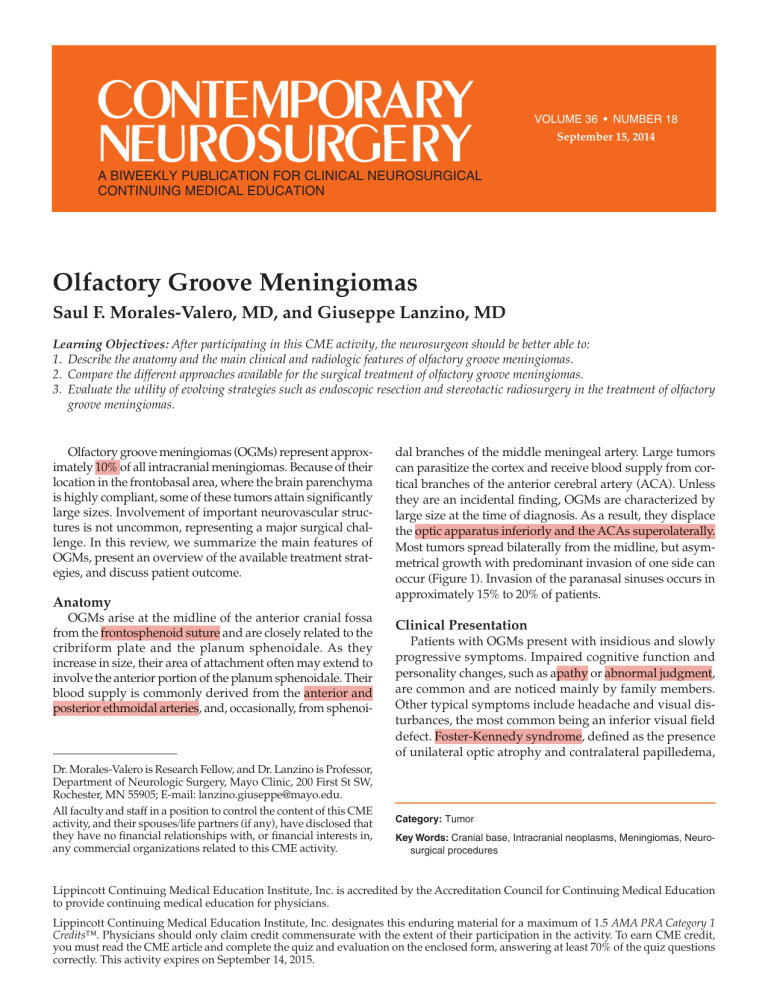
VOLUME VOLUME 36 36 •• NUMBER NUMBER 118 January 31, 2014 September 15, 2014 A BIWEEKLY PUBLICATION FOR CLINICAL NEUROSURGICAL CONTINUING MEDICAL EDUCATION Olfactory Groove Meningiomas Saul F. Morales-Valero, MD, and Giuseppe Lanzino, MD Learning Objectives: After participating in this CME activity, the neurosurgeon should be better able to: 1. Describe the anatomy and the main clinical and radiologic features of olfactory groove meningiomas. 2. Compare the different approaches available for the surgical treatment of olfactory groove meningiomas. 3. Evaluate the utility of evolving strategies such as endoscopic resection and stereotactic radiosurgery in the treatment of olfactory groove meningiomas. Olfactory groove meningiomas (OGMs) represent approximately 10% of all intracranial meningiomas. Because of their location in the frontobasal area, where the brain parenchyma is highly compliant, some of these tumors attain significantly large sizes. Involvement of important neurovascular structures is not uncommon, representing a major surgical challenge. In this review, we summarize the main features of OGMs, present an overview of the available treatment strategies, and discuss patient outcome. Anatomy OGMs arise at the midline of the anterior cranial fossa from the frontosphenoid suture and are closely related to the cribriform plate and the planum sphenoidale. As they increase in size, their area of attachment often may extend to involve the anterior portion of the planum sphenoidale. Their blood supply is commonly derived from the anterior and posterior ethmoidal arteries, and, occasionally, from sphenoi- Dr. Morales-Valero is Research Fellow, and Dr. Lanzino is Professor, Department of Neurologic Surgery, Mayo Clinic, 200 First St SW, Rochester, MN 55905; E-mail: lanzino.giuseppe@mayo.edu. All faculty and staff in a position to control the content of this CME activity, and their spouses/life partners (if any), have disclosed that they have no financial relationships with, or financial interests in, any commercial organizations related to this CME activity. dal branches of the middle meningeal artery. Large tumors can parasitize the cortex and receive blood supply from cortical branches of the anterior cerebral artery (ACA). Unless they are an incidental finding, OGMs are characterized by large size at the time of diagnosis. As a result, they displace the optic apparatus inferiorly and the ACAs superolaterally. Most tumors spread bilaterally from the midline, but asymmetrical growth with predominant invasion of one side can occur (Figure 1). Invasion of the paranasal sinuses occurs in approximately 15% to 20% of patients. Clinical Presentation Patients with OGMs present with insidious and slowly progressive symptoms. Impaired cognitive function and personality changes, such as apathy or abnormal judgment, are common and are noticed mainly by family members. Other typical symptoms include headache and visual disturbances, the most common being an inferior visual field defect. Foster-Kennedy syndrome, defined as the presence of unilateral optic atrophy and contralateral papilledema, Category: Tumor Key Words: Cranial base, Intracranial neoplasms, Meningiomas, Neurosurgical procedures Lippincott Continuing Medical Education Institute, Inc. is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. Lippincott Continuing Medical Education Institute, Inc. designates this enduring material for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should only claim credit commensurate with the extent of their participation in the activity. To earn CME credit, you must read the CME article and complete the quiz and evaluation on the enclosed form, answering at least 70% of the quiz questions correctly. This activity expires on September 14, 2015. Figure 2. Imaging studies in a 43-year-old woman who developed a dull, mid-frontal headache and occasional olfactory hallucinations over a 12-month period. Axial T1-weighted MRI with contrast demonstrated a 3-cm OGM (A). On a T2-weighted, fluid-attenuated inversion recovery sequence, significant peritumoral edema was evident (B). Figure 1. T1-weighted MRI with contrast in a 62-year-old woman who presented with progressive cognitive decline over a 12-month period and frontal headache, worse with Valsalva maneuvers. The axial (A) and coronal (B) views demonstrate the presence of a homogeneously enhancing extra-axial mass arising at the anterior cranial fossa, with predominant growth to the right side of the midline and displacement of the right frontal lobe, consistent with an OGM. The patient underwent successful surgical resection of the tumor. cranial base. Calcifications are observed in 15% to 20% of cases. MRI allows better characterization of the tumor and its relationship to the surrounding neurovascular structures, such as the optic apparatus, ACA, and the anterior communicating artery (AcomA) complex. If present, invasion of the paranasal sinuses can be better defined with MRI, especially in the coronal and sagittal planes. On T1- and T2-weighted sequences, OGMs are revealed as extra-axial masses isointense to gray matter. They exhibit avid and homogeneous enhancement after gadolinium injection. Edema is not uncommon, even in patients with small tumors (Figure 2). is observed in a minority of patients. Impaired olfaction is usually present at the time of diagnosis, but patients are rarely aware of this deficit because of the slow growth rate of most of these tumors. Imaging Both CT and MRI are useful in the evaluation of patients with OGMs. On CT scans, these tumors display the typical characteristics of meningiomas at other locations; they are often rounded, with a broad attachment to the dura mater. OGMs are isodense to the brain parenchyma and reveal homogeneous enhancement with contrast. CT is particularly useful to reveal the hyperostosis, or less commonly the bone destruction, caused by these tumors in the underlying Treatment Surgery Although observation is indicated in asymptomatic patients and elderly patients with small, minimally symptomatic EDITOR: Ali F. Krisht, MD Director, Arkansas Neuroscience Institute Little Rock, Arkansas The continuing education activity in Contemporary Neurosurgery is intended for neurosurgeons, neurologists, neuroradiologists, and neuropathologists. PRODUCTION ASSISTANT: Ronalda Williams by Lippincott Williams & Wilkins, Inc., 16522 Hunters Green Parkway, Hagerstown, MD 21740-2116. Customer Service: Phone (800) 638-3030, Fax (301) 223-2400, or E-mail customerservice@lww.com. Visit our website at www.lww.com. EDITORIAL BOARD: Emad Aboud, MD Tarek Abuelem, MD Ossama Al-Mefty, MD Kenan Arnautovic, MD, PhD Mustafa Baskaya, MD Bernard Bendok, MD Luis A.B. Borba, MD, PhD Ketan R. Bulsara, MD Ruben Dammers, MD, PhD Evandro De Oliveira, MD Samer Elbabaa, MD Giuseppe Lanzino, MD Gerardo Guinto, MD Regis Haid, MD Sanford P.C. Hsu, MD Randy L. Jensen, MD, PhD Paulo A.S. Kadri, MD Niklaus Krayenbühl, MD Jacques J. Morcos, MD Mika Niemelä, MD, PhD Thomas C. Origitano, MD, PhD Vikram C. Prabhu, MD Stylianos Rammos, MD Stephen F. Shafizadeh, MD, PhD Mikael Svensson, MD Uǧur Türe, MD M. Gazi Yaş argil, MD Contemporary Neurosurgery (ISSN 0163-2108) is published bi-weekly Copyright 2014 Lippincott Williams & Wilkins, Inc. All rights reserved. Priority Postage paid at Hagerstown, MD, and at additional mailing offices. POSTMASTER: Send address changes to Contemporary Neurosurgery, Subscription Dept., Lippincott Williams & Wilkins, 16522 Hunters Green Parkway, Hagerstown, MD 21740-2116. Publisher: Randi Davis Subscription rates: Individual: US $716 with CME, $612 with no CME; international $961 with CME, $792 with no CME. Institutional: US $903, international $926. In-training: US resident $139 with no CME, international $162. Single copies: $35. GST Registration Number: 895524239. Send bulk pricing requests to Publisher. COPYING: Contents of Contemporary Neurosurgery are protected by copyright. Reproduction, photocopying, and storage or transmission by magnetic or electronic means are strictly prohibited. Violation of copyright will result in legal action, including civil and/or criminal penalties. Permission to reproduce copies must be secured in writing; at the newsletter website (www.contempneurosurg.com), select the article, and click “Request Permission” under “Article Tools” or e-mail customercare@copyright.com. Reprints: For commercial reprints and all quantities of 500 or more, e-mail reprintsolutions@wolterskluwer.com. For quantities of 500 or under, e-mail reprints@lww.com, call 1-866-903-6951, or fax 1-410-528-4434. PAID SUBSCRIBERS: Current issue and archives (from 1999) are available FREE online at www.contempneurosurg.com. Contemporary Neurosurgery is independent and not affiliated with any organization, vendor, or company. Opinions expressed do not necessarily reflect the views of the Publisher, Editor, or Editorial Board. A mention of products or services does not constitute endorsement. All comments are for general guidance only; professional counsel should be sought for specific situations. Indexed by Bio-Sciences Information Services. For information on CME accreditation, see back page. 2 Figure 3. Illustration of the basic surgical steps for the resection of an OGM as performed from an anterolateral route, including coagulation of the ethmoidal arteries through a transtumoral approach (A), internal debulking of the tumor (B), separation from surrounding structures (C), and removal from the site of attachment (D). tumors, surgical treatment via craniotomy is the mainstay of treatment. A variety of surgical approaches to OGMs has been described. The main route is either anterior (frontal/subfrontal) or anterolateral (pterional and its numerous modifications). Each approach has its advantages and disadvantages. The anterior route provides immediate access to the tumor, with adequate exposure of both sides, and facilitates resection of its superior aspect (often tenaciously adherent to the undersurface of the frontal lobe). Disadvantages of the anterior route include transgression of the frontal sinus; bilateral frontal lobe retraction; need for ligation of the superior sagittal sinus (for a bilateral frontal approach); and limited visualization of the optic apparatus and the ACA/AcomA complex, which is only visualized with this approach toward the late phases of surgery, after extensive internal debulking of the tumor. The lateral and anterolateral routes provide excellent visualization of the tumor/optic apparatus and ACA/AcomA complex, although removal of the upper extent of the tumor can be more laborious compared with a pure anterior route, especially for large-size tumors. Independent of the approach used, during the craniotomy, it is important to plan for possible reconstruction of the cranial base (eg, preparation of a vascularized pericranial flap, harvest of abdominal fat, or fascia lata). Details of the various types of craniotomies used for resection of OGMs are beyond the scope of this article. We schematically describe the basic surgical steps as performed from an anterolateral route, as follows: Devascularization of the tumor. The capsule of the tumor is identified working underneath the arachnoidal plane. The tumor is then entered in the lateral inferior aspect, and the feeders (ethmoidal branches) coming from below are coagulated through a transtumoral approach (Figure 3A). Internal debulking. After the tumor is partially “amputated” and the vascular supply from the ethmoidal arteries interrupted, internal debulking is performed with the aid of the ultrasonic aspirator or with simple suction in soft tumors 3 (Figure 3B). Fast internal debulking is safe, as long as it is done within the boundaries of the tumor, because the important neurovascular structures are situated behind the tumor and beyond the arachnoidal plane. Many OGMs have bilateral extension, and there is often a portion of tumor that extends behind the opposite side of the falx. Therefore, to debulk this portion, the inferior falx is cut, and the crista galli is often rongeured out. Separation from surrounding structures. After extensive internal debulking with preservation of the arachnoidal plane, the tumor is carefully separated from the optic nerves and the AcomA complex by use of high-magnification and microsurgical techniques (Figure 3C). Usually, the arachnoidal plane is well maintained, and its continuity is interrupted only at the point where small branches of the ACA enter the tumor capsule to provide blood supply or relatively large veins “exit” the tumor to join cortical venous drainage pathways. The arachnoidal plane may also be compromised if there is brain invasion. In true OGMs, the optic nerves are usually protected by a relatively thick layer of arachnoid, and they are displaced inferiorly. Small tongues of the tumor might partially extend underneath the nerve, but because the attachment of the tumor is more anterior, these portions can be mobilized easily from the lateral side of the optic nerve while the arachnoidal layer is preserved. In patients with large tumors, a lobe of tumor might extend between the 2 optic nerves anterior to the chiasm, which can be carefully separated and mobilized after internal debulking of the tumor while preserving the arachnoid overlying the optic nerves. The ACA, when in contact with the tumor, also lies behind the arachnoidal plane. It can be identified laterally and then followed medially up to the AcomA complex. Extreme care must be taken during this phase to avoid any potential damage to the medial lenticulostriate arteries or the artery of Heubner. Removal of the superior portion of the tumor. Once the capsule has been separated from the arachnoid protecting the optic nerve and the AcomA complex, the tumor is carefully separated from the undersurface of the frontal lobe. This part of the operation can be, at times, cumbersome from a lateral approach because of the decreased inferosuperior view. Removal of the orbital rim improves the ability to look up from the lateral frontal route, but this maneuver rarely should be necessary. Removal of the tumor from the site of attachment. Once the bulk of the tumor has been removed, attention shifts again to the attachment of the tumor. In a true OGM, this is localized around the area of the olfactory groove, with one side being usually predominant. The attachment is extensively coagulated, and residual fragments of the tumor are removed until the bone of the anterior cranial fossa is visualized (Figure 3D). From a lateral approach, it can be difficult to preserve the ipsilateral olfactory nerve, especially for medium- and largesize tumors, but it is often possible to preserve the contralateral nerve by carefully dissecting it from the contralateral edge of the tumor. In the presence of hyperostosis of the base of attachment, the hyperostotic bone is carefully removed with a diamond drill. At the conclusion of this maneuver, the anterior cranial base is inspected for any potential defect. Various autologous grafts reinforced with fibrin glue can be used to cover or fill any cranial defect. Endoscopic Approaches The endoscopic endonasal approach represents an alternative for surgical treatment in selected patients with OGMs. Its main advantages include its minimally invasive nature and the avoidance of brain retraction. However, compared with open transcranial approaches, the endoscopic approach is associated with lower rates of gross total resection and higher rates of postoperative cerebrospinal fluid (CSF) leak. However, it is possible that with increased Figure 4. Initial and follow-up images (T1-weighted MRI with contrast) of a 50-year-old man who presented with slowly progressive personality changes and cognitive impairment. Initial MRI demonstrated a large, avidly enhancing extra-axial mass consistent with an OGM (A). After surgical resection, an area of plaque-like enhancement was noted at the base of attachment of the tumor and was thought to be a small residual (B). The patient underwent gamma knife surgery, and follow-up imaging after 5 years demonstrates the stable residual tumor (C). 4 an insidious clinical course and are found to have large lesions at the time of the diagnosis. Surgical treatment via an anterior or anterolateral route is the mainstay of treatment in patients with OGMs. Following basic surgical steps in an organized fashion, complete resection can be achieved with minimal morbidity. Alternative treatment options such as endoscopic resection and stereotactic radiosurgery can be considered in carefully selected patients. operator experience, better instrumentation, and improved methods of skull base reconstruction, endoscopic techniques will gain an increased role in the resection of OGMs. Radiosurgery Stereotactic radiosurgery can be considered the primary treatment strategy in the setting of small, incidentally discovered tumors or as an adjuvant modality when complete resection is not feasible (Figure 4). A recent study of 41 patients with OGM treated with stereotactic radiosurgery reported a tumor control rate of 95% after a median follow-up of 65 months and preservation of olfaction in the majority of patients. Readings Bassiouni H, Asgari S, Stolke D. Olfactory groove meningiomas: functional outcome in a series treated microsurgically. Acta Neurochir (Wien). 2007;149:109-121. Gande A, Kano H, Bowden G, et al. Gamma Knife radiosurgery of olfactory groove meningiomas provides a method to preserve subjective olfactory function. J Neurooncol. 2014;116:577-583. Hentschel SJ, DeMonte F. Olfactory groove meningiomas. Neurosurg Focus. 2003;14:e4. Komotar RJ, Starke RM, Raper DM, et al. Endoscopic endonasal versus open transcranial resection of anterior midline skull base meningiomas. World Neurosurg. 2012;77:713-724. Morales-Valero SF, Van Gompel JJ, Loumiotis I, et al. Craniotomy for anterior cranial fossa meningiomas: historical overview. Neurosurg Focus. 2014;36:E14. Nakamura M, Struck M, Roser F, et al. Olfactory groove meningiomas: clinical outcome and recurrence rates after tumor removal through the frontolateral and bifrontal approach. Neurosurgery. 2007;60:844-852. Romani R, Lehecka M, Gaal E, et al. Lateral supraorbital approach applied to olfactory groove meningiomas: experience with 66 consecutive patients. Neurosurgery. 2009;65:39-52. Spektor S, Valarezo J, Fliss DM, et al. Olfactory groove meningiomas from neurosurgical and ear, nose, and throat perspectives: approaches, techniques, and outcomes. Neurosurgery. 2005;57:268-280. Tomasello F, Angileri FF, Grasso G, et al. Giant olfactory groove meningiomas: extent of frontal lobes damage and long-term outcome after the pterional approach. World Neurosurg. 2011;76:311-317. Van Gompel JJ, Frank G, Pasquini E, et al. Expanded endonasal endoscopic resection of anterior fossa meningiomas: report of 13 cases and metaanalysis of the literature. Neurosurg Focus. 2011;30:E15. Outcome The most recent surgical series do not report mortality after surgical resection of OGMs. Among the possible complications seen in the postoperative period, the most common are CSF leak, meningitis, hematoma, and cerebral edema. The rates of CSF leak and meningitis can be minimized by an appropriate cranial base reconstruction, and cerebral edema can be prevented by avoiding significant brain retraction. After successful resection, most patients experience improvement in cognitive function, and personality changes resolve or improve. Visual deficits improve in approximately 80% of cases. In contrast, olfactory function is recovered in a minority of patients, even after anatomic preservation of the olfactory tracts. Tumor recurrence has been documented in approximately 5% of patients and is highly correlated with the initial degree of resection and the histologic characteristics of the tumor. Conclusion OGMs are a specific subset of meningiomas located in the frontobasal area. Patients with OGMs commonly present with Visit www.contempneurosurg.com Your online subscription to Contemporary Neurosurgery offers: • Most popular articles feature • Access to the archive of published issues • e-Pub downloads to access articles on your e-reader device • e-Table of Contents delivered to your inbox • Personalization features, such as saved search results and article collections • CME access To activate your online access, click “Register” at the top right corner of the website. 5 To earn CME credit, you must read the CME article and complete the quiz and evaluation on the enclosed form, answering at least 70% of the quiz questions correctly. Select the best answer and use a blue or black pen to completely fill in the corresponding box on the enclosed answer form. Please indicate any name and address changes directly on the answer form. If your name and address do not appear on the answer form, please print that information in the blank space at the top left of the page. Make a photocopy of the completed answer form for your own files and mail the original answer form in the enclosed postage-paid business reply envelope. Your answer form must be received by Lippincott CME Institute by September 14, 2015. Only two entries will be considered for credit. At the end of each quarter, all CME participants will receive individual issue certificates for their CME participation in that quarter. These individual certificates will include your name, the publication title, the volume number, the issue number, your participation date, and the AMA credit awarded. For more information, call (800) 638-3030. Online quiz instructions: To take the quiz online, log on to your account at http://www.contempneurosurg.com, and click on the “CME” tab at the top of the page. Then click on “Access the CME activity for this newsletter,” which will take you to the log-in page for CME.lwwnewsletters.com. Enter your username and password for this screen as follows: Your CME username will be the letters LWW (case sensitive) followed by the 12-digit account number above your name on the paper answer form mailed with your issue. Your CME password will be 1234; this password may not be changed. Follow the instructions on the site. You may print your official certificate immediately. Please note: Lippincott CME Institute, Inc., will not mail certificates to online participants. The American Association of Neurological Surgeons (AANS) manually tracks AMA PRA Category 1 Credits™ earned from neurosurgery activities not sponsored or joint-sponsored by the AANS. As a service to AANS members, Lippincott CME Institute will continue to provide the AANS a monthly listing of their participants and the CME credits they earned so that AANS members do not have to send their individual certificates to the AANS for tracking. 1. OGMs represent about 10% of all intracranial meningiomas. 6. True or False? 2. True or False? OGMs receive blood supply from the anterior and posterior ethmoidal arteries. 7. True or False? 3. 8. Cognitive impairment, personality changes, and headaches are the most common symptoms in patients with OGMs. Devascularization of the tumor is one of the first steps in successful surgical resection of OGMs. True or False? 9. True or False? 5. Anterior and anterolateral approaches can be used for the surgical resection of OGMs. True or False? Large OGMs displace the optic apparatus superiorly. True or False? 4. OGMs are best evaluated with MRI, which clearly delineates their relationship to surrounding neurovascular structures. Foster-Kennedy syndrome occurs in the majority of patients with OGMs. Resection of OGMs via an endoscopic endonasal approach is associated with lower rates of postoperative CSF leak. True or False? 10. Stereotactic radiosurgery can be used to treat patients with residual and small, incidentally discovered tumors. True or False? True or False? 6