Patch Testing Increases the Likelihood of Recognizing
Anuncio

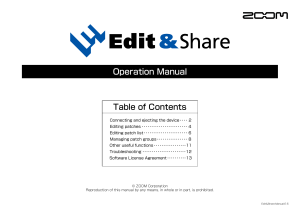
Documento descargado de http://www.elsevier.es el 20/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 64 autoimmune diseases.2 The course of this disease is selflimiting. The lesions resolve within 2 to 4 weeks without residual scarring or recurrence.1 Although its etiology is unknown, the development of this disease is associated with various viral infections, the most common of which is Epstein-Barr virus.1,3-9 The case reported here involved acute ulceration of the vulva (Lipschütz ulcers), associated with primary influenza A virus infection. Because of the high incidence of infection by this virus and the great public alarm regarding the H1N1 serotype, we believe that it is important to study acute ulceration of the vulva and its relationship with influenza A virus infection.10 References 1. Farhi D, Wendling J, Molinari E, Raynal J, Carcelain G, Morand P, et al. Non-sexually related acute genital ulcers in 13 pubertal girls: a clinical and microbiological study. Arch Dermatol. 2009;145:38–45. 2. Fett N, Hinshaw M. Multiple painful vaginal ulcerations. Arch Dermatol. 2008;144:547–52. 3. Martín JM, Molina I, Ramón D, Alpera R, de Frutos E, García L, et al. Úlceras vulvares agudas de Lipschütz. Actas Dermosiiliogr. 2004;95:224–6. 4. Halvorsen JA, Brevig T, Aas T, Skar AG, Slevolden EM, Moi H. Genital ulcers as initial manifestation of Epstein-Barr virus infection: two new cases and a review of the literature. Acta Derm Venereol. 2006;86:439–42. CASE AND RESEARCH LETTERS 5. Barnes CJ, Alio AB, Cunningham BB, Friedlander SF. EpsteinBarr virus associated genital ulcers: an under-recognized disorder. Pediatr Dermatol. 2007;24:130–4. 6. Crawford DH, Swerdlow AJ, Higgins C, McAulay K, Harrison N, William H, et al. Sexual history and Epstein-Barr virus infection. J Infect Dis. 2002;186:731–6. 7. Portnoy J, Ahronheim GA, Ghibu F, Clecner B, Joncas JH. Recovery of Epstein-Barr virus from genital ulcers. N Engl J Med. 1984;311:966–8. 8. Cheng SX, Chapman MS, Margesson LJ, Birenbaum D. Genital ulcers caused by Epstein-Barr virus. J Am Acad Dermatol. 2004;51:824–6. 9. Navarro Ll, Domenech V, Elizalde J, Pujol E. Primoinfección por el virus de Epstein-Barr: una causa poco conocida de úlcera genital aguda. ¿Úcera de Lipschütz? Rev Clin Esp. 1996;196:570– 1. 10. Wetter DA, Bruce AJ, MacLaughlin KL, Rogers III RS. Ulcus vulvae acutum in a 13-year-old girl after inluenza A infection. Skinmed. 2008;7:95–8. A. Esteve-Martínez,* J. López-Davia, A. García-Rabasco, I. Febrer-Bosch, V. Alegre-de Miquel Servicio de Dermat ología, Consorcio Hospit al General Universit ario de Valencia, Valencia, Spain *Corresponding author. E-mail address: alteamarsa@hotmail.com (A. EsteveMartínez). Patch Testing Increases the Likelihood of Recognizing Lamotrigine as a Cause of Drug-Induced Rash La imputabilidad de la lamotrigina en el exantema medicamentoso aumenta con las pruebas epicutáneas To t he Edit or: Lamotrigine, an aromatic antiepileptic drug, is mainly used to manage epilepsy and bipolar disorder and to stabilize mood. The most common adverse reaction to this drug is a skin rash that typically develops in the first 8 weeks of treatment. The patient was a 64-year-old woman with a history of depression. She had been on treatment with ranitidine and venlafaxine for more than 2 years, and was also receiving lamotrigine. She attended the emergency department with a 4-day history of pruritic, erythematous macules and papules that showed cephalocaudal progression (Figures 1 and 2), discomfort in the mouth, and fever of 38ºC. She had been prescribed lamotrigine 12 days before the symptoms commenced. A lamotrigine-induced drug rash was suspected. Treatment was therefore withdrawn and the patient was prescribed Figure 1 Skin symptoms. Documento descargado de http://www.elsevier.es el 20/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. CASE AND RESEARCH LETTERS Figure 2 65 Skin symptoms. Figure 3 prednisone, 0.5 mg/kg/d, and dexchlorpheniramine, 6 mg/8 h. Biopsy was performed in the outpatient clinic 6 days after the onset of the skin rash, and the result was compatible with toxicoderma. The lesions resolved 12 days after starting treatment with the corticosteroids and antihistamines. With a diagnosis of a probable lamotrigine-induced drug reaction, the patient was referred for patch testing, which was performed 5.5 months after the episode resolved. Patches were placed on the upper part of the patient’s back and left for 48 hours. The standard GEIDAC (Spanish Contact Dermatitis Research Group) battery of tests was used: Thin-Layer Rapid Use Epicutaneous Test (Mekos Laboratorios ApS, Denmark) and additional allergens (Chemotechnique Diagnostics, Sweden). The commercial form of lamotrigine tablets (Lamotrigina Merck) was also tested by crushing the tablets and preparing 30% dilutions in water and petroleum jelly. Readings were made at 72 and 168 hours (Figure 3), in accordance with the guidelines of the International Contact Dermatitis Research Group. Positive results were observed for Lamotrigina Merck in water (++) and in petroleum jelly (+) on day 3 and day 6; results were also positive for nickel (++) and palladium (+), but these results were not considered relevant. The patch test results considerably raised the probability that lamotrigine was the cause of the drug reaction in our patient. Lamotrigine-induced drug reactions are generally mild and resolve spontaneously; however, reactions should be monitored closely as they can be life-threatening. Patients are informed that one of the undesirable side Table 1 Patch test results. effects is the possible development of Stevens-Johnson syndrome.1 We frequently encounter skin reactions of this kind in routine clinical practice. It is often difficult to establish the cause, especially in patients receiving multiple treatments.2 Diagnosis must be based on clinical and chronological parameters as there is no standard laboratory test that can determine the origin of this type of reaction. Experts are of the opinion that patch testing of medical products should be performed 2 to 6 months after a reaction. When the commercial form of a drug is used, it should be crushed and prepared in water and in petroleum jelly at a concentration of 30%. Readings should be made at 48 and 96 hours, and if results are negative, again at 7 days.3 We have found only 3 previous articles referring to the use of this type of test in patients with a suspected lamotrigine-induced allergic drug reaction (Table 1). The significance of patch testing in drug-induced reactions is variable, with positive reactions reported in 10% to 50% of cases, depending on the study4,7; however, it is not yet possible to accurately determine the specificity of the test or its negative or positive predictive values. The rate of positive results is affected both by the drug and by the type of clinical reaction. Higher yields are obtained when the following lesions are present: maculopapular rash,5 drug-induced eruption,4,6,8,9 disseminated eczema, systemic contact dermatitis, baboon syndrome (intertriginous drug eruption), and drug reactions with eosinophilia and systemic symptoms (DRESS). Very low yields are obtained in cases Patch test results in the studies reviewed Lamminiausta K Monzón S5 Hesiao CJ6 4 Patients Controls P+ C+ Concentration 5 1 1 5 5 0 0 1 1 0 0 0 30% water and petroleum jelly 10% water and petroleum jelly 50% water and petroleum jelly C+: positive results for controls; P+: positive results for patients. Documento descargado de http://www.elsevier.es el 20/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 66 with urticaria, Stevens-Johnson syndrome, toxic epidermal necrolysis, pruritus, or vasculitis.10 Patch testing with drugs has been demonstrated to be useful in determining the cause of drug-related skin reactions.9,11 The main advantages of patch testing over other diagnostic procedures are that serious adverse reactions are rare and testing can be performed with any commercial form of the drug. Given the absence of a gold standard for determining the causal agent and the importance of reaching a specific diagnosis in these patients, other tests, such as prick, intradermal, and oral challenge tests, should be performed if the results of the patch tests are negative. Conlict of Interest The authors declare they have no conflict of interest. References 1. Francesco G, Cristiana A, Rocco LV, Marinella V, Maurizio E, Antonino R. Hypersensitivity to Lamotrigine and Nonaromatic Anticonvulsant Drugs: A Review. Curr Pharm Des. 2008;14:2874–82. 2. Ghislain PD, Bodarwe AD, Vanderdonckt O, Tennstedt D, Marot L, Lachapelle JM. Drug-induced eosinophilia and multisystemic failure with positive patch-test reaction to spironolactone: DRESS syndrome. Acta Derm Venereol. 2004;84:65–8. 3. Barbaud A, Gonc¸alo M, Bruynzeel D, Bircher A. Guidelines for performing skin tests with drugs in the investigation of cutaneous adverse drug reactions. Contact Dermatitis. 2001;45:321–8. Pregnancy-Related Erythema Annulare Centrifugum Eritema anular centrífugo asociado a gestación To t he Edit or: Erythema annulare centrifugum (EAC) is an uncommon skin disease consisting of annular and polycyclic, erythematous, papular lesions with borders that advance slowly but do not leave scars. Although its etiology remains unknown, the disease has been associated with a range of clinical conditions, including pregnancy.1-3 We describe a new case of EAC associated with pregnancy, provide a review of the relevant literature, and discuss the role of hormones as a possible trigger. A 34-year-old woman in her 28th week of pregnancy and with a history of allergy to tetracyclines consulted for slightly pruritic, annular lesions on the trunk and limbs which had appeared in the 12th week of pregnancy. She said she had not had any recent infections or been exposed CASE AND RESEARCH LETTERS 4. Lamminiausta K, Kortekangas-Savolainen O. The usefulness of skin tests to prove drug hypersensitivity. Br J Dermatol. 2005;152:968–74. 5. Monzón S, Garces MM, Reiehell C, Lezaun A, Colás C. Positive patch test in hypersensitivity to lamotrigine. Contact Dermatitis. 2002;47:361. 6. Hesiao CJ, Lee JY, Wong TW, Sheu HM. Extensive ixed drug eruption due to lamotrigine. Br J Dermatol. 2001;144:1289– 91. 7. Barbaud A. Drug patch testing in systemic cutaneous drug allergy. Toxicology. 2005;209:209–16. 8. Alanko K, Stubb S, Reitamo S. Topical provocation of ixed drug eruption. Br J Dermatol. 1987;116:517–61. 9. Alanko K. Topical provocation of ixed drug eruption. A study of 30 patients. Contact Dermatitis. 1994;31:25–7. 10. Puig L, Nadal C, Fernández-Figueras MT, Alomar A. Carbamazepine-induced drug rashes; diagnostic value of patch test depends on clinico-pathologic presentation. Contact Dermatitis. 1996;34:435–7. 11. Elzagallaai AA, Knowles SR, Rieder MJ, Bend JR, Shear NH, Koren G. Patch Testing for the Diagnosis of Anticonvulsant Hypersensitivity Syndrome. A Systematic Review. Drug Saf. 2009;32:391–408. L. Fuertes,* I. García-Cano, J. Ortiz de Frutos, F. Vanaclocha Servicio de Dermat ología, Hospit al 12 Oct ubre, Madrid, Spain *Corresponding author. E-mail address: laurafdv@hotmail.es (L. Fuertes). to any medications, except for folic acid, which she had been taking since early pregnancy. Physical examination revealed annular erythematous lesions of various sizes, with slightly raised borders, a clear center, without vesiculation, and scaling on the inner margins of the rims; the lesions were located on the thighs, the trunk, and the arms (Figure 1). We requested a biopsy from the advancing border of a lesion to corroborate an initial diagnosis of EAC. Histologically, there was a lymphohistiocytic infiltrate around the superficial vessels with areas of spongiosis and focal parakeratosis. Periodic acid-Schiff staining for fungi was negative (Figure 2). Blood, urine, and serology studies for toxoplasmosis, syphilis, measles, hepatitis B and C, and human immunodeficiency virus were normal. Following confirmation of the suspected diagnosis of EAC, treatment was initiated with methylprednisolone 0.1% cream applied twice daily. However, the lesions did not improve and several new lesions appeared over the course of the pregnancy. Within a few hours of delivery, the lesions started to regress rapidly and had disappeared almost completely 3 days later (Figure 3). Five days after delivery, coinciding with the onset of lactation, the