-individual variations (36), it is not surprising that outcomes are largely unrelated to changes in blood pressure. The model of PP = CI*SVRI also implies that SVRI is a scalar variable, although the total resistance is actually composed of the inverse of sums of regional conductances, which are not clinically measurable and which are somewhat independent of each other. Thus, PP does not measure global or specific organ perfusion; with relatively fixed cardiac output, an increase in blood pressure will occur through a net increase in SVRI which is not likely to be evenly distributed across all vascular beds and thus will result from a change in the distribution of blood flow across organs. This implies that increasing blood pressure occurs through a reduction in blood flow to some regions. We need to measure more than blood pressure to improve outcomes related to circulation and organ perfusion. Standard hemodynamic monitors provide a minimal data set that crudely characterizes the circulation. Repetitive measurement and recording of heart rate, arterial blood pressure, and, recently, arterial oxygen saturation have been the basis for safety monitoring of the circulation in anesthesia and critical care, but in many instances, these parameters do not have adequate predictive or heuristic value. These supply-side measures are to the circulation what the fiO2 and breathing rate are to the respiratory system. For the circulation, the venous (postsystemic extraction) oxygen saturation provides a downstream signal about how the heart and circulatory system have functioned in systemic gas exchange. Near-infrared spectrometry (NIRS) is the ‘pulse ox for the circulation’ providing real-time, continuous, noninvasive, organ-specific, and quasi-global postextraction monitoring. Physiologic rationale Shock is the most common cause of pediatric cardiac arrest (37). Global, regional, or intraregional alteration © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 NIRS: exposing the circulatory dark side in oxygen delivery (DO2) creates a state of oxygen debt and anaerobic metabolism with failure to meet metabolic demand (oxygen consumption, VO2) (38–40). The severity and duration of oxygen debt in critical illness is directly linked to the development of end-organ ischemia, multiorgan failure and death (40,41). Prompt interventions directed at reversing oxygen debt are associated with improved outcomes (22,42,43). Delayed recognition and treatment of oxygen debt cause preventable morbidity and mortality (44). The anesthetized child is not immune from these principles and may be at higher risk because of surgical and anesthetic effects. Standard vital sign parameters are not highly predictive of the degree of circulatory failure and often underestimate the magnitude of oxygen debt (34,35). Biochemical indicators of organ hypoperfusion such as blood lactate, unmeasured anions, and base deficit correlate with the severity of oxygen debt and mortality (39,45), but cannot be continuously measured and lag circulatory changes. Systemic venous oxygen saturation (SvO2) monitoring provides an estimate of global oxygen balance according to the Fick equation SvO2 = SaO2 VO2/DO2 (35). Venous saturation may be sampled intermittently or continuously monitored via an oximetric catheter, and SvO2-guided resuscitation is associated with improved outcomes in shock (22,42). However, central venous line placement is invasive and often technically challenging in infants and small children, adding significant delay in both assessment and treatment. More importantly, SvO2 represents the flowweighted averages of individual organ saturations and may be insensitive to maldistribution of regional blood flows. In shock, elevated sympathetic tone redistributes blood flow away from splanchnic and mesenteric regions (35,46–49). Thus, regional ischemia may be clinically silent until organ dysfunction occurs, resulting in increased morbidity and mortality. Continuous noninvasive organ-specific perfusion monitoring is possible with infrared spectroscopy. NIRS is a completely noninvasive methodology now commonly used to measure regional tissue oxygenation and perfusion. The regional oxygen saturation (rSO2) approximates regional venous saturation, and in combination with arterial oxygen saturation allows for the estimation of regional oxygen economy. Manipulation of the regional Fick equation (rSO2 = SaO2 VO2/DO2) is often performed to derive regional arterio-venous difference (DarSO2 = SaO2 rSO2) or fractional oxygen extraction (fOE = [SaO2 rSO2]/SaO2), both of which are proportional to blood flow when hemoglobin concentration and metabolism are constant (35,50). Thus, NIRS opens a window for regional circulation monitoring that can drive organ-specific goal-directed treatments. 75 NIRS: exposing the circulatory dark side Technology Near-infrared spectrometry technologies derive estimates of physiologic measures by the application of modifications of the Beer Lambert law relating photon transmission to concentration of absorbers and scatterers in biologic suspensions. Near-infrared light passes through tissues, such as skin and bone, with minimal absorption. Significant biologic absorbers include heme-containing (hemoglobin) and nonheme-containing (bilirubin, myoglobin, cytochrome oxidase) chromophores, with oxyhemoglobin (HbO2) and deoxyhemoglobin (HbR) being the primary absorbers of nearinfrared light in blood (51–54). NIRS devices use laser or diode light sources to emit multiple wavelengths of near-infrared light (700–1000 nm). Because HbO2 and HbR have different absorption spectra, their concentrations can be derived by solution of multiple equations. Measurement of the light intensity at the isobestic point (the wavelength at which HbO2 and HbR absorb nearinfrared light equally) allows for an estimation of total Hb content. Although the concentrations of nonheme absorbers can degrade precision of absolute measurements, the ratio of HbO2/(HbO2 + HbR) is more robust (55–57). This estimate of field oxyhemoglobin saturation is termed regional saturation (rSO2) or tissue oxygenation index (TOI). For the validation of regional oxygen saturation, this field is modeled as lying between the arterial and regional venous blood. As 75–90% of the blood in tissue is postarteriolar, the rSO2 value is an estimate of regional venous saturation (54,55,58–61), NIRS devices provide saturation that is regional and optically weighted (rSO2), while intravascular catheters provide saturation that is regional and flow-weighted (SvO2); thus, the two measures are highly related but not equivalent. The clinical feasibility of NIRS derives from technologic optimization of the competing constraints of reflectance spectroscopy. While the absolute light path of an individual photon in suspension cannot be determined, the average photon path is an ellipse from light source to detector. The depth of this light path is approximately one-half of the source-detector distance. Larger sourcedetector separation yields deeper tissue interrogation but less photon recovery; these trade-offs are optimized with 4–5 cm source-detector separation. Most current (spatially resolved continuous wave) devices also include a near light path, and employ subtraction algorithms to reject measures from shallow tissue, effectively focusing the measure on deeper tissue (62). The resulting monitored field is 2–3 cm deep, making neonates, infants and children the ideal candidates for organ-specific circulation monitoring with NIRS. 76 J.P. Scott and G.M. Hoffman Animal and pediatric studies demonstrate good correlation between the rSO2C and jugular venous bulb saturation (SjvO2) (60,63–68). In all studies, the withinpatient trends were good, but absolute agreement is better in smaller heads, because the same sensor geometry interrogates a tissue field that is proportionally larger and deeper (69). Sensor location will be sensitive to heterogeneity within organs, but in the absence of cortical pathology, there is little difference between left, right, or midline forehead placement (57,70). Currently available devices are highly correlated with each other but do not show absolute equivalence (61,71). Unlike pulse oximetry, NIRS does not depend on a pulsatile signal, and thus, continuous oxygenation measures are available during all alterations of perfusion, including nonpulsatile cardiopulmonary bypass (CPB) and circulatory arrest, planned or otherwise (72–77). Normal measures In acyanotic humans, cerebral saturation (rSO2C) ranges between 60% and 80% (60,78–87). The regional blood flow/metabolism relationship can be better expressed by the arterial-NIRS difference (DarSO2) or the fOE, with normal cerebral fOE of 20–40%, and somatic fOE of 10–30%. The cerebral fOE drops in the minutes after birth, while the somatic fOE remains elevated for a longer period of time, perhaps related to later closure of the ductus arteriosus (83). In normal newborns in the first week of life (85), the average resting cerebral rSO2C was 77 8%, resting somatic-renal (rSO2S) 86 8%, and somatic-renal to cerebral difference (DrSO2SC) was 9 9%. Somatic measures showed greater variability within than between patients, indicating the state dependence of these measures (Figure 1). Cerebral oximetry Near-infrared spectrometry was initially developed to monitor the cerebral circulation. In adults, bilateral frontal cerebral oximetry is used to monitor perfusion to at risk areas of grey matter within cerebral cortex in the watershed areas between the anterior and middle cerebral arteries (88). The smaller head circumference of neonates and children permits greater depth of penetration of and assessment of subcortical tissue oxygenation (Figure 2) (69). Experimental data reveal a threshold for cerebral oxygen debt at rSO2C in the 35–45% range, which correspond to the 50% reduction in cerebral blood flow that produces injury (89). In animals, neuronal ATP depletion and development of cerebral anaerobic metabolism occurred with RSO2C <45%, hypoxic ischemic injury © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 J.P. Scott and G.M. Hoffman NIRS: exposing the circulatory dark side Figure 1 Normal values for cerebral and somatic (renal) regional saturation (rSO2) measures, derived from 25 normal newborns over the first 5 days of life. Individual measures were obtained at 10-s intervals over a 5-h period that included resting and feeding. Individual patient medians and ranges shown. Shaded regions are 95%CI for patient and population. Deeply shaded regions are mean and SD of patient means. The cerebral extraction was 20%, and the somatic extraction was 11%, with an average somatic-cerebral rSO2 difference was 9%. Although highly dynamic in the short term, the pattern of average somatic rSO2 exceeding average cerebral rSO2 was observed in 24/25 neonates, and there were no consistent or important changes in either measure in the transition from resting to feeding. From source (85) with permission. Figure 2 Areas of potential hypoxic–ischemic injury in the neonatal brain include moderate and deep cortical structures. The light path of a near-infrared (NIR) spectroscopy device applied to the frontal forehead will traverse areas at risk between the short- and longpenetrating arteries. More of these regions will be in the monitored field in neonates with small head dimensions. From source (69) with permission. Figure 3 Relation between near-infrared spectroscopy regional oxygen saturation (ScO2) and brain tissue lactate concentration in piglets. The lactate concentrate rose sharply at saturations <45%. Modified from source (90) with permission. occurred with rSO2C <40%, and neuronal cell death at an RSO2C <30% (Figure 3) (90,91). These data are consistent with clinical studies documenting worse neurologic outcomes in infants and children who experience prolonged normothermic cerebral saturation <40–50% (92–95). In children with congenital heart disease (CHD) requiring CPB, prolonged perioperative cerebral desaturation <45% was associated with abnormal brain © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 magnetic resonance (MRI) imaging findings (96,97) and worsened neurodevelopmental outcomes (97,98). Multisite oximetry Multisite oximetry can monitor the circulations in multiple organs, typically brain and a somatic organ such as the kidney, liver, intestine, or muscle. Typically, the cerebral circulation has tight flow-metabolism coupling driven by local autoregulatory mechanisms, while the 77 NIRS: exposing the circulatory dark side somatic circulations (rSO2S) have sympathetically modulated resistances that can alter rapidly with changes in autonomic outflow. A monitoring strategy that includes a cerebral and a noncerebral organ can assess oxygen delivery to organs with perfusion regulated by different neurohormonal mechanisms and thus reveal changes in the distribution of blood flow with changes in patient state that are completely invisible to global circulatory measures (99,100). Somatic NIRS saturation data have been validated for the detection of changes in perfusion of renal, hepatic, and mesenteric, and muscle circulations in animal and human catheter-based vascular occlusion procedures (101). Skeletal muscle blood flow and metabolism has been extensively interrogated with NIRS (55,102). In piglet models of renal, hepatic, or mesenteric ischemia, somatic NIRS values correlate well with organ-specific measurements of oxygen delivery, venous saturation, and lactate levels (103–107). Normothermic desaturation kinetics detected by NIRS are congruent with time dependence of ischemic injury of different organs (Figure 4) (104,105). In human studies, the greatest degree of agreement between somatic NIRS and organ-specific venous saturation data occur infants weighing <10 kg (101,108). The region specificity of NIRS is most obvious during interventions that produce major changes in the distribution of blood flow, including application of aortic cross-clamp during low-flow CPB with selective cerebral perfusion or coarctation repair (109–114). The somatic-cerebral saturation gradient (DrSO2SC) reflects differences in flow-metabolism ratios in each region, and these NIRS data are congruent with micropuncture measures of brain and kidney oxygen tension distributions (115,116). The DrSO2SC is a shorthand comparison of the arterial-somatic and J.P. Scott and G.M. Hoffman arterial-cerebral differences (or extractions) and is about 10–15% in normals and well-supported patients (35,85,105,117–119). The DrSO2SC narrows with activation of the sympathetic nervous system in response to stressors including early shock. Increased systemic vascular resistance maintains perfusion of heart and brain, at the expense of perfusion to the kidneys and mesenteric organs, with subsequent development of organ dysfunction and increased mortality (50,120,121). Two-site NIRS is valuable in the identification of somatic hypoperfusion in early compensated shock, as reduced renal/mesenteric perfusion may be clinically silent until organ dysfunction occurs (122– 124). As the mixed venous oxygen saturation is the flowweighted average of regional venous saturations, mathematical reconstructions of SvO2 from a multiple-site NIRS rSO2 measures perform better than single-site correlations (35,50,125–127). Two-site cerebral and renal somatic saturation data correlate well in linear models with SvO2 (35). For patients who do not have central access, two-site NIRS provides a surrogate SvO2 for rapid assessment and goal-directed treatment (Figure 5). In conjunction with pulse oximetry, this technique allows for a dynamic noninvasive estimate of regional and global oxygen extraction with adequate accuracy for clinical use (35,128). Near-infrared spectrometry and oxygen debt in congenital heart disease Children with CHD are at risk for global and regional oxygen debt. Ischemic neurologic injury and acute kidney injury (AKI) are the most common lasting manifestations of regional oxygen debt in survivors. Multisite rSO2-monitoring aids in the detection of low cardiac Figure 4 Near-infrared spectrometryderived desaturation curves from cerebral, mesenteric, renal, and skeletal muscle beds in isoflurane-anesthetized neonatal piglets during conditions of normothermic global ischemia induced by acute cardiac arrest. Data are expressed as the absolute change in regional saturation (rSO2) from baseline. Cerebral tissue has the most rapid desaturation during global ischemia, reflecting the highest ratio of oxygen consumption. From source (104) with permission. 78 © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 J.P. Scott and G.M. Hoffman NIRS: exposing the circulatory dark side Figure 5 Simultaneous measures of cerebral and somatic rSO2 and optically measured saturation from the superior vena cava (SvO2), in neonates following stage one palliation of hypoplastic left heart syndrome. A linear combination of both cerebral and renal rSO2 best fit the SvO2, with approximately equal weighting of cerebral and somatic sites. Adapted from source (35) with permission. output and organ-specific oxygen debt. Consequently, within our institution, two-site cerebral and renal NIRS monitoring has become standard for all phases of care in children with complex CHD (50,129,130). Preoperative NIRS monitoring has resulted in improved care delivery and decreased resource utilization in neonates with unpalliated hypoplastic left heart syndrome (HLHS). These infants have tenuous parallel circulation with threats to oxygen delivery from both arterial desaturation and low systemic perfusion. As pulmonary vascular resistance (PVR) decreases during the first days of life, pulmonary blood flow (QP) may increase at the expense of systemic blood flow (high QP:QS), which can be calculated from a modified Fick equation utilizing SaO2 and SvO2, and estimated with SvO2 reconstructed from multisite NIRS (105,131). Management without mechanical ventilation is enabled in infants with high SaO2 and preserved systemic perfusion monitored by NIRS, while those with evidence of systemic hypoperfusion received appropriate goal-directed interventions (132). We found that somatic blood flow (assessed by DarSO2S) was consistently reduced prior to stage one palliation but that these indices of perfusion were normalized by surgical palliation and support (Table 1). These neonates are extreme exemplars of patients with circulatory vulnerability related to both arterial hypoxemia and left to right shunts, demonstrating how NIRS monitoring provides continuous noninvasive diagnostic information to guide rational therapy. For example, provision of respiratory support to preterm infants with large patent ductus can worsen mesenteric perfusion as detected by increased mesenteric fOE (133). Postoperatively, low cardiac output syndrome (LCOS) is common, with the superimposition of ischemia reperfusion injury, myocardial edema and diastolic dysfunction, and changes in oxygen consumption (134,135). When combined with conventional pulse oximetry, NIRS derived indices of systemic perfusion have been successfully applied to identify neonates at risk for shock and guide appropriate therapy. In neonates following stage 1 palliation (S1P), reduced rSO2S and somatic-cerebral gradients were associated with increasing risk of biochemical shock, multiple organ dysfunction, and mortality (113,121,125,126,130,131,136– 138). In acyanotic infants and children undergoing biventricular repairs, average cerebral and somatic NIRS rSO2 values were inversely related to the development Table 1 Regional oxygenation by pulse oximetry (SaO2), cerebral (rSO2C), and renal somatic (rSO2S) Near-infrared spectrometry in normal newborns (85), and patients with HLHS before (132) and after (120) stage one palliation. Derived parameters are somatic-cerebral rSO2 difference (ΔrSO2SC), arterial-cerebral difference (ΔarSO2C) and arterial-somatic difference (ΔarSO2S). Somatic hypoperfusion is evident before palliation by a wide ΔarSO2S and a small somatic-cerebral difference (ΔrSO2SC). Although the absolute SaO2 and regional rSO2 after palliation is lower than normal newborns, the regional blood flow parameters, as reflected by arterial-regional differences, are normalized Parameters SaO2 rSO2C rSO2S ΔrSO2SC ΔarSO2C ΔarSO2S SvO2 Normal (N = 25, n = 17690) HLHS Pre-S1P (N = 47, n = 1831) 98 4 77.7 7.9 86.7 7.6 9.0 8.9 20.3 7.9 11.2 7.6 92.3 66.8 68.4 1.6 25.1 23.5 5.4a 8.5a 8.8a 9.4a,b 9.0 9.1a,b HLHS post-S1P (N = 41, n = 1554) 84.8 66.4 78.4 11.9 18.2 6.3 64.2 6.1a 9.0a 7.7a 9.4 8.6 7.3 9.6 HLHS, hypoplastic left heart syndrome; S1P, stage 1 palliation. Different from normal neonates. b Different from post-S1P. a © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 79 NIRS: exposing the circulatory dark side of organ hypoperfusion and anaerobic metabolism, with postoperative lactic acidosis associated with an average two-site NIRS saturation <65% (Figure 6) (125). Somatic measures may be valid from probe placements that target renal, mesenteric, or muscle beds (105,139). The circulatory complexity of patients with CHD has led to consensus recommendation for NIRS in single ventricle patients at risk for or being resuscitated from shock (37,50,140). In both cyanotic and acyanotic infants, two-site NIRS monitoring has increased the recognition of circulatory abnormalities and decreased the incidence of shock in our ICU (105,141). Hypoxic ischemic neurologic injury Ischemic neurologic injury is the most common sequelae of regional oxygen debt during and after pediatric heart surgery (94). The etiology of peri-CPB ischemic neurologic injury is multifactorial, including impairment of cerebral autoregulation, increased cerebral vascular resistance, deep hypothermic circulatory arrest (DHCA), and global LCOS (112,119,142,143). Cerebral oximetry is a critical tool in the detection of CPB-associated cerebral dysoxia. Cerebral desaturation, during rewarming and after CPB, is common and associated with cerebral injury (97,113,143–146), with higher thresholds during hypothermia (147,148). Although thresholds and intervention strategies based on cerebral NIRS that improve outcome are incompletely validated (93), neurodevelopmental outcomes can be normal with application of cerebral goal-directed approaches (98,143,149). CPB is associated with impaired cerebral autoregulation resulting in pressure-dependent flow, maldistribution of cerebral blood flow, and increased risk of Figure 6 A linear combination of cerebral and somatic rSO2 was highly related to blood lactate concentration in infants and children following two-ventricle corrective surgery. Elevated lactate levels were seen when the linear combination was <65%. Modified from source (125) with permission. 80 J.P. Scott and G.M. Hoffman ischemic neurologic injury. Cerebral NIRS permits a continuous assessment of the lower limits of cerebral autoregulation. NIRS-derived indices of cerebral blood flow correlate well with transcranial doppler (TCD) measurements of the middle cerebral artery velocity and cerebral PP (150). Online detection of the lower limit of autoregulation, a concept fundamental to neurologic protection but elusive in individual determination, is apparent when changes in blood pressure and cerebral rSO2 are coherent, and this effect can be quantitated and automated to drive individualized targets for management (150,151). Deep hypothermic circulatory arrest is variably associated with adverse neurologic outcomes following cardiac surgery that are only loosely associated with total duration of arrest (152). Risk factors for neurologic insult during DHCA include the length of circulatory arrest, temperature, hematocrit, and pH management strategy. Cerebral NIRS monitoring has been utilized to identify at risk states during DHCA (148,153–156). With the degree of post-DHCA neurologic injury most closely related to the time spent at the rSO2C nadir, corresponding to a state of cerebral oxygen debt with and no cerebral oxygen consumption (143,157,158). NIRS-guided DHCA management strategies that include identification of the rSO2C nadir and avoidance of prolonged desaturation are associated with improved outcomes (143,149,157). The technique of selective antegrade cerebral pefusion (ACP) of the brain via the right inominate artery can reduce or eliminate the need for DHCA (110–113). Continuous rSO2C monitoring during ACP aids the detection of cerebral perfusion abnormalities and is critical to ensuring optimal cerebral flow and adequate antegrade flow. Animal and human data demonstrate improved cerebral outcomes only if ACP flow is adequate to normalize cerebral blood flow, detectable by TCD or NIRS (143,149,159–161). Early postoperative rSO2C depression following cardiac surgery is consistent with elevated post-CPB cerebral vascular resistance, which frequently occur following deep hypothermia (113,155). This phenomenon occurs after repair of one and two ventricle lesions at deep hypothermia (113,118,119). Abnormal cerebral vascular resistance contributes to restricted cerebral perfusion and potential cerebral ischemia, with highest risk in the first postoperative day (Figure 7) (98,118,119). Severe intraoperative (162) and postoperative (98,114) cerebral desaturation is associated with reduced neurodevelopmental performance in early childhood (Figure 8). The convergence of experimental and clincial findings make cerebral rSO2 a rational target for goal-directed therapy. © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 J.P. Scott and G.M. Hoffman Figure 7 In neonates following stage, one palliation hypoplastic left heart syndrome, an early postoperative period of cerebral desaturation was observed despite improving global hemodynamic measures, emphasizing the vulnerability of the cerebral circulation. The contributions of cerebral and somatic saturation to the superior vena cava saturation are also evident. From source (119) with permission. Acute kidney injury Post-CPB AKI remains a major source of morbidity in children with CHD. Over 40% of children with CHD develop AKI following bypass (163). The pathogenesis of CPB-related AKI is not completely understood, but renal ischemia is an important contributing factor to its development (105,164–166). In animals, exposure to CPB results in severe renal medullary hypoxia and increased rates of AKI (167). Biochemical detection of AKI includes measurement of serum creatinine and urine output, but these parameters are insensitive and lagging indicators of renal ischemia. Somatic-renal desaturation is an early predictor of postoperative renal dysfunction. In infants following biventricular repair, 2 h of rSO2R <50% was associated with a fourfold rate of AKI (164). Similarly, following single ventricle repair, rSO2R <60% for 1 h predicted an eightfold risk of AKI (105,165). Recent studies of biomarkers of AKI demonstrate rSO2R <50% is predictive of elevated urinary cystatin C, IL-18, and Kim-1, as well as increased morbidity and mortality (166). Somatic-renal regional oximetry can provide a target for intervention to reduce ischemic injury. Near-infrared spectrometry and sepsis-mediated oxygen debt Pediatric sepsis has high mortality when not rapidly reversed. The ability to reverse oxygen debt in sepsis is © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 NIRS: exposing the circulatory dark side Figure 8 Cerebral desaturation detected by near-infrared spectrometry in the 48 h following neonatal palliation of hypoplastic left heart syndrome was associated with poorer performance on a robust multi-domain neurodevelopmental measure (visual-motor integration scale) when tested 4–5 years of age. Adapted from (98) with permission. associated with improved survival. Physiologic measures associated with survival include the ability to increase cardiac index, DO2, and VO2 (40,168). Animal models of sepsis reveal a clear correlation between endotoxinmediated reductions in mesenteric perfusion, transcutaneous somatic NIRS, and invasive measures of mesenteric oxygen delivery (venous saturation, oxygen delivery, and lactate measurements) (106,107). Outcomes in sepsis and septic shock are improved when goal-directed treatments include circulatory optimization based on SvO2 measurement. Pediatric multisite NIRS monitoring approximates SvO2 measurements and allows goal-directed treatments to begin earlier, a most important factor in improved outcome (22,42,44). Failure to normalize both central and regional oxygen measures is associated with poor outcome in resuscitation from shock (169,170). Near-infrared spectrometry and oxygen debt in prematurity Regional oximetry in premature infants aids in the recognition of potentially devastating complications such as hypoxic neurologic injury and necrotizing enterocolitis (NEC). Cerebral oximetry in premature infants has been used to identify hypoxic and hyperemic states associated with adverse neurologic outcomes. In infants with severe birth asphyxia, irreversible neurologic injury resulting in neuronal cell death, loss of oxygen consumption and autoregulation was associated with abnormal elevation in rSO2C (171). Transient episodes of pressure passive cerebral blood flow are common in very low 81 NIRS: exposing the circulatory dark side birth weight premature infants, detectable by continuous cerebral oximetry (172,173). Persistent blood-pressure-dependent and high rSO2C values in very premature infants is indicative of loss of cerebral autoregulation and greater risk of peri-intraventricular hemorrhage (174). Preterm, septic, and surgical neonates are at risk for developing NEC. Mesenteric/splanchnic somatic oximetry has shown promise as a continuous noninvasive monitor in the detection of mesenteric perfusion (105,139,175). In piglets, anterior abdominal wall rSO2 values were significantly lower in animals who later developed NEC (176). In preterm infants, reduced splanchnic NIRS correlate with feeding intolerance and NEC (177), and premature neonates with acute surgical abdominal processes have reduced splanchnic to cerebral rSO2 gradients (178). This multisite approach has also been exploited to individualize the need for and response to blood transfusion (80,179,180). The recent finding of higher rates of NEC, death, and disability (but lower rates of retinopathy) in prematures subjected to an oxygen-restrictive management strategy emphasizes the potential for differential end-organ injury in vulnerable patients with otherwise-acceptable arterial saturation (181). Effects of anesthesia and interventions Deliberate and inadvertant changes in arterial, venous, and tissue pressure, body position, blood gas composition, temperature, hemoglobin concentration, and anesthetic depth occur routinely during anesthesia. Most drugs in the anesthesiologist’s armamentarium have direct or indirect effects on vascular tone, myocardial performance, and cerebral metabolism; these effects can be additive, competing, or idiosyncratic, and thus, the magnitude and direction of these effects are difficult to predict. The potent cerebral vasodilator J.P. Scott and G.M. Hoffman effects of anesthetic vapors have been extensively investigated in experimental settings (182) and are obvious with NIRS monitoring. Cerebral rSO2 also tends to increase with propofol and thiopental, but to decrease with etomidate (183). The regional hyperemia that accompanies sympathectomy with caudal or major regional local anesthetic block can be readily detected by NIRS (184,185). While the effect of changes in arterial pCO2 and hydrogen ion concentration on the regional circulations are well known to anesthesiologists, these remain only theoretic constructs without online measures. For example, hypercapnia dilates both cerebral and somatic arterioles, causes a degree of sympathetic activation, and increases PVR. In neonates and infants, the superimposition of these effects generally causes an increase in cerebral blood flow, but a decrease in somatic blood flow (Figure 9) (105,117,186,187). The complexity of effects of vasoactive drugs on the distribution of vascular resistances and myocardial function makes prediction of specific organ effects inaccurate. For example, the effects of epinephrine or norepinephrine on renal blood flow depend on a constellation of host and disease factors, and this variation drives the need for individualized therapies. Multisite NIRS monitoring allows observation of patient-specific effects of complex interventions on complex systems and provides more targets for individualized goal-directed treatment. Sources of error Errors in clinical application of NIRS devices are largely related to misunderstanding of the optical limitations, which are more significant in large patients (52,101,188), in whom abdominal organspecific measures may be invalid, but almost all patients have an accessible skeletal muscle field for Figure 9 Changes in arterial carbon dioxide tension (pCO2) can alter the distribution of regional vascular resistance and blood flow. In neonates, following stage one palliation of hypoplastic left heart syndrome, and increase in pCO2 causes an increase in cerebral blood flow and oxygenation, but this is mirrored by a reduction in renal-somatic blood flow and oxygenation. From source (186) with permission. 82 © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 J.P. Scott and G.M. Hoffman NIRS: exposing the circulatory dark side somatic monitoring. The optical field of current 4–5 cm source-detector distance devices will interrogate only about 1–2 cm3 of tissue, and both individual anatomic variation and intra-organ heterogeneity must be considered. Direct hyperbilirubinemia will cause a reduction in the rSO 2 relative to the regional venous measure, and this effect needs further quantification (189,190). Other sources of error are interpretive or inferential. The relationship between rSO2 and regional pO2 will depend on temperature, pCO2, and local factors, and both overly high and overly low tissue pO2 are associated with injury. Regional blood flow and saturation can change quickly, and overinterpretation of a single regional rSO2 measure as a global or persistent characteristic may be misguided. Conversely, disregard of worrisome rSO2 information in the face of normal blood pressure may not reflect understanding of the complexity of circulatory physiology. can be disruptive, challenging the anesthesiologist to re-interpret the clinical state with more a complex physiologic understanding. Noninvasive measurement of regional oxygen saturation with NIRS can provide a probe of organ-specific blood flow or oxygen supply/demand relationships that are good enough for use in a wide variety of clinical scenarios, but the current technology is more suitable for neonates, infants and small children. Future developments will permit more accurate measures in larger patients and those with other optical confounders and will allow greater spatial resolution. Through an understanding of both the principles and limitations of current and future devices and appropriate application of these technologies, venous oximetry with NIRS can do for the circulation monitoring what pulse oximetry has done for respiratory monitoring: provide continuous noninvasive information that can meaningfully increase recognition of venous desaturation, organ ischemia, and shock-like states. Summary The cardiovascular system is complex, and more multidimensional measures are necessary to describe and monitor its characteristics and function. Measures in both the pressure and oxygen domain can help decode whole body and regional pressure and flow changes, which are often in opposite directions; thus, the continuous availability of information from NIRS Acknowledgments Sources of funding: Internal Medical College of Wisconsin and Children’s Hospital of Wisconsin. Conflicts of interest No conflicts of interest declared. References 1 Eichhorn JH. Prevention of intraoperative anesthesia accidents and related severe injury through safety monitoring. Anesthesiology 1989; 70: 572–577. 2 Eichhorn JH, Cooper JB, Cullen DJ et al. Anesthesia practice standards at Harvard: a review. J Clin Anesth 1988; 1: 55–65. 3 Keats AS. Anesthesia mortality in perspective. Anesth Analg 1990; 71: 113–119. 4 Barach P, Small SD. Reporting and preventing medical mishaps: lessons from nonmedical near miss reporting systems. BMJ 2000; 320: 759. 5 Gaba DM. Anaesthesiology as a model for patient safety in health care. BMJ 2000; 320: 785. 6 Cooper JB, Cullen DJ, Nemeskal R et al. Effects of information feedback and pulse oximetry on the incidence of anesthesia complications. Anesthesiology 1987; 67: 686–694. 7 Moller JT, Johannessen NW, Espersen K et al. Randomized evaluation of pulse oximetry in 20,802 patients; II: perioper- © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 8 9 10 11 ative events and postoperative complications. Anesthesiology 1993; 78: 445–453. Bhananker SM, Ramamoorthy C, Geiduschek JM et al. Anesthesia-related cardiac arrest in children: update from the Pediatric Perioperative Cardiac Arrest Registry. Anesth Analg 2007; 105: 344–350. Cheney FW, Posner KL, Lee LA et al. Trends in anesthesia-related death and brain damage: a closed claims analysis. Anesthesiology 2006; 105: 1081–1086. Morray JP, Geiduschek JM, Ramamoorthy C et al. Anesthesia-related cardiac arrest in children: initial findings of the Pediatric Perioperative Cardiac Arrest (POCA) Registry. Anesthesiology 2000; 93: 6–14. Ramamoorthy C, Haberkern CM, Bhananker SM et al. Anesthesia-related cardiac arrest in children with heart disease: data from the Pediatric Perioperative Cardiac Arrest (POCA) registry. Anesth Analg 2010; 110: 1376–1382. 12 Shah A, Shelley KH. Is pulse oximetry an essential tool or just another distraction? The role of the pulse oximeter in modern anesthesia care. J Clin Monit Comput 2013; 27: 235–242. 13 Cote CJ, Goldstein EA, Cote MA et al. A single-blind study of pulse oximetry in children. Anesthesiology 1988; 68: 184–188. 14 Pedersen T, Møller AM, Hovhannisyan K. Pulse oximetry for perioperative monitoring. Cochrane Database Syst Rev 2009; 4: CD002013. 15 Merry A, Eichhorn J, Wilson I. Extending the WHO ‘Safe Surgery Saves Lives’ project through global oximetry. Anaesthesia 2009; 64: 1045–1048. 16 Merry AF, Cooper JB, Soyannwo O et al. International standards for a safe practice of anesthesia 2010. Can J Anaesth 2010; 57: 1027–1034. 17 Kwok AC, Funk LM, Baltaga R et al. Implementation of the World Health Organization surgical safety checklist, including introduction of pulse oximetry, in a 83 NIRS: exposing the circulatory dark side 18 19 20 21 22 23 24 25 26 27 28 29 84 resource-limited setting. Ann Surg 2013; 257: 633–639. Hoffman GM. Outcomes of pediatric anesthesia. Semin Pediatr Surg 2008; 17: 141– 151. Peddy SB, Hazinski MF, Laussen PC et al. Cardiopulmonary resuscitation: special considerations for infants and children with cardiac disease. Cardiol Young 2007; 17 (Suppl 2): 116–126. Goepfert MS, Richter HP, zu Eulenburg C et al. Individually Optimized Hemodynamic Therapy Reduces Complications and Length of Stay in the Intensive Care Unit. 2013. Hamilton MA, Cecconi M, Rhodes A. A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients. Anesth Analg 2011; 112: 1392–1402. de Oliveira CF, de Oliveira DS, Gottschald AF et al. ACCM/PALS haemodynamic support guidelines for paediatric septic shock: an outcomes comparison with and without monitoring central venous oxygen saturation. Intensive Care Med 2008; 34: 1065–1075. Rivers EP, Coba V, Whitmill M. Early goal-directed therapy in severe sepsis and septic shock: a contemporary review of the literature. Curr Opin Anaesthesiol 2008; 21: 128–140. Haque IU, Zaritsky AL. Analysis of the evidence for the lower limit of systolic and mean arterial pressure in children. Pediatr Crit Care Med 2007; 8: 138–144. Nafiu OO, Voepel-Lewis T, Morris M et al. How do pediatric anesthesiologists define intraoperative hypotension? Pediatr Anesth 2009; 19: 1048–1053. Nafiu OO, Kheterpal S, Morris M et al. Incidence and risk factors for preincision hypotension in a noncardiac pediatric surgical population. Pediatr Anesth 2009; 19: 232–239. Bijker JB, van Klei WA, Kappen TH et al. Incidence of intraoperative hypotension as a function of the chosen definition: literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology 2007; 107: 213–220. Taffe P, Sicard N, Pittet V et al. The occurrence of intra-operative hypotension varies between hospitals: observational analysis of more than 147,000 anaesthesia. Acta Anaesthesiol Scand 2009; 53: 995–1005. Bijker JB, van Klei WA, Vergouwe Y et al. Intraoperative hypotension and 1-year mortality after noncardiac surgery. Anesthesiology 2009; 111: 1217–1226. J.P. Scott and G.M. Hoffman 30 Walsh M, Devereaux PJ, Garg AX et al. Relationship between intraoperative mean arterial pressure and clinical outcomes after noncardiac surgery: toward an empirical definition of hypotension. Anesthesiology 2013; 119: 507–515. 31 Pizov R, Eden A, Bystritski D et al. Hypotension during gradual blood loss: waveform variables response and absence of tachycardia. Br J Anaesth 2012; 109: 911–918. 32 Stricker PA, Lin EE, Fiadjoe JE et al. Absence of tachycardia during hypotension in children undergoing craniofacial reconstruction surgery. Anesth Analg 2012; 115: 139–146. 33 Li T, Zhu Y, Fang Y et al. Determination of the optimal mean arterial pressure for postbleeding resuscitation after hemorrhagic shock in rats. Anesthesiology 2012; 116: 103–112. 34 Tibby SM, Hatherill M, Marsh MJ et al. Clinicians’ abilities to estimate cardiac index in ventilated children and infants. Arch Dis Child 1997; 77: 516–518. 35 Hoffman GM, Ghanayem NS, Tweddell JS. Noninvasive assessment of cardiac output. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2005: 12–21. 36 Brady K, Hogue CW. Intraoperative hypotension and patient outcome: does” one size fit all?”. Anesthesiology 2013; 119: 495–497. 37 Kleinman ME, Chameides L, Schexnayder SM et al. Pediatric advanced life support: 2010 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics 2010; 126: e1361–e1399. 38 Barbee RW, Reynolds PS, Ward KR. Assessing shock resuscitation strategies by oxygen debt repayment. Shock 2010; 33: 113–122. 39 Rixen D, Siegel JH. Bench-to-bedside review: oxygen debt and its metabolic correlates as quantifiers of the severity of hemorrhagic and post-traumatic shock. Crit Care 2005; 9: 441–453. 40 Shoemaker WC, Appel PL, Kram HB. Role of oxygen debt in the development of organ failure sepsis, and death in high-risk surgical patients. Chest 1992; 102: 208–215. 41 Shoemaker WC, Appel PL, Kram HB. Tissue oxygen debt as a determinant of postoperative organ failure. Prog Clin Biol Res 1989; 308: 133–136. 42 Rivers E, Nguyen B, Havstad S et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001; 345: 1368–1377. 43 Tweddell JS, Hoffman GM, Mussatto KA et al. Improved survival of patients undergoing palliation of hypoplastic left heart 44 45 46 47 48 49 50 51 52 53 54 55 56 57 syndrome: lessons learned from 115 consecutive patients. Circulation 2002; 106(12 Suppl 1): 182–189. Rivers EP. Early goal-directed therapy in severe sepsis and septic shock: converting science to reality. Chest 2006; 129: 217–218. Balasubramanyan N, Havens PL, Hoffman GM. Unmeasured anions identified by the Fencl-Stewart method predict mortality better than base excess, anion gap, and lactate in patients in the pediatric intensive care unit. Crit Care Med 1999; 27: 1577–1581. Ruokonen E, Takala J, Kari A. Regional blood flow and oxygen transport in patients with the low cardiac output syndrome after cardiac surgery. Crit Care Med 1993; 21: 1304–1311. Ruokonen E, Takala J, Kari A et al. Regional blood flow and oxygen transport in septic shock. Crit Care Med 1993; 21: 1296. Marik PE. Gastric intramucosal pH. A better predictor of multiorgan dysfunction syndrome and death than oxygen-derived variables in patients with sepsis. Chest 1993; 104: 225–229. Meier-Hellmann A, Hannemann L, Specht M et al. Relationship Between Mixed Venous and Hepatic Venous O2 Saturation in Patients with Septic Shock. Oxygen Transport to Tissue XV. New York, NY: Plenum Press, 1994: 701–707. Ghanayem NS, Wernovsky G, Hoffman GM. Near-infrared spectroscopy as a hemodynamic monitor in critical illness. Pediatr Crit Care Med 2011; 12(4 Suppl.): S27–S32. Jobsis FF. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science 1977; 198: 1264–1267. Wahr JA, Tremper KK, Samra S et al. Near-infrared spectroscopy: theory and applications. J Cardiothorac Vasc Anesth 1996; 10: 406–418. Kurth CD, Steven JM, Benaron D et al. Near-infrared monitoring of the cerebral circulation. J Clin Monit 1993; 9: 163–170. Kurth CD, Thayer WS. A multiwavelength frequency-domain near-infrared cerebral oximeter. Phys Med Biol 1999; 44: 727–740. Boushel R, Langberg H, Olesen J et al. Monitoring tissue oxygen availability with near infrared spectroscopy (NIRS) in health and disease. Scand J Med Sci Sports 2001; 11: 213–222. Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth 2009; 103(Suppl 1): i3–i13. Menke J, Voss U, Moller G et al. Reproducibility of cerebral near infrared spectroscopy in neonates. Biol Neonate 2003; 83: 6–11. © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 J.P. Scott and G.M. Hoffman 58 Ewert P, Kretschmar O, Peters B et al. Transcatheter closure of congenital ventricular septal defects. Z Kardiol 2004; 93: 147–155. Interventioneller Verschluss angeborener Ventrikelseptumdefekte. Breitere Indikationsstellung dank neuer Implantate. 59 Watzman HM, Kurth CD, Montenegro LM et al. Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology 2000; 93: 947–953. 60 Nagdyman N, Fleck T, Schubert S et al. Comparison between cerebral tissue oxygenation index measured by near-infrared spectroscopy and venous jugular bulb saturation in children. Intensive Care Med 2005; 31: 846–850. 61 Nagdyman N, Ewert P, Peters B et al. Comparison of different near-infrared spectroscopic cerebral oxygenation indices with central venous and jugular venous oxygenation saturation in children. Pediatr Anesth 2008; 18: 160–166. 62 Davie SN, Grocott HP. Impact of extracranial contamination on regional cerebral oxygen saturation: a comparison of three cerebral oximetry technologies. Anesthesiology 2012; 116: 834–840. 63 Abdul-Khaliq H, Troitzsch D, Berger F et al. Regional transcranial oximetry with near infrared spectroscopy (NIRS) in comparison with measuring oxygen saturation in the jugular bulb in infants and children for monitoring cerebral oxygenation [Regionale transkranielle Oxymetrie mit Nahinfrarot-Spektroskopie (NIRS) im Vergleich zur Messung der Sauerstoffsattigung im Bulbus jugularis bei Sauglingen und Kindern als Monitoring der zerebralen Oxygenierung]. Biomed Tech (Berl) 2000; 45: 328– 332. 64 Daubeney PE, Pilkington SN, Janke E et al. Cerebral oxygenation measured by nearinfrared spectroscopy: comparison with jugular bulb oximetry. Ann Thorac Surg 1996; 61: 930–934. 65 Pollard V, Prough DS, DeMelo AE et al. Validation in volunteers of a near-infrared spectroscope for monitoring brain oxygenation in vivo. Anesth Analg 1996; 82: 269– 277. 66 Leyvi G, Bello R, Wasnick JD et al. Assessment of cerebral oxygen balance during deep hypothermic circulatory arrest by continuous jugular bulb venous saturation and near-infrared spectroscopy. J Cardiothorac Vasc Anesth 2006; 20: 826–833. 67 Ricci M, Lombardi P, Schultz S et al. Nearinfrared spectroscopy to monitor cerebral oxygen saturation in single-ventricle physiology. J Thorac Cardiovasc Surg 2006; 131: 395–402. 68 Kreeger RN, Ramamoorthy C, Nicolson SC et al. Evaluation of pediatric near-infra- © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 NIRS: exposing the circulatory dark side 69 70 71 72 73 74 75 76 77 78 79 80 81 red cerebral oximeter for cardiac disease. Ann Thorac Surg 2012; 94: 1527–1533. Hoffman GM. Neurologic monitoring on cardiopulmonary bypass: what are we obligated to do? Ann Thorac Surg 2006; 81: S2373–S2380. Kishi K, Kawaguchi M, Yoshitani K et al. Influence of patient variables and sensor location on regional cerebral oxygen saturation measured by INVOS 4100 near-infrared spectrophotometers. J Neurosurg Anesthesiol 2003; 15: 302–306. Dix LM, van Bel F, Baerts W et al. Comparing near-infrared spectroscopy devices and their sensors for monitoring regional cerebral oxygen saturation in the neonate. Pediatr Res 2013; doi: 10.1038/pr.2013.133. [Epub ahead of print]. Abdul-Khaliq H, Troitzsch D, Schubert S et al. Cerebral oxygen monitoring during neonatal cardiopulmonary bypass and deep hypothermic circulatory arrest. Thorac Cardiovasc Surg 2002; 50: 77–81. Daubeney PE, Smith DC, Pilkington SN et al. Cerebral oxygenation during paediatric cardiac surgery: identification of vulnerable periods using near infrared spectroscopy. Eur J Cardiothorac Surg 1998; 13: 370–377. Kurth CD, Levy W, Chance B. Oxygen metabolism during circulatory arrest. J Neurosurg 1994; 81: 330–331. Kurth CD, Steven JM, Nicolson SC. Cerebral oxygenation during pediatric cardiac surgery using deep hypothermic circulatory arrest. Anesthesiology 1995; 82: 74–82. Kurth CD, Steven JM, Nicolson SC et al. Kinetics of cerebral deoxygenation during deep hypothermic circulatory arrest in neonates. Anesthesiology 1992; 77: 656–661. Nagdyman N, Fleck TP, Ewert P et al. Cerebral oxygenation measured by nearinfrared spectroscopy during circulatory arrest and cardiopulmonary resuscitation. Br J Anaesth 2003; 91: 438–442. Kim MB, Ward DS, Cartwright CR et al. Estimation of jugular venous O2 saturation from cerebral oximetry or arterial O2 saturation during isocapnic hypoxia. J Clin Monit Comput 2000; 16: 191–199. Tina LG, Frigiola A, Abella R et al. Near infrared spectroscopy in healthy preterm and term newborns: correlation with gestational age and standard monitoring parameters. Curr Neurovasc Res 2009; 6: 148–154. Dani C, Pratesi S, Fontanelli G et al. Blood transfusions increase cerebral, splanchnic, and renal oxygenation in anemic preterm infants. Transfusion 2010; 50: 1220–1226. Petrova A, Mehta R. Near-infrared spectroscopy in the detection of regional tissue 82 83 84 85 86 87 88 89 90 91 92 93 94 oxygenation during hypoxic events in preterm infants undergoing critical care. Pediatr Crit Care Med 2006; 7: 449–454. Dave V, Brion L, Campbell D et al. Splanchnic tissue oxygenation, but not brain tissue oxygenation, increases after feeds in stable preterm neonates tolerating full bolus orogastric feeding. J Perinatol 2008; 29: 213–218. Binder C, Urlesberger B, Avian A et al. Cerebral and peripheral regional oxygen saturation during postnatal transition in preterm neonates. J Pediatr 2013; 163: 394– 399. Pichler G, Binder C, Avian A et al. Reference ranges for regional cerebral tissue oxygen saturation and fractional oxygen extraction in neonates during immediate transition after birth. J Pediatr 2013; doi: 10.1016/j.jpeds.2013.07.007. Bernal NP, Hoffman GM, Ghanayem NS et al. Cerebral and somatic near-infrared spectroscopy in normal newborns. J Pediatr Surg 2010; 45: 1306–1310. Nagdyman N, Fleck T, Barth S et al. Relation of cerebral tissue oxygenation index to central venous oxygen saturation in children. Intensive Care Med 2004; 30: 468–471. Misra M, Stark J, Dujovny M et al. Transcranial cerebral oximetry in random normal subjects. Neurol Res 1998; 20: 137. Roesner JP, Koch A, Bateman R et al. Accurate and continuous measurement of oxygen deficit during haemorrhage in pigs. Resuscitation 2009; 80: 259–263. Ginsberg MD. Adventures in the pathophysiology of brain ischemia: penumbra, gene expression, neuroprotection: the 2002 Thomas Willis Lecture. Stroke 2003; 34: 214–223. Kurth CD, Levy WJ, McCann J. Nearinfrared spectroscopy cerebral oxygen saturation thresholds for hypoxia-ischemia in piglets. J Cereb Blood Flow Metab 2002; 22: 335–341. Kurth CD, McCann JC, Wu J et al. Cerebral oxygen saturation-time threshold for hypoxic-ischemic injury in piglets. Anesth Analg 2009; 108: 1268–1277. Levy WJ, Levin S, Chance B. Near-infrared measurement of cerebral oxygenation. Correlation with electroencephalographic ischemia during ventricular fibrillation. Anesthesiology 1995; 83: 738–746. Austin EH 3rd, Edmonds HL Jr, Auden SM et al. Benefit of neurophysiologic monitoring for pediatric cardiac surgery. J Thorac Cardiovasc Surg 1997; 114: 707–715, 17; discussion 15-6. Nollert G, Mohnle P, Tassani-Prell P et al. Postoperative neuropsychological dysfunction and cerebral oxygenation during 85 NIRS: exposing the circulatory dark side 95 96 97 98 99 100 101 102 103 104 86 cardiac surgery. Thorac Cardiovasc Surg 1995; 43: 260–264. Edmonds HL Jr, Ganzel BL, Austin EH 3rd. Cerebral oximetry for cardiac and vascular surgery. Semin Cardiothorac Vasc Anesth 2004; 8: 147–166. Dent CL, Spaeth JP, Jones BV et al. Brain magnetic resonance imaging abnormalities after the Norwood procedure using regional cerebral perfusion. J Thorac Cardiovasc Surg 2006; 131: 190–197. Kussman BD, Wypij D, Laussen PC et al. Relationship of intraoperative cerebral oxygen saturation to neurodevelopmental outcome and brain magnetic resonance imaging at 1 year of age in infants undergoing biventricular repair. Circulation 2010; 122: 245–254. Hoffman GM, Brosig CL, Mussatto KA et al. Perioperative cerebral oxygen saturation in neonates with hypoplastic left heart syndrome and childhood neurodevelopmental outcome. J Thorac Cardiovasc Surg 2013; 146: 1153–1164. Kraut A, Barbiro-Michaely E, Mayevsky A. Differential effects of norepinephrine on brain and other less vital organs detected by a multisite multiparametric monitoring system. Med Sci Monit 2004; 10: 220. Mandelbaum M, Barbiro-Michaely E, Tolmasov M et al., eds. Effects of severe hemorrhage in in-vivo brain and small intestine mitochondrial NADH and microcirculatory blood flow. advances in biomedical photonics and imaging. Proceedings of the 6th International Conference on Photonics and Imaging in Biology and Medicine (Pibm 2007) Wuhan, China, 4–6 November 2007; 2008: World Scientific. Booth EA, Dukatz C, Ausman J et al. Cerebral and somatic venous oximetry in adults and infants. Surg Neurol Int 2010; 1: 75. Wong JK, Smith TN, Pitcher HT et al. Cerebral and lower limb near-infrared spectroscopy in adults on extracorporeal membrane oxygenation. Artif Organs 2012; 36: 659–667. Hoffman GM, Wider MD. Organ specificity of rSO2 measurements during regional ischemia in piglets. Anesthesiology 2008; 109: A272. [Internet] Available at: http:// www.asaabstracts.com/strands/asaabstracts/abstract.htm? year=2008&index=6&absnum=1980. Accessed 5 January, 2011. Hoffman GM, Wider MD. Changes in regional oxygenation by NIRS during global ischemia in piglets. Anesthesiology 2008; 109: A1512. [Internet]. Available at: http:// www.asaabstracts.com/strands/asaabstracts/abstract.htm? year=2008&index=9&absnum=1984. Accessed 5 January, 2011. J.P. Scott and G.M. Hoffman 105 Hoffman GM, Tweddell JS. Regional blood flow monitoring in the perioperative period. In: Kleinman CS, Seri I, eds. Hemodynamics and Cardiology: Neonatology Questions and Controversies, 2nd edn. Philadelphia: W.B. Saunders, 2012: 473–487. 106 Nahum E, Skippen PW, Gagnon RE et al. Correlation of transcutaneous hepatic nearinfrared spectroscopy readings with liver surface readings and perfusion parameters in a piglet endotoxemic shock model. Liver Int 2006; 26: 1277–1282. 107 Nahum E, Skippen PW, Gagnon RE et al. Correlation of near-infrared spectroscopy with perfusion parameters at the hepatic and systemic levels in an endotoxemic shock model. Med Sci Monit 2006; 12: BR313– BR317. 108 Ortmann LA, Fontenot EE, Seib PM et al. Use of near-infrared spectroscopy for estimation of renal oxygenation in children with heart disease. Pediatr Cardiol 2011; 32: 748–753. 109 Pigula FA, Gandhi SK, Siewers RD et al. Regional low-flow perfusion provides somatic circulatory support during neonatal aortic arch surgery. Ann Thorac Surg 2001; 72: 401–406; discussion 6-7. 110 Pigula FA, Nemoto EM, Griffith BP et al. Regional low-flow perfusion provides cerebral circulatory support during neonatal aortic arch reconstruction. J Thorac Cardiovasc Surg 2000; 119: 331–339. 111 Andropoulos DB, Diaz LK, Fraser CD Jr et al. Is bilateral monitoring of cerebral oxygen saturation necessary during neonatal aortic arch reconstruction? Anesth Analg 2004; 98: 1267–1272; table of contents. 112 Andropoulos DB, Stayer SA, Diaz LK et al. Neurological monitoring for congenital heart surgery. Anesth Analg 2004; 99: 1365–1375; table of contents. 113 Hoffman GM, Stuth EA, Jaquiss RD et al. Changes in cerebral and somatic oxygenation during stage 1 palliation of hypoplastic left heart syndrome using continuous regional cerebral perfusion. J Thorac Cardiovasc Surg 2004; 127: 223–233. 114 Berens RJ, Stuth EA, Robertson FA et al. Near infrared spectroscopy monitoring during pediatric aortic coarctation repair. Pediatr Anesth 2006; 16: 777–781. 115 Baumgartl H, Zimelka W, Lubbers DW. Evaluation of PO(2) profiles to describe the oxygen pressure field within the tissue. Comp Biochem Physiol A Mol Integr Physiol 2002; 132: 75–85. 116 Lubbers DW, Baumgartl H. Heterogeneities and profiles of oxygen pressure in brain and kidney as examples of the pO2 distribution in the living tissue. Kidney Int 1997; 51: 372–380. 117 McQuillen PS, Nishimoto MS, Bottrell CL et al. Regional and central venous oxygen saturation monitoring following pediatric cardiac surgery: concordance and association with clinical variables. Pediatr Crit Care Med 2007; 8: 154–160. 118 Furck AK, Hansen JH, Uebing A et al. The impact of afterload reduction on the early postoperative course after the Norwood operation - a 12-year single-centre experience. Eur J Cardiothorac Surg 2010; 37: 289–295. 119 Uebing A, Furck AK, Hansen JH et al. Perioperative cerebral and somatic oxygenation in neonates with hypoplastic left heart syndrome or transposition of the great arteries. J Thorac Cardiovasc Surg 2011; 142: 523–530. 120 Hoffman GM, Ghanayem NS, Stuth EA et al. NIRS-derived somatic and cerebral saturation difference provides non-invasive real-time hemodynamic assessment of cardiogenic shock and risk of anaerobic metabolism. Anesthesiology 2004; 99: A1448. [Internet]. Available at: http:// www.asaabstracts.com/strands/asaabstracts/abstract.htm? year=2004&index=16&absnum=2206. Accessed 5 January, 2011. 121 Hoffman GM, Ghanayem NS, Mussatto KA et al. Postoperative two-site NIRS predicts complications and mortality after stage 1 palliation of HLHS. Anesthesiology 2007; 107: A234. [Internet]. Available at: http://www.asaabstracts.com/strands/asaabstracts/abstract.htm? year=2007&index=16&absnum=1585. Accessed 5 January, 2011. 122 Dyess DL, Powell RW, Swafford AN Jr et al. Redistribution of organ blood flow after hemorrhage and resuscitation in fullterm piglets. J Pediatr Surg 1994; 29: 1097– 1102. 123 Reilly PM, Wilkins KB, Fuh KC et al. The mesenteric hemodynamic response to circulatory shock: an overview. Shock 2001; 15: 329–343. 124 Ceppa EP, Fuh KC, Bulkley GB. Mesenteric hemodynamic response to circulatory shock. Curr Opin Crit Care 2003; 9: 127–132. 125 Chakravarti SB, Mittnacht AJ, Katz JC et al. Multisite near-infrared spectroscopy predicts elevated blood lactate level in children after cardiac surgery. J Cardiothorac Vasc Anesth 2009; 23: 663–667. 126 Li J, Van Arsdell GS, Zhang G et al. Assessment of the relationship between cerebral and splanchnic oxygen saturations measured by near-infrared spectroscopy and direct measurements of systemic haemodynamic variables and oxygen transport after the Norwood procedure. Heart 2006; 92: 1678–1685. © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 J.P. Scott and G.M. Hoffman 127 Redlin M, Koster A, Huebler M et al. Regional differences in tissue oxygenation during cardiopulmonary bypass for correction of congenital heart disease in neonates and small infants: relevance of near-infrared spectroscopy. J Thorac Cardiovasc Surg 2008; 136: 962–967. 128 Morey TE, Gravenstein N, Rice MJ. Let’s think clinically instead of mathematically about device accuracy. Anesth Analg 2011; 113: 89–91. 129 Ghanayem NS, Hoffman GM, Mussatto KA et al. Perioperative monitoring in high-risk infants after stage 1 palliation of univentricular congenital heart disease. J Thorac Cardiovasc Surg 2010; 140: 857–863. 130 Tweddell JS, Ghanayem NS, Hoffman GM. Pro: NIRS is “standard of care” for postoperative management. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2010; 13: 44–50. 131 Hoffman GM, Tweddell JS, Ghanayem NS et al. Alteration of the critical arteriovenous oxygen saturation relationship by sustained afterload reduction after the Norwood procedure. J Thorac Cardiovasc Surg 2004; 127: 738–745. 132 Johnson BA, Hoffman GM, Tweddell JS et al. Near-infrared spectroscopy in neonates before palliation of hypoplastic left heart syndrome. Ann Thorac Surg 2009; 87: 571–577; discussion 7-9. 133 Petrova A, Bhatt M, Mehta R. Regional tissue oxygenation in preterm born infants in association with echocardiographically significant patent ductus arteriosus. J Perinatol 2011; 31: 460–464. 134 Li J, Zhang G, Holtby HM et al. Inclusion of oxygen consumption improves the accuracy of arterial and venous oxygen saturation interpretation after the Norwood procedure. J Thorac Cardiovasc Surg 2006; 131: 1099–1107. 135 Li J, Zhang G, Holtby H et al. The influence of systemic hemodynamics and oxygen transport on cerebral oxygen saturation in neonates after the Norwood procedure. J Thorac Cardiovasc Surg 2008; 135: 83–90, e1-2. 136 Tweddell JS, Hoffman GM, Fedderly RT et al. Phenoxybenzamine improves systemic oxygen delivery after the Norwood procedure. Ann Thorac Surg 1999; 67: 161–167; discussion 7-8. 137 Hoffman GM, Ghanayem NS, Kampine JM et al. Venous saturation and the anaerobic threshold in neonates after the Norwood procedure for hypoplastic left heart syndrome. Ann Thorac Surg 2000; 70: 1515– 1520; discussion 21. 138 Tweddell JS, Ghanayem NS, Mussatto KA et al. Mixed venous oxygen saturation mon- © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88 NIRS: exposing the circulatory dark side 139 140 141 142 143 144 145 146 147 148 itoring after stage 1 palliation for hypoplastic left heart syndrome. Ann Thorac Surg 2007; 84: 1301–1310; discussion 10-1. Kaufman J, Almodovar MC, Zuk J et al. Correlation of abdominal site near-infrared spectroscopy with gastric tonometry in infants following surgery for congenital heart disease. Pediatr Crit Care Med 2008; 9: 62–68. Marino BS, Tibby SM, Hoffman GM. Resuscitation of the patient with the functionally univentricular heart. Curr Pediatr Rev 2013; 9: 148–157. Hoffman GM, Ghanayem NS, Berens RJ et al. Reduction in critical indicators of shock by routine use of two-site NIRS in pediatric ICU patients. Anesthesiology 2006; 106: A803. [Internet]. Available at: http:// www.asaabstracts.com/strands/asaabstracts/abstract.htm? year=2006&index=6&absnum=1239. Accessed 5 January, 2011. Hoffman G, Groneck J, Mussatto K et al. Modified pH startegy during antegrade cerebral perfusion improves cerebral hemodynamics. Proceedings of the 2009 Annual Meeting of the American Society Anesthesiologists [Internet]. 2009: A687. Available from: http://www.asaabstracts.com/strands/ asaabstracts/abstract.htm?year=2009& index=16&absnum=2022. Accessed 5 January, 2011. Hoffman GM, Ghanayem NS. Perioperative neuromonitoring in pediatric cardiac surgery: techniques and targets. Prog Pediatr Cardiol 2010; 29: 123–130. Mutch WA, Ryner LN, Kozlowski P et al. Cerebral hypoxia during cardiopulmonary bypass: a magnetic resonance imaging study. Ann Thorac Surg 1997; 64: 695–701. Dent CL, Spaeth JP, Jones BV et al. Brain magnetic resonance imaging abnormalities after the Norwood procedure using regional cerebral perfusion. J Thorac Cardiovasc Surg 2005; 130: 1523–1530. Hoffman GM, Mussatto KA, Brosig CL et al. Perioperative cerebral oxygen saturation in neonates with hypoplastic left heart syndrome and childhood neurodevelopmental outcome. J Thorac Cardiovasc Surg 2013; 146: 1153–1164. Kadoi Y, Kawahara F, Saito S et al. Effects of hypothermic and normothermic cardiopulmonary bypass on brain oxygenation. Ann Thorac Surg 1999; 68: 34–39. Dexter F, Hindman BJ. Theoretical analysis of cerebral venous blood hemoglobin oxygen saturation as an index of cerebral oxygenation during hypothermic cardiopulmonary bypass. A counterproposal to the “luxury perfusion” hypothesis. Anesthesiology 1995; 83: 405–412. 149 Andropoulos DB, Easley RB, Brady K et al. Neurodevelopmental outcomes after regional cerebral perfusion with neuromonitoring for neonatal aortic arch reconstruction. Ann Thorac Surg 2013; 95: 648–654; discussion 54-5. 150 Brady KM, Mytar JO, Lee JK et al. Monitoring cerebral blood flow pressure autoregulation in pediatric patients during cardiac surgery. Stroke 2010; 41: 1957–1962. 151 Brady KM, Lee JK, Kibler KK et al. Continuous measurement of autoregulation by spontaneous fluctuations in cerebral perfusion pressure: comparison of 3 methods. Stroke 2008; 39: 2531–2537. 152 Wypij D, Newburger JW, Rappaport LA et al. The effect of duration of deep hypothermic circulatory arrest in infant heart surgery on late neurodevelopment: the Boston Circulatory Arrest Trial. J Thorac Cardiovasc Surg 2003; 126: 1397– 1403. 153 Greeley WJ, Ungerleider RM, Kern FH et al. Effects of cardiopulmonary bypass on cerebral blood flow in neonates, infants, and children. Circulation 1989; 80: I209– I215. 154 Greeley WJ, Ungerleider RM, Smith LR et al. The effects of deep hypothermic cardiopulmonary bypass and total circulatory arrest on cerebral blood flow in infants and children. J Thorac Cardiovasc Surg 1989; 97: 737–745. 155 Greeley WJ, Kern FH, Meliones JN et al. Effect of deep hypothermia and circulatory arrest on cerebral blood flow and metabolism. Ann Thorac Surg 1993; 56: 1464–1466. 156 Sakamoto T, Zurakowski D, Duebener LF et al. Interaction of temperature with hematocrit level and pH determines safe duration of hypothermic circulatory arrest. J Thorac Cardiovasc Surg 2004; 128: 220– 232. 157 Kussman BD, Wypij D, DiNardo JA et al. Cerebral oximetry during infant cardiac surgery: evaluation and relationship to early postoperative outcome. Anesth Analg 2009; 108: 1122–1131. 158 Sakamoto T, Hatsuoka S, Stock UA et al. Prediction of safe duration of hypothermic circulatory arrest by near-infrared spectroscopy. J Thorac Cardiovasc Surg 2001; 122: 339–350. 159 Chen Y, Liu J, Ji B et al. The optimal flow rate for antegrade cerebral perfusion during deep hypothermic circulatory arrest. Artif Organs 2012; 36: 774–779. 160 Pirzadeh A, Schears G, Pastuszko P et al. Effect of deep hypothermic circulatory arrest followed by low-flow cardiopulmonary bypass on brain metabolism in newborn piglets: comparison of pH-stat and 87 NIRS: exposing the circulatory dark side 161 162 163 164 165 166 167 168 169 170 88 alpha-stat management. Pediatr Crit Care Med 2011; 12: e79–e86. Hofer A, Haizinger B, Geiselseder G et al. Monitoring of selective antegrade cerebral perfusion using near infrared spectroscopy in neonatal aortic arch surgery. Eur J Anaesthesiol 2005; 22: 293–298. Simons J, Sood ED, Derby CD et al. Predictive value of near-infrared spectroscopy on neurodevelopmental outcome after surgery for congenital heart disease in infancy. J Thorac Cardiovasc Surg 2012; 143: 118– 125. Parikh CR, Devarajan P, Zappitelli M et al. Postoperative biomarkers predict acute kidney injury and poor outcomes after pediatric cardiac surgery. J Am Soc Nephrol 2011; 22: 1737–1747. Owens GE, King K, Gurney JG et al. Low renal oximetry correlates with acute kidney injury after infant cardiac surgery. Pediatr Cardiol 2011; 32: 183–188. Hoffman GM, Ghanayem NS, Mussatto KA et al. Perioperative perfusion assessed by somatic NIRS predicts postoperative renal dysfunction. Anesthesiology 2005; 103: A1327. [Internet]. Available at: http://www. asaabstracts.com/strands/asaabstracts/ abstract.htm?year=2005&index=15&absnum=1769. Accessed 5 January, 2011. Hazle MA, Gajarski RJ, Aiyagari R et al. Urinary biomarkers and renal nearinfrared spectroscopy predict intensive care unit outcomes after cardiac surgery in infants younger than six months of age. J Thorac Cardiovasc Surg 2013; 146: 861–867 e1. Stafford-Smith M, Grocott HP. Renal medullary hypoxia during experimental cardiopulmonary bypass: a pilot study. Perfusion 2005; 20: 53–58. Hayes MA, Timmins AC, Yau EH et al. Oxygen transport patterns in patients with sepsis syndrome or septic shock: influence of treatment and relationship to outcome. Crit Care Med 1997; 25: 926–936. Sakr Y, Dubois MJ, De Backer D et al. Persistent microcirculatory alterations are associated with organ failure and death in patients with septic shock. Crit Care Med 2004; 32: 1825–1831. Lima A, van Bommel J, Jansen TC et al. Low tissue oxygen saturation at the end of early goal-directed therapy is associated J.P. Scott and G.M. Hoffman 171 172 173 174 175 176 177 178 179 180 with worse outcome in critically ill patients. Crit Care 2009; 13(Suppl 5): S13. Toet MC, Lemmers PM, van Schelven LJ et al. Cerebral oxygenation and electrical activity after birth asphyxia: their relation to outcome. Pediatrics 2006; 117: 333–339. Soul JS, Hammer PE, Tsuji M et al. Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr Res 2007; 61: 467–473. Tsuji M, Saul JP, du Plessis A et al. Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics 2000; 106: 625–632. Alderliesten T, Lemmers P, Smarius JJ et al. Cerebral oxygenation, extraction, and autoregulation in very preterm infants who develop peri-intraventricular hemorrhage. J Pediatr 2013; 162: 698– 704. e2. Gillam-Krakauer M, Cochran CM, Slaughter JC et al. Correlation of abdominal rSO2 with superior mesenteric artery velocities in preterm infants. J Perinatol 2013; 33: 609– 612. Gay AN, Lazar DA, Stoll B et al. Nearinfrared spectroscopy measurement of abdominal tissue oxygenation is a useful indicator of intestinal blood flow and necrotizing enterocolitis in premature piglets. J Pediatr Surg 2011; 46: 1034–1040. Cortez J, Gupta M, Amaram A et al. Noninvasive evaluation of splanchnic tissue oxygenation using near-infrared spectroscopy in preterm neonates. J Matern Fetal Neonatal Med 2011; 24: 574–582. Fortune PM, Wagstaff M, Petros AJ. Cerebro-splanchnic oxygenation ratio (CSOR) using near infrared spectroscopy may be able to predict splanchnic ischaemia in neonates. Intensive Care Med 2001; 27: 1401–1407. Bailey SM, Hendricks-Mu~ noz KD, Mally P. Splanchnic-cerebral oxygenation ratio as a marker of preterm infant blood transfusion needs. Transfusion 2012; 52: 252–260. van Hoften JC, Verhagen EA, Keating P et al. Cerebral tissue oxygen saturation and extraction in preterm infants before and after blood transfusion. Arch Dis Child Fetal Neonatal Ed 2010; 95: F352–F358. 181 Boost I, Stenson B, Tarnow-Mordi W et al. Oxygen saturation and outcomes in preterm infants. N Engl J Med 2013; 368: 2094. 182 Szabo EZ, Luginbuehl I, Bissonnette B. Impact of anesthetic agents on cerebrovascular physiology in children. Pediatr Anesth 2009; 19: 108–118. 183 Lovell AT, Owen-Reece H, Elwell CE et al. Continuous measurement of cerebral oxygenation by near infrared spectroscopy during induction of anesthesia. Anesth Analg 1999; 88: 554. 184 Bettesworth J, Bhalla T, Barry ND et al. Changes in tissue oxygenation following caudal epidural blockade in infants and children. Pediatr Anesth 2012; 22: 1068– 1071. 185 Tighe P, Elliott C, Lucas S et al. Noninvasive tissue oxygen saturation determined by near-infrared spectroscopy following peripheral nerve block. Acta Anaesthesiol Scand 2011; 55: 1239–1246. 186 Hoffman GM, Ghanayem NS, Musa N et al. Differential effects of carbon dioxide tension on cerebral and somatic oxygenation assessed by near infrared spectroscopy in postoperative neonates. Anesthesiology 2005; 103: A1374. [Internet]. Available at: http://www.asaabstracts.com/strands/asaabstracts/abstract.htm? year=2005&index=15&absnum=1852. Accessed 5 January, 2011. 187 Li J, Zhang G, Holtby H et al. Carbon dioxide–a complex gas in a complex circulation: its effects on systemic hemodynamics and oxygen transport, cerebral, and splanchnic circulation in neonates after the Norwood procedure. J Thorac Cardiovasc Surg 2008; 136: 1207–1214. 188 Germon TJ, Evans PD, Barnett NJ et al. Cerebral near infrared spectroscopy: emitter-detector separation must be increased. Br J Anaesth 1999; 82: 831–837. 189 Madsen PL, Skak C, Rasmussen A et al. Interference of cerebral near-infrared oximetry in patients with icterus. Anesth Analg 2000; 90: 489–493. 190 Song JG, Jeong SM, Shin WJ et al. Laboratory variables associated with low nearinfrared cerebral oxygen saturation in icteric patients before liver transplantation surgery. Anesth Analg 2011; 112: 1347– 1352. © 2013 John Wiley & Sons Ltd Pediatric Anesthesia 24 (2014) 74–88