The prevalence, correlates and treatment of pain in
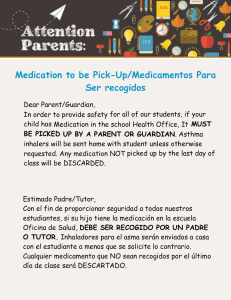
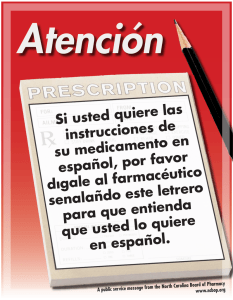
Anuncio

Current Medical Research & Opinion 0300-7995 doi:10.1185/03007995.2010.542136 Vol. 27, No. 2, 2011, 463–480 Article FT-0154.R1/542136 All rights reserved: reproduction in whole or part not permitted P.C. Langley Abstract University of Minnesota, Minneapolis, MN, USA Address for correspondence: Paul C. Langley PhD (for the CHANGE PAIN International Advisory Board), University of Minnesota, 7-159 Weaver-Densford Hall, 308 Harvard St SE, Minneapolis, MN 55455, USA. Tel.: þ1 520 577 0436; Fax: (612) 624-2974; P8366@msn.com Key words: HRQoL – Pain – Prevalence – Severity Accepted: 18 November 2010; published online: 3 January 2011 Citation: Curr Med Res Opin 2011; 27:463–80 CHANGE PAIN International Advisory Board members: K Ahlbeck, Karolinska University Hospital Solna, Stockholm, Sweden D Aldington, Churchill Hospital, Oxford, UK E Alon, Universitätsspital Zurich, Zurich, Switzerland M Berti, A.O. Ospedaliero-Universitaria Parma, Parma, Italy B Collett, University Hospitals of Leicester, Leicester, UK F Coluzzi, Sapienza Università di Roma, Rome, Italy F Huygen, University Hospital Rotterdam, Rotterdam, The Netherlands W Jaksch, Wilhelminenspital der Stadt Wien, Vienna, Austria E Kalso, Helsinki University Central Hospital, Helsinki, Finland M Kocot-Ke˛pska, Poradnia Leczenia Bólu University Hospital, Kraków, Poland A Mangas, Hospital de Santo André, Leiria, Portugal C Margarit, Hospital General Universitario de Alicante, Alicante, Spain P Mavrocordatos, Clinique Cecil, Lausanne, Switzerland B Morlion, University Hospitals Leuven, Pellenberg, Belgium G Müller-Schwefe, Schmerz- und Palliativzentrum Göppingen, Göppingen, Germany A Nicolaou, St Georges Hospital, London, UK C Pérez Hernández, Hospital Universitario de la Princesa, Madrid, Spain J Pergolizzi, School of Medicine, Johns Hopkins University, Baltimore, MD, USA M Schäfer, Campus Virchow Klinikum, Charité Berlin, Berlin P Sichère, Paris, France G Varrassi, Università degli Studi di L’Aquila, L’Aquila, Italy ! 2011 Informa UK Ltd www.cmrojournal.com se oa d, No Cop Un t yr au fo ig th r ht di or S sp ize a la d le © y, us 20 vi e o ew p r 1 r C 1I o an h o n d p ibi m rin ted m fo rm t a . Au e si th rc aU ng or i le is al K co ed D py us is Lim fo ers tr ite rp c i er an bu d so d t na ow io l u nl n Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Original article The prevalence, correlates and treatment of pain in the European Union Objectives: To report on the results of a recent large-scale, internet-based survey of the population, prevalence and attributes of pain experience in the United Kingdom (UK), France, Spain, Germany and Italy. Methods: The results reported here are taken from the internet-based, 2008 National Health and Wellness Survey (NHWS). In addition to detailing the prevalence of pain, the survey reports on the correlates of pain – sociodemographic characteristics of respondents, health status and health related quality of life, pain associated comorbidities, satisfaction with care, employment and productivity and utilization of health care resources. In addition, the survey also captures treatment patterns, satisfaction with medications (both prescription and over the counter [OTC]) and adherence experience. Results: An estimated 49.7 million persons in these five countries reported pain by both its severity and frequency in the previous month. Of these, 11.2 million reported severe pain, 29.4 million reported moderate pain and 9.0 million reported mild pain. The population prevalence of daily pain is 8.85% with 3.47% reporting severe daily pain and 4.70% moderate daily pain. The cumulative burden of pain is demonstrated in terms of HRQoL, employment status and workforce activities as well as in healthcare resource utilization. The most striking impacts are seen in the impact of severe and frequent pain on HRQoL. Of the measures employed, the impact on the physical component score (PCS) of the SF-12 and the SF-6D absolute utility scores are substantial. The presence of severe and daily pain not only reduces the PCS score against that reported for the no pain population by over 20 points (or approximately 40%) but the impact on the absolute utility score is to reduce it from a no pain average of 0.74 to a score of 0.54. As far as productivity losses to the community are concerned the impact of severe pain is equally dramatic. Conclusions: The reported prevalence of pain in these five countries represents a substantial burden to individuals, employers, healthcare systems and society in general. The fact that one in five of the adult population has experienced pain presents a major policy challenge. This would involve not only reducing the prevalence of pain – where chronic pain may be considered a disease in its own right – but to co-ordinate pain management programs across a range of disease states and socio-economic groups. Introduction Comprehensive, pan-European assessments of the prevalence, characteristics, correlates and burden of pain are limited – both in their scope and in the attributes of pain treatment and experience that are captured. With few exceptions, little is known at this level of the societal burden of pain in terms of its impact on HRQoL, workforce status and productivity, and healthcare resource utilization. Even less is known about the characteristics that distinguish those experiencing The prevalence, correlates and treatment of pain Langley 463 Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Current Medical Research & Opinion Volume 27, Number 2 February 2011 pain from those who are not experiencing pain; a distinction that is critical to an assessment of the societal burden. The purpose of this paper is to report, in general terms, on the results of a recent pan-European study of pain in five countries: the UK, France, Spain, Germany and Italy. Data for this study are from the 2008 NHWS1. Until the present study, the most comprehensive assessment of the prevalence, severity, treatment and impact of pain in Europe is from Breivik et al.2. This computer assisted telephone survey covered 15 European countries and Israel. Overall, some 46,934 respondents agreed to participate (a refusal rate of 46%); they had to have suffered from pain for six months or more, experienced pain in the last month and several times in the last week. Respondents were only included if their reported pain intensity was 5 on a 10-point numeric rating scale. In depth interviews with 4839 respondents found 66% reporting moderate pain and the balance reporting severe pain. The study results focused on exploring the demographics of pain, correlates of pain experienced, the impact of defined chronic pain on quality of life and daily activities, understanding current treatment practices and satisfaction with treatment, as well as exploring attitudes towards pain. Another large-scale study of pain in Europe that is worth noting is McDermott et al.3 on the burden of neuropathic pain. This study, with a relatively small convenience sample across six European countries recruited from physician practices, evaluated pain severity, HRQoL, overall health, productivity, non-prescription medication use and frequency of physician visits. Other community pain studies include two by Rustøen et al.4,5, reporting in two papers on the prevalence and characteristics of chronic pain in Norway; Gerdle et al.6, reporting on the prevalence of pain and its impact on work status in Sweden, and the Brattberg et al.7 study of pain prevalence also in Sweden; a study by Bassols et al.8 on pain prevalence in Catalonia, and the prevalence of pain in older adults in Catalonia by Miró et al.9; Smith et al.10 reporting on the community impact of pain in the Grampian region of Scotland; the Eriksen et al.11 study of chronic pain in Denmark; and the more recent German study of chronic pain in primary care by Frießem et al.12. To these would be added the recent pan-European review by Juniper et al.13 of the impact of chronic low back pain. The present study is designed to complement two recently published studies which, using the same data set, have evaluated the impact of the severity and frequency of pain on health related quality of life and healthcare resource utilization14, and employment status, absenteeism and presenteeism15. Outside of the European Union there have been a large number of pain prevalence studies published and some systematic reviews. The most comprehensive studies are those undertaken by national agencies with surveys such as the National Health Interview Survey in the US16. 464 The prevalence, correlates and treatment of pain Langley In the case of systematic reviews a key reference is the Ospina and Harstall17 review of the prevalence of chronic pain in 2002, together with earlier studies, cited by Ospina and Harstall, namely Verhaak et al. in 199818 and Nickel and Raspe in 200119. There was little overlap in the studies selected for these various reviews, reflecting both definitions adopted and the diversity in study design. In the 13 studies selected by Ospina and Harstall it was impossible to come to any consensus on the prevalence of chronic pain with estimates in the range 10.1% to 55.2%. It was possible, however, to come to a consensus view on the prevalence of severe chronic pain with a range from 10% to 13%. Using the IASP definition of chronic pain20, four studies reviewed by Ospina and Harstall yielded an estimate of the weighted mean prevalence of chronic pain at 35.5% (range 11.5% to 55.2%)17. The present study differs in a number of important respects from previous cross-section studies of the prevalence of pain in Europe. First, it focuses on the current experience of pain – pain experienced in the past month. Second, as it is based on a general health status survey, it allows a comparison between those experiencing pain and those not reporting pain in the last month. Third, the study captures two key dimensions of pain: self-reported pain severity and the frequency with which pain has been experienced. Fourth, while the study asks respondents how long they have been taking prescription pain drugs, it does not attempt to impose an arbitrary distinction between chronic and acute pain. Finally, the study focuses on three complementary outcomes of the experience of pain: HRQoL, employment status and workplace productivity, and healthcare resource utilization. The ability to benchmark against those respondents not experiencing pain allows a comprehensive assessment of the individual and societal burden of pain. Methods The purpose of the present analysis is to provide an overview of the results of the 2008 NHWS1 as they relate to the dimensions of pain reported, the prevalence of pain, its correlates and the association between pain and measures of the societal burden of pain. National Health and Wellness Survey The NHWS is an internet based, cross-sectional study of the healthcare attitudes, behaviors, and characteristics of the adult population in the United States, Japan and five European countries1. The survey is designed to be representative of the population 18 years and over in each country. Since its initiation in 1998, over 600,000 survey responses across approximately 140 conditions have been www.cmrojournal.com ! 2011 Informa UK Ltd Current Medical Research & Opinion Volume 27, Number 2 collected. Core reports for each country can be purchased to give bivariate results. Multivariate analyses of results and special supplementary surveys are also available. The present analysis is based on the results of the 2008 NHWS for the European Union. Five countries are included – the UK, France, Italy, Germany and Spain. A total of 53,524 persons 18 years of age and over were interviewed, yielding an age/gender weighted or estimated population of 247.3 million for these five EU countries. Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Dimensions of pain reported The dimensions of pain identified in the NHWS include: Pain experienced in the past month Frequency with which pain is experienced Pain type and associated health status Medication utilization and satisfaction Medication adherence Type of pain medication Duration of pain medication utilization Satisfaction with pain medication Side effects of pain medication Pain experienced in the last month Overall, the 2008 NHWS sample comprised 53,524 respondents. After adjusting to exclude a number of minor or acute pain categories, which were assigned back to the no pain category, a total of 11,891 respondents were identified as reporting pain in the last month. As a weighted population for the five EU countries in the NHWS (247.3 million), a total of 51.8 million reported pain (20.9%) or just over one in five of the population 18 years of age and over. Severe pain was reported by 11.3 million, moderate pain by 29.4 million and mild pain by 9.0 million. An estimated 2.0 million failed to report pain frequency. Note that respondents were asked only to report subjectively assessed ‘severe’, ‘moderate’ and ‘mild pain’; pain scales were not used. Respondents were not asked how long they had experienced pain; rather they were asked how long they had taken specific prescription and/or OTC pain medications. Although there is no unique, clinically based measure of pain, there is a relatively high correlation between self-reported pain status and, for example, pain scales. Frequency of pain experienced Respondents to the NHWS were asked to report the frequency with which they had problems with pain. Options ranged from daily pain to those who experienced pain once a month or less. For the purposes of this analysis the six categories identified in the NHWS have been ! 2011 Informa UK Ltd www.cmrojournal.com February 2011 collapsed to four: ‘daily’, ‘2–4 times a week’, ‘5–6 times a week’, and ‘weekly or less’. These responses can be combined with pain severity to yield ranked combinations from ‘severe pain and daily frequency’ to ‘mild pain’ experience weekly or less. In this study persons only reporting severity of pain (and not frequency of pain) are excluded from the analysis. Pain type and associated health status The NHWS asks respondents reporting pain in the last month which of a list of conditions caused them to feel pain in the last month. These include the most commonly identified causes of pain – back problems, joint pain, neck and migraine – as well as experience of neuropathic pain. At the same time all respondents are also asked which of a number of conditions (n ¼ 34) they have experienced in the last 12 months. These include health states often associated with pain – depression, anxiety, generalized anxiety disorder and sleep difficulties. Medication utilization and satisfaction Respondents were asked if they used prescription or OTC medications to treat their pain. If the response is yes, then for the prescription medications, they are asked to identify from pre-assigned lists for each country in the NHWS the prescription medications they currently use. Pre-assigned lists are not used for OTC medications; respondents are asked to write in the products used. Respondents were also asked, for each of the prescription and OTC medications used, to indicate for how many months/years they had been using prescription medication for pain. As respondents could reply to this question for each medication reported, the responses are collapsed to capture the longest time (in months) that a prescription or OTC medication had been taken. Rather than include the actual number of months, the responses were categorized into those who had taken one or more prescription medications for less than three months and those who had taken medications for three or more months. For each of the prescription and OTC pain medications identified, respondents were asked to indicate how satisfied they were with the product. Responses (seven in all) ranged from ‘extremely dissatisfied’ through ‘neither dissatisfied nor satisfied’ to ‘extremely satisfied’. Although the majority of respondents were on one prescription medication, it was decided to collapse the responses to allow the following categories: Extremely dissatisfied, very dissatisfied or somewhat dissatisfied with all prescription/OTC medications Extremely satisfied, very satisfied or somewhat satisfied with all prescription/OTC medications The prevalence, correlates and treatment of pain Langley 465 Current Medical Research & Opinion Volume 27, Number 2 February 2011 Neither dissatisfied nor satisfied with all prescription/ OTC medications Mixed response for those taking more than one prescription/OTC medication Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Medication adherence Adherence to prescription medications is captured through the application of the Morisky scale21. The four items in the scale focus on barriers to medication taking. The items are: Have you ever forgotten to take your medication? Are you careless at times about taking your medication? When you feel better do you sometimes stop taking your medication? Sometimes if you feel worse when you take the medicine, do you stop taking it? As a ‘yes’ response is scored as one and no is scored as zero, the scale can take values from zero (no ‘yes’ responses) to 4 for the least adherent. These results are presented as averages for the integer valued respondent Morisky score in each of the pain and medication groups. Health related quality of life The instrument selected to measure HRQoL in the NHWS is the SF-12 (version 2)22. The SF-12 is a multipurpose short-form with 12 questions. These questions are all selected from the SF-36 health survey23,24. The SF-12 is a generic measure. A key objective in developing the SF12 in the early 1990 s was to construct the shortest possible form that would replicate the physical and mental health summary scores generated from the SF-36 with at least 90% accuracy. To support this, a further objective was to replicate each of the eight SF-36 health concepts with at least one questionnaire item to set the stage for scoring an eight-scale profile from SF-12 responses. The eight health concepts common to both the SF-36 and SF-12 are: Physical functioning Role physical (accomplishment) Bodily pain General health Vitality (energy level) Social functioning Role emotional (accomplishment) Mental health (feeling) It is worth noting that the SF-12 bodily pain item does not ask respondents to indicate either the severity or the frequency with which pain is experienced. Rather the question asks respondents ‘How much did pain interfere with your normal work (including both work outside the home and housework)’ with the response choice (five items) from ‘not at all’ to ‘extremely’. 466 The prevalence, correlates and treatment of pain Langley While it is possible to develop a health profile utilizing the item responses corresponding to these eight concepts, the focus here is on the two summary scores that can be generated from the respective item responses. These are (i) the physical component summary (PCS) and (ii) the mental component summary (MCS). The former captures the first four elements in the bullet point above, the latter the last four elements. Details of how the links are established and the scoring algorithms are given in Ware et al.22. For the purpose of the present analysis the PCS and MCS summary scores are utilized as normed scores. This is achieved by transforming the raw scores for the items to a mean of 50 and a standard deviation of 10 for the US population. Normed scores can be calculated for both the eight SF-12 scales as well as for the PCS and MCS summary scores. Although country-specific scoring algorithms are available outside the US, the argument has been that it is more appropriate to use a standard scoring algorithm as scores can then be compared across countries. The appropriateness of using the US as a standard benchmark has been demonstrated for nine European countries (including the five countries in the NHWS)22. Given the cross-country nature of the present analysis, the US standard scoring algorithms are used. As well as generating profile and summary PCS and MCS scores, the SF-12 can also be used to generate health state utilities. This is achieved through application of the SF-6D. The SF-6D provides a means for using the SF-36 and SF-12 in economic evaluation by estimating a preference-based single index measure for health from these data using general population values25,26. Any patient who completes the SF-36 or the SF-12 can be uniquely classified according to the SF-6D. The SF-6D describes 18,000 health states in all. It comes with a set of preference weights obtained from a sample of the general population using the recognized valuation technique of standard gamble. The SF-6D allows the analyst to obtain quality adjusted life years (QALYs) from the SF-36 or SF-12 for use in cost utility analysis. The index has interval scoring properties and yields summary scores on a 0–100 scale. The preference weights, which have recently been revised, are those for a UK population27. Labor force participation, absenteeism and presenteeism The NHWS asks individuals to state their current employment status. Four employment status categories are identified, together with job seeking and reasons for not working. In the present analysis a total of five categories are used to assess the impact of pain. These are: Employed full time Employed part time Self-employed www.cmrojournal.com ! 2011 Informa UK Ltd Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Current Medical Research & Opinion Volume 27, Number 2 Unemployed (actively looking for work) Not in the labor force The NHWS uses the Workplace Productivity and Activity Impairment Scale (WPAI)28 to measure the impact of health status on employment related activities. The WPAI questionnaire measures work time missed and work and activity impairment because of a specified health problem during the past 7 days28. The validity and accuracy of the instrument has been established in a number of disease states (e.g., irritable bowel syndrome, asthma, dermatitis, Crohn’s disease)29,30. The WPAI absenteeism and workplace questions are only relevant to those in employment – where the NHWS identifies persons who are currently employed full-time, employed part-time or self-employed. Respondents are asked to indicate: During the past seven days, how many hours did you miss from work because of your health problems? (Range 0 to 112 hours.) During the past seven days, how many hours did you miss from work because of any other reason such as vacation, holidays, time off to participate in this study? (Range 0 to 112 hours.) During the past seven days, how many hours did you actually work? (Range 0 to 112 hours.) During the past seven days how much did your health problems affect your productivity while you were working? (Response on a 0–10 scale from ‘health problems had no effect on work’ to ‘health problems completely prevented me from working’.) During the past seven days, how much did your health problems affect your ability to do your regular daily activities, other than work at a job? (Response on a 0–10 scale from ‘health problems had no effect on my daily activities’ to ‘health problems completely prevented me from doing my daily activities’.) Two measures of employment impact are presented in this analysis. These are: (i) Absenteeism: percentage of work time missed in the past seven days (ii) Presenteeism: percentage of hours worked impacted by impaired productivity February 2011 Provider visits, emergency room visits and hospitalizations The 2008 NHWS also asks respondents about their use of healthcare resources. Resource utilization is considered in terms of visits or events as they relate to: Emergency room visits in the last six months Number of times hospitalized in the last six months Number of visits in the last six months to traditional healthcare providers The number of visits for each type of traditional healthcare provider is also identified, but this level of detail is not considered in the present analysis. Traditional healthcare providers include general practitioner/family practitioner, nurse practitioner/physician assistant as well as medical specialists. Non-traditional or excluded providers include acupuncturist, chiropractor, herbalist, physical therapist, nutritionist, massage therapist and occupational therapist. Results Prevalence, severity and frequency of pain Estimates of the prevalence of pain reported in the previous month by severity and frequency for the five countries are given in Table 1. Overall, out of an estimated total population 18 years of age and over of 245.3 million, an estimated 20.27% (49.7 million) reported both pain severity and the frequency of pain experienced in the last month. Among these 22.47% (11.17 million) report having severe pain and 59.20% (29.42 million) moderate pain. The population prevalence of persons reporting severe pain was 4.61% and moderate pain 12.0%; daily pain was reported by 8.85% of the population. In the severe pain category, the overwhelming majority reported experiencing daily pain (75.16%). This contrasts with only 39.90% in the moderate pain category and 16.12% in the mild pain category. The population prevalence of pain by age, gender, education and household income is detailed in Table 2. The prevalence of pain is greatest in the 40 to 59 year age group. As expected, the population prevalence of pain among Table 1. Population prevalence of pain by severity and frequency, NHWS 2008*. Frequency of pain reported Daily 4–6 times a week 2–3 times a week Weekly or less Total pain population Total big 5 EU population Severe pain (%) Moderate pain (%) Mild pain (%) Total pain population (%) 3.47 0.40 0.30 0.45 4.61 22.47 (11.17 m) 4.79 1.69 2.47 3.06 12.00 59.20 (29.42 m) 0.59 0.32 0.74 2.00 3.66 18.06 (8.98 m) 8.85 2.41 3.51 5.51 20.27 20.27 (49.7 m) *UK, France, Spain, Germany, Italy. Source: NHWS, 2008. ! 2011 Informa UK Ltd www.cmrojournal.com The prevalence, correlates and treatment of pain Langley 467 Current Medical Research & Opinion Volume 27, Number 2 February 2011 Table 2. Pain population prevalence distribution by severity, age, gender, education and household income, NHWS 2008. Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Characteristics Age 18 to 39 years of age 40 to 59 years of age 60 years and over Gender Males Females Education University High school Other Household income Under E20,000 E20,000 to E39,999 E40,000 and above No response Severe pain (%) Moderate pain (%) Mild pain (%) Total pain population (%) 0.87 2.30 1.45 3.42 4.84 3.74 1.57 1.31 0.77 5.86 8.45 5.96 1.58 3.04 4.41 7.59 1.99 1.67 7.98 12.30 0.92 2.23 1.46 2.97 5.90 3.14 1.20 1.84 0.62 5.09 9.97 5.22 1.78 1.46 0.69 0.69 3.95 4.06 2.19 1.80 0.98 1.36 0.87 0.44 6.70 6.89 3.75 2.93 Table 3. Pain population, distribution of severe, moderate and mild pain by age, gender, education and household income, NHWS 2008. Characteristics Severe pain (%) Moderate pain (%) Mild pain (%) Total (%) 14.80 27.16 24.33 58.35 57.29 62.75 26.85 15.55 12.92 100.0 100.0 100.0 19.76 24.71 55.28 61.75 24.97 13.54 100.0 100.0 18.16 22.40 27.94 58.30 59.18 60.12 23.54 18.42 11.95 100.0 100.0 100.0 26.49 21.22 18.38 23.45 58.93 59.02 58.32 61.38 14.57 19.76 23.30 15.17 100.0 100.0 100.0 100.0 Age 18 to 39 years of age 40 to 59 years of age 60 years and over Gender Males Females Education University High school Other Household income Under E20,000 E20,000 to E39,999 E40,000 and above No response Source: NHWS, 2008. Source: NHWS, 2008. females is substantially greater than for males (overall 12.30% vs. 7.98%). The case for mild pain is less clear cut. Persons with university education report a lower prevalence of pain that those with high school education while the prevalence of pain tends to decline with higher household income; notably among those with severe pain. Distribution of pain Within the pain population, the distribution of pain level by age, gender, education and household income is dominated by those reporting moderate pain (Table 3). Within the pain population females report more severe (24.71%) and moderate (61.75%) pain than males. The proportion reporting severe pain increases with lower educational attainment (which is inversely related to mild pain). A similar gradient is found in the case of household income with the percentage reporting severe pain declining the higher the level of income reported. with that pain type, with 25% reporting severe pain and 15% mild pain. In the case of back pain, for example, 60.33% report experiencing it as a moderate pain while 24.53% report it as a severe pain. Associated health status Associated health conditions experienced in the past 12 months by the pain population are detailed in Table 5. Overall, in rank order, the most commonly stated health status categories are headache (63.65%), sleep difficulties (46.55%), abdominal pain (38.15%), insomnia (37.27%) and anxiety (35.97%). At the same time the pain population prevalence of associated health states also shows a relationship with pain severity. The prevalence of depression, for example, is 35.38% for those with severe pain, falling to 19.74% for those with mild pain. A similar pattern is found in respect of sleep difficulties, reported anxiety, generalized anxiety disorder, insomnia and panic disorders. Conditions causing pain Conditions causing pain among the pain population are detailed in Table 4. The categories are not mutually exclusive. The most frequently reported condition causing pain is back pain with almost two-thirds of respondents citing this condition (65.56%). The next most frequently cited condition is joint pain (51.66%) followed by neck pain (32.20%). Among all pain conditions noted, the largest single category is for moderate pain experience, followed by severe pain. That is, approximately 60% of respondents have experienced moderate pain associated 468 The prevalence, correlates and treatment of pain Langley Medication utilization Medication utilization is considered from three perspectives. First, the distribution of reported pain experience by medication class (Table 6); second, the distribution of medication reported within disease severity class (Table 7); and third, the distribution of prescription medication use within disease severity class (Table 8). Medication status is categorized by reported utilization of one or more prescription or OTC pain medications. www.cmrojournal.com ! 2011 Informa UK Ltd Current Medical Research & Opinion Volume 27, Number 2 February 2011 Table 4. Pain population, prevalence of conditions causing pain by pain severity, NHWS 2008. Pain experienced Back pain Joint pain Neck pain Headache Arthritis pain Migraine Dental pain Menstrual pain Sprains or strains Surgery or medical procedure pain Severe pain (%) Moderate pain (%) Mild pain (%) Prevalence of pain experienced in pain population (%) 24.53 25.07 25.01 21.26 32.22 25.15 19.41 15.87 14.92 37.75 60.33 59.73 60.80 60.96 57.97 62.19 62.37 65.44 58.10 51.43 15.15 15.20 14.19 17.78 9.81 12.66 18.22 18.69 26.98 10.82 65.56 51.66 32.20 31.36 17.50 14.34 12.21 22.95 9.55 7.19 Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Source: NHWS, 2008. Table 5. Population prevalence and distribution of health conditions experienced in past 12 months and pain severity, NHWS 2008. Associated health status Severe pain (%) Moderate pain (%) Mild pain (%) Total pain population (%) 64.50 57.57 38.96 47.42 41.96 31.12 34.72 35.38 17.39 14.56 18.69 14.90 16.45 15.97 13.78 15.86 10.45 12.90 12.15 11.84 8.22 8.58 6.83 5.67 4.53 9.43 7.63 3.60 3.27 62.98 44.89 38.34 35.87 34.65 33.60 29.59 22.97 15.12 14.92 14.16 13.53 10.91 10.25 11.02 9.40 9.33 9.08 8.99 7.21 7.49 7.57 5.42 4.86 4.31 3.30 3.48 2.80 2.37 64.76 38.11 36.53 29.07 32.77 31.50 25.98 19.74 16.62 15.21 11.54 13.59 8.58 7.97 8.20 5.37 10.15 7.70 7.92 5.43 7.82 5.17 4.07 5.57 5.88 0.83 2.18 0.90 2.66 63.65 46.55 38.15 37.27 35.97 32.66 30.11 25.21 15.91 14.89 14.72 13.85 11.75 11.14 11.14 10.14 9.73 9.70 9.52 7.95 7.72 7.37 5.50 5.17 4.64 4.25 4.19 2.64 2.63 Headache Sleep difficulties Abdominal pain Insomnia Anxiety Abdominal bloating Migraine Depression Nasal allergies/hayfever Gingivitis Generalized anxiety disorder Diarrhea (frequent) Restless legs syndrome Gastroesophageal reflux disease (GERD) or acid reflux Irritable bowel syndrome Chronic constipation Fungal infections of the skin Asthma Social anxiety disorder Panic disorder Eczema Nail fungus Anemia Phobias Dermatitis Fibromyalgia Post-traumatic stress disorder (PTSD) Gout Attention deficit disorder (ADD) Source: NHWS, 2008. Table 6. Pain population, distribution of pain severity by medication utilization, NHWS 2008. Medication status Only prescription pain medications Only OTC pain medications Prescription and OTC pain medications No pain medication Severe pain (%) Moderate pain (%) Mild pain (%) Total (%) 41.84 10.86 33.01 11.53 52.07 65.02 58.79 59.32 6.08 24.13 8.20 29.15 100.0 100.0 100.0 100.0 Source: NHWS, 2008. ! 2011 Informa UK Ltd www.cmrojournal.com The prevalence, correlates and treatment of pain Langley 469 Current Medical Research & Opinion Volume 27, Number 2 February 2011 Table 7. Pain population, distribution of medication utilization by pain severity, NHWS 2008. Medication status Severe pain (%) Moderate pain (%) Mild pain (%) Total pain population (%) Only prescription pain medications Only OTC pain medications Prescription and OTC pain medications No pain medication Total pain population 53.89 17.31 17.48 11.31 100.0 25.79 39.86 11.97 22.38 100.0 9.89 48.55 5.48 36.09 100.0 29.32 36.30 12.05 22.33 100.0 Source: NHWS, 2008. Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Table 8. Pain population, prescription medication utilization by pain severity NHWS, 2008. Medication status Severe pain (%) Moderate pain (%) Mild pain (%) Total pain population (%) Strong opioids* Weak opioids** Other prescription medication only*** No prescription medication Strong opioids and OTC pain medication* Weak opioids and OTC pain medication** Other prescription and OTC pain medication*** No prescription but used OTC medication Persons with prescription and/or OTC medications 10.96 27.57 15.36 11.31 2.34 7.49 7.65 17.31 100.0 1.11 10.97 13.70 22.38 0.39 3.70 7.89 39.86 100.0 0.47 2.69 6.73 36.09 0.14 1.37 3.96 48.55 100.0 3.24 13.26 12.82 22.33 0.79 4.14 7.13 36.30 100.0 *Includes weak opioids and other prescription medications. **Includes other prescription medications but excludes strong opioids. ***Excludes strong and weak opioids. Source: NHWS, 2008. Persons reporting severe pain tend to focus on either taking only prescription pain medications or combining these with over the counter (OTC) medications. Within the medication groups, 52.07% of those taking only prescription medications were experiencing moderate pain compared to 41.84% for those with severe pain (Table 6). The corresponding figures for those only taking OTC medications are 65.02% and 10.86% respectively. A total of 33.01% of those taking both prescription and OTC medications are in the severe pain group. The distribution of medication utilization within the total pain population clearly favors those only taking OTC medications (36.30%), with 29.32 only taking prescription medications (Table 7). Just over one in five (22.33%) took neither prescription nor OTC pain medications. Turning to the distribution of medications by pain severity category we find of those reporting severe pain 53.89% reported only taking prescription medications, with 17.31% only taking OTC medications. Among those with moderate pain, persons only taking OTC medications predominate (39.86%), with a much higher figure for mild pain (48.55%). Prescription medication utilization by drug class – strong opioids, weak opioids and other prescription medication – is presented as a hierarchy (Table 8). The first 470 The prevalence, correlates and treatment of pain Langley group is persons who report strong opioids including, if reported, weak opioids and other prescription medications. The second group is those who report weak opioid use and, if reported, other prescription medications but no strong opioids. The third group is those who take prescription medications but not strong or weak opioids. These distinctions carry over when OTC medications are added to these three prescription drug categories. Within the pain population only 3.24% report taking strong opioids with possibly weak opioids and other prescription medications; with 10.96% in the severe pain group. Persons who do not report strong opioids but report weak opioids and possibly other prescription medications are 13.26% in the total pain population but 27.57% in the severe pain population. A total of 12.82% report taking non-opioid prescription medications. A total of 36.30% of the pain population report taking only OTC products. This figure is highest in the mild pain category (48.55%) and lowest in the severe pain category (17.31%). Duration of pain medication utilization Table 9 reports the duration of medication utilization by medication utilization status. The medication utilization www.cmrojournal.com ! 2011 Informa UK Ltd Current Medical Research & Opinion Volume 27, Number 2 February 2011 Table 9. Pain population, duration of pain medication utilization by pain severity, NHWS 2008. Medication status Duration of medication utilization Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Strong opioids* Weak opioids** Other prescription medication*** Strong opioids and OTC pain medication* Weak opioids and OTC pain medication** Other prescription and OTC pain medication*** Persons with prescription and/or OTC medications Severe pain (%) Moderate pain (%) Mild pain (%) Under 3 months 3 months or more Under 3 months 3 months or more Under 3 months 3 months or more 7.48 28.75 32.07 2.91 6.52 22.26 100.0 16.36 39.90 20.17 3.33 11.00 9.24 100.0 1.63 17.62 45.11 1.09 7.31 27.25 100.0 3.14 30.72 35.01 1.01 10.15 19.97 100.0 0.00 22.03 37.83 1.32 6.27 32.55 100.0 3.89 16.25 45.43 0.81 9.64 23.97 100.0 *Includes weak opioids and other prescription medications. **Includes other prescription medications but excludes strong opioids. ***Excludes strong and weak opioids. Includes people reporting pain and using a prescription medication because duration was only collected in the NHWS for persons reporting one or more prescription medications. Source: NHWS, 2008. Table 10. Pain population, average Morisky score by pain severity and medication utilization, NHWS 2008. Medication status Strong opioids* Weak opioids** Other prescription medication*** Strong opioids and OTC pain medication* Weak opioids and OTC pain medication** Severe pain Moderate pain Mild pain Total pain population 0.694 0.983 1.193 0.925 1.505 1.323 1.068 1.302 1.813 1.713 0.964 1.063 1.555 0.501 1.656 0.829 1.027 1.296 1.169 1.624 Morisky score takes values from 0 to 4 (where 0 is adherent). *Includes weak opioids and other prescription medications. **Includes other prescription medications but excludes strong opioids. ***Excludes strong and weak opioids. Source: NHWS, 2008. hierarchy is the same as for Table 8. Duration is defined in terms of the longest period reported for any given medication within the medication class and is presented as the percentage of respondents reporting duration of use (but not compliance or adherence) for periods under 3 months and for 3 months or more by pain severity and medication status. For persons with severe pain who report a duration of 3 months or more, 16.36% report a strong opioid with possible weak opioid and other prescription medication use. The corresponding figure for those with a weak opioid (no strong opioid) and other possible prescription medication is 39.90% for a duration of 3 months or more. The corresponding figures for those with moderate pain are 30.72% for weak opioids and 3.24% for strong opioids. Again, for those with severe pain 20.17% report taking other prescription medications for 3 months or more compared to 35.01% for those reporting moderate pain. Prescription medication adherence Morisky scores for prescription adherence by medication status and pain severity are presented in Table 10 for the ! 2011 Informa UK Ltd www.cmrojournal.com same medication hierarchy reported in Tables 8 and 9. These are the average of respondent integer valued scores (range 0–4) across all respondents in the respective cells. The lower the score the greater the adherence. For the total pain population the Morisky scores vary from 0.829 in the case of those using strong opioids to 1.624 in the case of those using weak opioids and OTC pain medications. The greatest adherence reported, a Morisky score of 0.694, is for those with severe pain and utilizing strong opioids (to include weak opioids and other prescription medications). Satisfaction with pain medications Overall, the overwhelming majority of persons taking prescription pain medications report they are satisfied with all medications taken (Table 11). Taking account of the substantial proportion of the pain population who do not take prescription medications (58.63%), 29.63% report being satisfied with all prescription medications. Among those with severe pain, where those not taking prescription medications account for only 28.62% of the The prevalence, correlates and treatment of pain Langley 471 Current Medical Research & Opinion Volume 27, Number 2 February 2011 Table 11. Pain population, satisfaction with prescription and OTC pain medications by pain severity, NHWS 2008. Satisfaction Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Satisfaction with prescription pain medications Satisfied with all prescription pain medication No view on all prescription pain medication Dissatisfaction with all prescription pain medications Other No prescription pain medication Satisfaction with OTC pain medications Satisfied with all OTC pain medication No view on all OTC pain medication Dissatisfaction with all OTC pain medications Other No OTC pain medication Not asked Severe pain (%) Moderate pain (%) Mild pain (%) Total pain population (%) 47.96 7.23 7.4 8.79 28.62 100.0 27.9 3.73 3.28 2.85 62.24 100.0 12.2 1.18 1.14 0.85 84.63 100.0 29.63 4.07 3.83 3.84 58.63 100.0 12.15 2.97 1.48 0.88 28.62 53.89 100.0 9.11 1.33 0.76 0.78 62.24 25.79 100.0 4.82 0.14 0.26 0.26 84.63 9.89 100.0 9.03 1.49 0.83 0.71 58.63 29.32 100.0 Source: NHWS, 2008. severe pain population, 47.96% report being satisfied with all prescription medications. Societal burden of pain Three aspects of the societal burden of pain are considered. These are: Health related quality of life Labor force participation and productivity Healthcare resource utilization HRQoL HRQoL results are presented in Table 12. Estimates for the mental and physical component scores for the SF-12 show a disparity between PCS and MCS measures with the deficit impact of pain substantially greater for the former measure. Against an implicit norm of 50, persons reporting no pain had a PCS of 50.96 (SD 8.42) while those reporting pain had a corresponding score of 44.26 (SD 11.60). Within the pain population persons reporting severe pain have the greatest deficit in PCS (32.03; SD 11.53), followed by those reporting moderate pain (42.27; SD 10.62). Within the severe pain category, those reporting daily pain report a PCS of only 29.220 (SD 10.45). The MCS for the total pain population (44.26, SD 11.60) is substantially below that for the no pain population (50.96; SD 8.42). Even so, MCS by pain severity and frequency categories are not markedly different from each other. The impact of pain on SF-6D health utility scores is most clearly seen in respect of severe pain. Against a no pain group absolute utility of 0.74 (SD 0.13), persons experiencing severe pain have an estimated absolute 472 The prevalence, correlates and treatment of pain Langley utility score of 0.56 (SD 0.12). Corresponding scores for moderate pain are 0.66 (SD 0.12) and mild pain 0.72 (SD 0.12). The impact of frequency is seen most dramatically in the severe pain category. Persons reporting severe daily pain have a utility of 0.54 (SD 0.11) compared to those with moderate daily pain reporting a utility of 0.64 (SD 0.64). Responses to each of the eight SF-12 scales are detailed in Table 13 for each of the pain severity groups and the no pain population. There is a deficit recorded for each scale between the pain and no pain populations. The deficit is greatest for bodily pain and for general health. The deficit pattern is repeated for each level of pain severity; the greater the reported pain severity the greater the deficit for each scale. In the severe pain category, the deficit is greatest for bodily pain (28.71 vs. 49.99 in the no pain group). Labor force participation and productivity The association between labor force participation (LFP) and pain severity is detailed in Table 14. The LFP in the no pain population is 64.46%. The LFP in the pain population is 55.93%, falling to 44.67% in the severe pain group. This decline in LFP occurs for all employed components of LFP but not for the unemployed (i.e., those actively looking for work). Absenteeism and presenteeism Patterns of absenteeism and presenteeism mirror those for labor force participation (Table 15). Rates of absenteeism over the previous week increase along with presenteeism as pain increases in severity. In the case of absenteeism, with www.cmrojournal.com ! 2011 Informa UK Ltd Current Medical Research & Opinion Volume 27, Number 2 February 2011 Table 12. Population health related quality of life: pain severity and frequency by SF-12 mental and physical summary scores and SF-6D utilities, NHWS, 2008. Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Frequency of pain reported SF-12 MCS Once a day 4–6 times a week 2–3 times a week Weekly or less Total pain population SF-12 PCS Once a day 4–6 times a week 2–3 times a week Weekly or less Total pain population SF-6D utilities Once a day 4–6 times a week 2–3 times a week Weekly or less Total pain population Persons not reporting pain MCS PCS SF-6D utilities Severe pain (SD) Moderate pain (SD) Mild pain (SD) Total pain population 41.36 (12.57) 40.63 (11.86) 41.36 (12.19) 44.96 (10.90) 41.65 (12.38) 45.32 (11.85) 44.20 (11.39) 43.74 (11.22) 44.87 (10.62) 44.72 (11.37) 46.71 (11.82) 45.47 (10.96) 44.54 (11.43) 46.43 (10.05) 46.01 (10.75) 43.86 (12.30) 43.78 (11.50) 43.71 (11.38) 45.44 (10.46) 44.26 (11.60) 29.20 (10.45) 35.88 (10.02) 40.09 (9.16) 45.10 (9.37) 32.03 (11.53) 37.56 (10.53) 42.05 (9.99) 43.96 (9.38) 48.41 (8.26) 42.27 (10.62) 45.40 (10.04) 46.27 (8.70) 47.01 (8.88) 50.40 (7.77) 48.54 (8.74) 34.81 (11.56) 41.61 (10.25) 44.28 (9.43) 48.86 (8.31) 41.07 (11.85) 0.54 (0.11) 0.58 (0.10) 0.62 (0.11) 0.67 (0.12) 0.56 (0.12) Score 47.00 (10.64) 50.96 (8.42) 0.74 (0.13) 0.64 (0.12) 0.66 (0.11) 0.67 (0.11) 0.70 (0.11) 0.66 (0.12) 0.72 (0.13) 0.70 (0.12) 0.69 (0.11) 0.73 (0.11) 0.72 (0.12) 0.60 (0.13) 0.65 (0.11) 0.67 (0.11) 0.71 (0.11) 0.65 (0.13) MCS: mental component score; PCS: physical component score; SD: standard deviation. Source: NHWS, 2008. Table 13. Population average scores to SF-12 scales by pain severity, NHWS 2008. SF-12 scale SF12 physical functioning SF12 role physical SF12 bodily pain SF12 general health SF12 vitality SF12 social functioning SF12 role emotional SF12 mental health Severe pain Moderate pain Mild pain Total pain population No pain population Mean SD Mean SD Mean SD Mean SD Mean SD 36.94 34.07 28.71 32.40 41.52 36.20 37.28 40.86 12.19 10.07 10.77 11.44 9.99 11.62 13.92 11.34 45.45 42.24 40.11 40.50 46.27 42.76 42.79 44.98 10.72 9.69 9.87 10.79 9.34 10.58 11.81 10.20 50.24 47.24 46.64 45.84 49.22 45.81 45.07 47.48 9.06 8.95 8.47 9.83 8.94 10.23 11.17 9.47 44.37 41.28 38.69 39.62 45.72 41.82 41.95 44.49 11.67 10.58 11.50 11.64 9.75 11.25 12.51 10.58 51.32 48.72 49.99 47.48 51.51 46.74 45.97 48.82 8.64 8.95 9.18 9.87 9.18 10.31 11.03 9.76 SD: standard deviation. Source: NHWS, 2008. Table 14. Labor force participation by pain severity, NHWS 2008. Labor force status Employed full-time Employed part-time Self-employed Unemployed In the labor force Not in the labor force Severe pain (%) Moderate pain (%) Mild pain (%) Total pain population (%) No pain population (%) 25.98 9.81 3.79 5.08 44.67 55.33 34.44 10.83 5.72 5.15 56.14 43.86 47.39 10.75 7.25 4.05 69.44 30.56 34.85 10.59 5.56 4.93 55.93 44.07 44.52 9.80 6.11 4.03 64.46 35.54 LFP is defined as the number of persons in each labor force category divided by the total population 18 years of age and over. Source: NHWS, 2008. ! 2011 Informa UK Ltd www.cmrojournal.com The prevalence, correlates and treatment of pain Langley 473 Current Medical Research & Opinion Volume 27, Number 2 February 2011 Table 15. Employed population absenteeism and presenteeism by pain severity, NHWS 2008. Average number of hours impacted last week (SD) Absenteeism Presenteeism Severe pain Moderate pain Mild pain No pain population 22.97 (37.10) 37.49 (28.58) 7.77 (22.26) 24.88 (24.90) 4.76 (16.35) 18.71 (22.77) 4.09 (16.11) 13.76 (21.17) Source: NHWS, 2008. Table 16. Population health care utilization: traditional provider visits, emergency room visits, hospitalizations, NHWS 2008. Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Average number of visits past 6 months (SD) Traditional provider visits Emergency room visits Hospitalizations Severe pain Moderate pain Mild pain No pain population 11.83 (12.00) 0.50 (1.47) 0.59 (3.67) 7.82 (8.90) 0.32 (1.33) 0.22 (1.75) 5.51 (6.93) 0.22 (0.67) 0.16 (0.64) 4.39 (6.08) 0.18 (1.03) 0.14 (1.25) Source: NHWS, 2008. the no pain population as the reference point (4.09% absenteeism) those with mild pain report an absenteeism rate of 4.76% climbing to 22.97% for those with severe pain. The corresponding presenteeism estimates increase from 18.71% in the mild pain group to 37.49% in the severe pain group compared to 13.76% in the no pain population. Healthcare resource utilization Healthcare resource utilization is considered in terms of: (i) traditional provider visits; (ii) emergency room visits; and (iii) hospitalizations. Comparing the no pain to the pain population there is a clear demarcation in terms of resource utilization (Table 16). This is most clearly seen in respect of those experiencing severe pain where a substantially higher average number of traditional provider visits (11.83 vs. 4.39), emergency room visits (0.50 vs. 0.18) and hospitalizations (0.59 vs. 0.14) is observed. These differences reduce as pain severity declines. Discussion In the pain population, the most frequently reported conditions causing pain are back pain (65.56%) joint pain (51.66%), neck pain (32.20%) and headache (31.36%) (Table 4). The categories are not mutually exclusive. These results are entirely consistent with previous studies reporting over half the respondents having back pain, some 40% with joint pain and 20% with neck pain. The estimates given here are somewhat higher than those reported by Breivik et al.2, which probably reflects Breivik’s focus on chronic pain. What is of interest to note, however, is that the distribution of the severity of pain reported is similar across all top four pain condition 474 The prevalence, correlates and treatment of pain Langley groups with the majority reporting moderate pain and approximately one in four reporting severe pain. A key distinction between the present survey of pain experience and previous national surveys is in the assessment of the severity, frequency and duration of pain experienced. The present survey is not intended, for example, to focus on chronic pain per se but on the current experience of pain in a representative European population. This includes, by definition, persons who are receiving treatment for their pain condition. In this context, a major objective of the survey is to assess the extent and correlates of the individual and societal burden of pain; i.e., the extent to which current pain experience impacts health related quality of life, workforce status and productivity, and healthcare resource utilization. While this does not mean that the duration and intensity of pain experienced are not potentially important attributes, the focus is on perceived pain severity and its frequency. In the Breivik study, the screening questions exclude all persons who do not meet its definition of chronic pain2: experienced pain for at least six months, had experienced pain in the last month, had experienced pain at least twice a week and rated their pain as at least 5 on a 10-point numeric rating scale. This is, of course, not the only definition of chronic pain found in the literature. Smith et al.10 differentiated ‘any chronic pain’ from ‘significant chronic pain’ and ‘severe chronic pain’ – all of which had a common element of pain duration of at least 3 months. This follows from the IASP definition of chronic pain as ‘ . . . pain which persists past the normal time of healing . . . With nonmalignant pain, three months is the most convenient point of division between acute and chronic pain, but for research purposes six months will often be preferred’’20. A recent study of pain in primary care by Frießem et al. in 200912 defines chronic pain as recurring or constant pain lasting longer than six months. www.cmrojournal.com ! 2011 Informa UK Ltd Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Current Medical Research & Opinion Volume 27, Number 2 A further consideration in avoiding screening questions that arbitrarily differentiate pain groups is the identification of the type of pain experienced and the extent to which respondents suffer from widespread pain and the duration of that pain. This points to the multidimensional nature of pain and further aspects of the societal burden of pain. Gerdle et al.6 report on a population study in Sweden of the prevalence of widespread pain and its impact on work status. They find that widespread pain under the ACR criteria31 gives an overall population prevalence of 4.8% while the Manchester definition32 yields a population prevalence of 7.4%. More recently Von Korff and Dunn33 have argued that the duration approach to the definition of chronic pain is less than optimal. Defining chronic pain solely by duration has not produced reliable or valid methods for the differentiation of chronic from acute pain in either clinical or epidemiological research. The key point is that pain, in particular chronic pain, is multidimensional. Taking a prospective approach to defining chronic pain the authors propose a risk scoring algorithm to predict probabilities of chronic pain 1 to 5 years ahead. A comparison of the risk score with pain days experienced across pain conditions showed less than moderate agreement. The two approaches differed in their profile of chronic pain across pain conditions. Risk score patients, however, with possible and probable chronic pain differed from low-risk patients in both reported intensity and duration. Risk scores had improved predictive power for future severe pain over pain days across all pain conditions assessed. The authors suggest that chronic pain should be defined by the likelihood that the pain will continue into the future, not by duration of pain experience. In the general practitioner setting, however, it might be easier to distinguish chronic pain by duration rather than apply risk scores. While the NHWS does not allow estimation of the proposed Von Korff and Dunn33 risk score, the key point to note is the multidimensional nature of pain and the need to generate an estimate of the likelihood of chronic pain that is consistent across pain conditions. The advantage of the approach taken here in the classification of pain experience is one of flexibility. It allows various profiles of pain experience to be constructed and their impact assessed – as well as the independent contributions of pain frequency and pain severity combinations. For example, if chronic pain is defined as persons experiencing severe or moderate pain at least 4 to 6 times a week then an estimated 10.35% of those 18 years and over in the five EU countries would be classified as experiencing chronic pain. However, if the duration of prescription pain medication utilization is added, where the respondent must have taken at least one branded pain medication for at least 3 months, then this would yield a lower estimate. ! 2011 Informa UK Ltd www.cmrojournal.com February 2011 Rather than attempt to base an analysis of the prevalence and correlates of pain experience on an arbitrary distinction between persons experiencing acute and chronic pain – or on a risk score approach to assess the likelihood of chronic pain – the analysis presented here focuses on reported pain severity and pain frequency and the relationship between the pain and no pain populations in the five EU countries. While the emphasis has been on the correlates of those reporting pain severity, it could be extended to combine pain frequency with pain severity. This is most effectively assessed in the context of multivariate modeling. The potential importance of integrating these two dimensions of current pain experience is seen, first, in the relationship between severity of pain reported (Table 1) and, second, in the relationship between severity and frequency on the distribution of physical and mental summary scores from the SF-12 instrument and on the estimated SF-6D health utilities (Table 12). In the former case, the majority of persons reporting severe pain also report experiencing daily pain. The frequency of pain reported is more diffuse for both the moderate and, in particular, the mild pain groups. In the latter case, there is a clear relationship between the deficits reported for the three health related quality of life measures and the increasing severity and frequency of pain reported. This is seen most dramatically in the SF-12 physical summary scores for persons in the severe pain category. As far as the overall prevalence of pain in these five EU countries is concerned, the NHWS survey finds that one in five of the population experienced pain in the previous month (Table 1). The majority report experiencing moderate pain, a population prevalence of 12.0%, with a population prevalence for severe pain of 4.61%. These estimates are not inconsistent with previous estimates of the population prevalence of pain and estimates of the prevalence of chronic pain. Under the Breivik2 criteria 19% of the population of the 16 countries in their telephone survey reported moderate or severe chronic pain – with a range across the individual countries from 12% to 30%. The overall ratio of severe to moderate pain was 1:2, although (once again) there were significant differences in the relative importance of severe vs. moderate pain between the various countries. Using the IASP definition, however, Ospina and Harstall estimate a mean prevalence of chronic pain of 35.5% (range 55.2% to 11.5%) with a weighted mean prevalence under the ACR definition of 11.8% (range 10.1% to 10.5%)17. Even so, more recent estimates of the population prevalence pain and the prevalence of chronic severe pain point to the disparities than can exist. Gerdle et al.6 in their Swedish population study (age group 18 to 74 years) estimated a population prevalence for those reporting pain in the last week of 63.2%, with 4.8% to 7.4% reporting widespread chronic pain. A feature of the present study which is not found in previous studies is the frequency with which pain is The prevalence, correlates and treatment of pain Langley 475 Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Current Medical Research & Opinion Volume 27, Number 2 February 2011 experienced. While some studies report the experience of constant as opposed to intermittent pain2, the detail provided by the NHWS is not found. In the case of severe pain, some four out of five respondents report severe daily pain, while only two out of five respondents report daily moderate pain. This would qualify attempts to define chronic pain solely in terms of duration. What is of interest in the present study, however, is the apparently low population prevalence of mild pain. As previous studies have focused on moderate and severe pain, notably in respect of chronic pain and neuropathic pain, the experience of mild pain has tended to be overlooked. In McDermott’s study of neuropathic pain report3, using the Brief Pain Inventory score, that most patients reported moderate pain (54%) followed by severe pain (25%) and the balance mild pain. The impact of gender on the reporting and experience of pain has been extensively documented. Pain prevalence studies have consistently shown the impact of gender with women reporting more pain than men, reporting more severe and persistent pain and reporting pain in more body regions. General population studies have shown statistically significant gender differences16, thoracic spine pain34 and with even greater disparities for chronic widespread pain and fibromyalgia35. In the present analysis the difference in pain prevalence and gender is clear-cut both at the population pain prevalence level (Table 2) and within the pain population (Table 3). There is, however, one qualification: the gender difference favoring females only holds for severe and moderate pain; males report more mild pain. Within the pain population females, unlike males, are more likely to report severe and moderate pain. The impact of age on pain is also less clear cut. Rather than a simple gradient where the prevalence of pain across all pain severity categories increases with age, the results (at least for severe and moderate pain) point to the highest prevalence in the 40 to 59 years of age group (Table 2). Indeed, within the pain population, persons 40 to 59 years of age are more likely to report severe pain than the other age groups (Table 3). Although there seems to be a consensus view that there exists a strong social gradient between social status and the experience of pain, notably with educational attainment and household income36,37, the population prevalence results reported here do not support that proposition. At the population prevalence level, the percentage reporting pain is highest in the 40 to 59 years age group (9.97%) and in the intermediate household income (E20,000 to E39,999 group (6.89%). Severe pain is a possible exception. Within the pain population there is no evidence for the likelihood of moderate pain experience being different across income or education groups. Again, severe pain is a possible exception with the frequency reported being inversely related to both education and household income. 476 The prevalence, correlates and treatment of pain Langley It is important to distinguish patient or physician assessed conditions that are associated with self-reported pain from the comorbidities reported by patients experiencing pain. Indeed, the term comorbidity could be extended to include health risk behaviors and even socio-demographic and employment related characteristics – which may map into scales or instruments such as the SF-36. Current and former smokers, for example, have been found to have a higher prevalence or incidence, albeit modest, of low back pain38. While there is a growing literature on the comorbidities or health states that are associated with pain there is no consensus on the principal comorbidities – even when particular pain types of disease states associated with severe or moderate pain are the focus. This reflects, in part, the limitations of patient self reporting, the lack of an agreed classification system for reporting comorbidities and the lack of comprehensive clinical assessment of comorbidities in pain prevalence studies. The NHWS is no exception as respondents are merely asked to report on conditions they have experienced in the last 12 months – without reference to pain (Table 5). As it stands, the conditions reported are somewhat heterogeneous combining both direct pain experience with comorbidities which may or may not be argued to be linked to pain (e.g., nasal allergies/hayfever). Even so, the conditions ranked as having the highest prevalence in the pain population are clearly associated with pain experience – headache, abdominal pain, sleep difficulties, insomnia. At the same time there are a number of high prevalence conditions often associated with the existence of pain – anxiety and depression39 and migraine40. It is worth noting that the population prevalence of anxiety is 35.97% and depression is 25.21% with recent studies pointing to the role of psychosocial factors in amplifying the perception of pain severity, coping adequacy and mediating response41. As these responses are not mutually exclusive, it is of interest to speculate whether or not clinically distinguishable constructs or subgroups of conditions which may have distinct pathophysiological mechanisms of pain generation and response42. Of some note is the relationship between the pain population prevalence of psychiatric disorders with pain severity. As pain increases in severity the prevalence of depression, anxiety, generalized anxiety disorder and panic disorder increases significantly. Patterns of medication utilization point to an increased utilization of prescription pain medications with increased pain severity (Tables 6 and 7). There is little difference in patterns of use for those only reporting prescription medications between those reporting severe or moderate pain. There are, not surprisingly, relatively few respondents with severe pain who are only on OTC products. Even so there is a substantial proportion of respondents with severe pain who reportedly take no pain medications, a proportion that increases with moderate and then mild pain. www.cmrojournal.com ! 2011 Informa UK Ltd Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Current Medical Research & Opinion Volume 27, Number 2 Care has to be taken in interpreting opioid use. In the NHWS survey respondents could choose from pre-selected lists of prescription medications as well as detailing OTC medication utilization. In the results presented here a hierarchy of drug utilization is employed. At the apex are those persons who report strong opioids utilization with the possible addition of weak opioids and other prescription medications. At the next level are those who report weak opioids utilization and possibly other prescription medications but no strong opioids. Given this, it is noteworthy that almost 40% of those with severe pain who report taking prescription and/or OTC medications take at least a strong or a weak opioid; at the same time 17.31% report only taking OTC medications. This contrasts with utilization patterns among those with moderate or mild pain where opioids and other prescription drug use declines substantially, to be overtaken by exclusive non-prescription drug utilization. One feature of duration of medication utilization that stands out is the percentage of respondents who report long term utilization of opioids – in particular the use of weak opioids – in conjunction with other prescription medications (Table 9). Among respondents who have severe pain and who report 3 months or more of medication utilization, 39.90% report taking weak opioids and 16.36% strong opioids (together with other prescription medications). Among the severe pain group relatively few report long term utilization of combinations involving OTC products. Among those with moderate pain, for those with a duration of 3 months or more, sole utilization of prescription medications are still the largest categories. This holds for those reporting mild pain. A recent review by Broekmans et al.43 provides a useful overview of the degree of medication adherence in chronic non-malignant pain. The review found that lack of adherence is common, to include both medication overuse and underuse. A recent Taiwanese study assessed the Morisky score as a measure of adherence in chronic cancer pain where just over 50% of patients were non-adherent44. The results of the present study, in reporting average Morisky scores by medication status and pain severity, paint a somewhat different picture (Table 10). Persons who are experiencing severe pain are consistently more adherent to their medication, whether prescription or OTC, than those who are experiencing only moderate pain. As well, persons who report only strong or weak opioid utilization report consistently higher adherence compared to other pain medication groups, with persons on strong opioids and experiencing severe or moderate pain reporting the highest adherence rates. As Table 9 demonstrates, this adherence is on a relatively long term basis. Clearly, before blanket statements are made as to adherence experience, the potential impact of choice of medication and pain severity needs to be factored into the analysis. ! 2011 Informa UK Ltd www.cmrojournal.com February 2011 The level of satisfaction with pain medications, notably for prescription pain medications, is high (Table 11). Among the severe pain population, 47.96 report being satisfied with all prescription medications taken (with 28.62% not taking prescription pain medications). Ignoring this latter group, this figure translates to 67.19% or two out of three respondents. The impact of neuropathic pain on HRQoL has been the subject of community studies45 and recent reviews45–47. Smith et al. found that those experiencing neuropathic pain in three UK communities recorded significant differences on all dimensions of the SF-36 compared to those reporting no pain45. In reviews by both Jensen and O’Connor neuropathic pain was associated with significant HRQoL deficits in multiple domains – including physical and emotional suffering46,47. Utilizing the EQ-5D instrument as reference point, McDermott et al. point to substantial differences in the deficits associated with levels of pain severity although direct evidence for deficits compared to no pain populations have focused on hypothetical pain free states rather than direct observation. Unfortunately, relatively few of these studies have used a validated generic instrument to assess quality of life3. While Smith et al.10 utilize the SF-36, more recent studies which have taken a broader perspective2,3 have not included a validated instrument. In the present survey, as already noted this is recognized and the SF-12 instrument is used to assess HRQoL. The use of a validated instrument is important because it not only allows comparisons across studies but in the case of the SF-6D health utilities can be estimated. In terms of the scores reported for the SF-12 instrument, the deficit impact of pain is most clearly felt in terms of the PCS (Table 12). While there is a substantial deficit associated with the MCS, there is little variation between the pain severity and frequency categories. This is in contrast to the variability shown for the PCS, with severe daily pain showing the greatest deficit. The differential impact of pain on the PCS and MCS is most readily explained in terms of the components of the scores. The components of the PCS are of interest with the deficit in scores most clearly seen in respect of bodily pain. Even so, it is worth noting again that the SF-12 bodily pain item does not ask respondents to indicate either the severity or the frequency with which pain is experienced. Rather the question asks respondents ‘How much did pain interfere with your normal work (including both work outside the home and housework)’ with the response choice (five items) from ‘not at all’ to ‘extremely’. While depression has often been identified as a key element in the negative impact of pain on HRQoL it does not stand out in this analysis – even for severe pain. As well as evaluating the impact of pain on HRQoL, the present survey also allows an assessment of its impact on employment status and workplace productivity. There is The prevalence, correlates and treatment of pain Langley 477 Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Current Medical Research & Opinion Volume 27, Number 2 February 2011 now an extensive literature on the impact of pain and disability on employment status and the likelihood of returning to work. There are, however, relatively few studies that have considered the relationship between pain severity and factors such as pain duration on labor force status. Those studies that have considered the relationship point to the adverse impact on employment status48,49. In the present study, the presence of both severe and moderate pain is associated with reduced labor force participation (Table 14). Compared to the no pain population, severe pain respondents report an almost 20 point deficit in the percentage in full-time employment. While it is not possible to assign this deficit directly to the experience of pain as there may be other factors contributing to the employment decision, the deficit is clearly substantial and could be interpreted as one of the more significant community burdens associated with the experience of pain. Although the numbers are small, it is worth noting that while the percentage of those employed declines with pain, the percentage actively looking for work increases. The impact of pain on both absenteeism and presenteeism has been considered in a number of studies. These include the Stewart et al. assessment of lost productive time due to common pain conditions – impacting 13% of the US workforce50 – with the major losses due to presenteeism rather than absenteeism; the Roy assessment of the loss of productive time due to pain in the US51; and more recently, for pain associated with particular disease states, the review by Manchikanti et al. of the impact of spinal pain52 and the Sullivan et al. review of the impact of rheumatoid arthritis53. The results of the present study, not surprisingly, support the consensus view on the negative impact of pain on productivity in pointing to the impact of pain on both rates of absenteeism and presenteeism (Table 15). Finally, it should also come as no surprise that the presence of pain negatively impacts health care resource utilization (Table 16). This is seen in traditional provider visits, emergency room visits and hospitalizations. The impact is most pronounced in the severe pain category. Limitations of the analysis The results detailed here are essentially descriptive. In reporting on the key findings for the prevalence, correlates and outcomes associated with the severity and frequency of pain, little can be said as to the underlying causes for the observed patterns or the relative importance of pain severity and frequency, for example, on the HRQoL, workforce status and productivity and healthcare resource utilization. This would require a multivariate analysis that captured possible confounding factors – socio-demographic characteristics, health risk 478 The prevalence, correlates and treatment of pain Langley factors and the presence of comorbidities. Two complementary studies utilizing the same data set have already evaluated the quantitative impact of the severity and frequency of pain on HRQoL and healthcare resource utilization14 and the impact of pain on employment status, absenteeism and presenteeism15. Both point to the dominant impact of pain severity and frequency on these aspects of the burden of pain compared to socioeconomic characteristics, health risk behaviors and comorbidities. Other aspects that could be explored in similar analyses would be the determinants of gender differences in pain reported, the impact of pain prevalence within disease groups, medication utilization patterns and pain severity and frequency, adherence patterns and duration of utilization, and satisfaction with care. Even so, the results presented here point, not only to the pervasive presence of pain in these five EU countries, but to the potential importance of factoring in both pain severity and the frequency of pain experienced in understanding the burden of pain in the community. There are other limitations to this analysis that should be noted. First, the NHWS is an internet based survey and may not be representative of the five EU countries covered in the sample – particularly if there are potential biases in the extent to which internet access is available. Even so, over 50% of the EU population in all countries has internet access. The clear advantage of internet based surveys such as the NHWS is in their flexibility, timeliness and cost in identifying key aspects of the burden of disease – in particular, in the present case, the ability to identify a ‘no-pain’ control group. Given that the NHWS covers some 140 disease areas, it offers a robust vehicle for the analysis of pain. Second, respondents are asked to report their experience of pain. There is no separate clinical confirmation of the presence of pain and reported conditions and attributes that may be associated with pain experience. Third, the study is focused on the experience of pain. It has not been concerned with the broader issue of whether the experience of chronic pain should be considered as a disease in its own right54. If pain is considered as a disease in its own right, the sheer burden of pain would point to the need to evaluate the commitment to national pain management strategies, a need for more education to acquaint stakeholders with the burden of pain and the need to take a global perspective in management strategies. Conclusions The experience of pain – notably moderate and severe pain – is common in the adult population. With over one in five of the estimated 5 country adult population of some 250 million persons reporting having experienced www.cmrojournal.com ! 2011 Informa UK Ltd Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. Current Medical Research & Opinion Volume 27, Number 2 pain in the last month, notably moderate and severe pain, the burden of pain experience is substantial for both the individual and for the community as a whole. The burden imposed comprises not only pain severity, to exclude acute pain presentations associated with migraine, dental pain, menstrual pain and headache, but also the frequency of pain reported. Almost one in two of those experiencing pain, even with the range of pain modalities and treatment options open, report daily severe or moderate pain. Pain experience is dominated by back and joint pain, but with almost one in three also reporting neck pain and headaches ancillary to other pain conditions. Indeed, ancillary headache experience is reported by two out of three respondents. Not surprisingly respondents reporting severe pain also report the highest utilization of prescription pain medications, in particular the use of weak opioids. Overall, respondents are satisfied with their pain medications and are strongly adherent in medication utilization, notably among those experiencing severe pain. The cumulative burden of pain is amply demonstrated in terms of HRQoL, employment status and workforce activities as well as in healthcare resource utilization. Perhaps the most striking impacts are seen in the impact of severe and frequent pain on HRQoL. Of the three measures employed, the impact on the PCS component of the SF-12 and the SF-6D absolute utility scores are substantial. The presence of severe and daily pain not only reduces the PCS against that reported for the no pain population by over 20 points (or approximately 40%) but the impact on the absolute utility score is to reduce it from a no pain average of 0.74 to a score of 0.54. Both imply a substantial pain related clinical deficit. As far as productivity losses to the community are concerned the impact of severe pain is equally dramatic. Labor force participation for the severe pain group is some 20 points lower than for the no pain population while rates of absenteeism and presenteeism are over five time and three times greater respectively than those reported for the no pain population. The fact that one in five of the adult population of these five European countries reports experiencing pain in the past month presents a major challenge for both policies to reduce the incidence and prevalence of chronic pain in the community as well as policies to manage pain populations. Whether pain should be considered a disease in its own right, or managed as part of traditional disease intervention strategies where pain is a significant comorbidity, is an issue which has yet to be resolved. A lack of appreciation of the need to manage pain effectively in the long-term would be a major concern. Even so, the benefits of effective pain prevention and pain management strategies would appear to be substantial. ! 2011 Informa UK Ltd www.cmrojournal.com February 2011 Transparency Declaration of interest This study was supported by Grünenthal GmbH, Aachen, Germany. Declaration of financial/other interests P.C.L. has disclosed that he is a consultant for Kantar Health, a company that undertook this analysis on behalf of Grünenthal. Acknowledgments No assistance in the preparation of this article is to be declared. The author would like to acknowledge comments on earlier drafts from members of the CHANGE PAIN International Advisory Board. References 1. National Health and Wellness Survey. 2008. Available at: http:// chsinternational.com 2. Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life and treatment. Eur J Pain 2006; 10:287-333 3. McDermott AM, Toelle TR, Rowbotham DJ, et al. The burden of neuropathic pain: results from a cross-sectional survey. Eur J Pain 2006;10:127-35 4. Rustøen T, Wahl AK, Hanestad BR, et al. Prevalence and characteristics of chronic pain in the general Norwegian population. Eur J Pain 2004;8:555-65 5. Rustøen T, Wahl AK, Hanestad BR, et al. Age and the experience of chronic pain: differences in health and quality of life among younger, middle-aged, and older adults. Clin J Pain 2005;21:513-23 6. Gerdle B, Björk J, Cöster L, et al. Prevalence of widespread pain and associations with work status: a population study. BMC Musculoskelet 2008; 9:102 7. Brattberg G, Thorslund M, Wikman A. The prevalence of pain in a general population. The results of a postal survey in a county of Sweden. Pain 1989; 37:215-22 8. Bassols A, Bosch F, Campillo M, et al. An epidemiological comparison of pain complaints in the general population of Catalonia (Spain). Pain 1999;83:9-16 9. Miró J, Paredes S, Rull M, et al. Pain in older adults: a prevalence study in the Mediterranean region of Catalonia. Eur J Pain 2007;11:83-92 10. Smith BH, Elliott AM, Chambers A, et al. The impact of chronic pain in the community. Fam Prac 2001;18:292-99 11. Eriksen J, Jensenn MK, Sjogren P, et al. Epidemiology of chronic non-malignant pain in Denmark. Pain 2003;106:221-28 12. Frießem CH, Willweber-Strumpf A, Zenz MW. Chronic pain in primary care. German figures from 1991–2006. BMC Pub Health 2009;9:299 13. Juniper A, Le TK, Mladsi D. The epidemiology, economic burden, and pharmacological treatment of chronic low back pain in France, Germany, Italy, Spain and the UK: a literature based review. Expert Opin Pharmacother 2009;10:2581-92 14. Langley PC, Muller-Schwefe G, Nicolaou A, et al. The societal impact of pain in the European Union: health related quality of life and healthcare resource utilization. J Med Econ 2010;13:1-11 15. Langley PC, Muller-Schwefe G, Nicolaou A, et al. The impact of pain on labour force participation, absenteeism and presenteeism in the European Union. J Med Econ 2010;13:662-72 16. Pleis JR, Lucas JW, Ward BW. Summary health statistics for U.S. adults: National Health Interview Survey, 2008. National Center for Health Statistics. Vital Health Stat 2009;10:242 17. Ospina M, Harstall C. Prevalence of chronic pain: an overview. Alberta Heritage Foundation for Medical Research. Health Technology Assessment The prevalence, correlates and treatment of pain Langley 479 Current Medical Research & Opinion Volume 27, Number 2 18. 19. 20. 21. 22. Curr Med Res Opin Downloaded from informahealthcare.com by 186.84.232.28 on 09/22/14 For personal use only. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 480 February 2011 29, December 2002. Available at: http://ihe.ca/documents/prevalence_chronic_ pain_0.pdf [Last accessed 12 November 2010] Verhaak PFM, Kerssens JJ, Dekker J, et al. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain 1998;77:231-9 Nickel R, Raspe HH. Chronischer Schmerz: Epidemiologie und Inanspruchnahme. Nervenarzt 2001;72:897-906 Mersky H, Bogduk N (eds.) Classification of chronic pain. Seattle Washington WA: IASP Press, 1994 Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986;24:67-74 Ware JE, Kosinski M, Turner-Bowker DM, et al. How to Score the Version 2 of the SF-12 Health Survey (with a Supplement Documenting Version 1). Lincoln RI: Quality Metric, 2002 Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey (SF-12): construction of scales and preliminary tests of reliability and validity. Med Care 1996;32:220-33 Ware JE, Kosinski M, Keller SD. SF-12: How to score the SF-12 physical and mental health summary scales, 3rd edn. Lincoln RI: Quality Metric Inc., 1998 Brazier JE, Roberts JR. The estimation of a preference-based index from the SF-12. Med Care 2004;42:851-59 McCabe C, Brazier JE, Gilks P, et al. Using rank data to estimate health state utility models. J Health Econ 2006;25:418-31 Kharroubi S, Brazier JE, Roberts JR, et al. Modelling SF-6D health state preference data using a nonparametric Bayesian method. J Health Econ 2007;26:597-612 Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 1993; 4:353-65 Reilly MC, Bracco A, Ricci J-F, et al. The validity and accuracy of the Work Productivity and Activity Impairment questionnaire – irritable bowel syndrome version (WPAI:IBS). Aliment Pharmacol Ther 2004;20:459-67 Reilly MC, Gerlier L, Brabant Y, et al. Validity, reliability and responsiveness of the Work Productivity and Activity Impairment questionnaire in Crohn’s disease. Clin Ther 2008;30:393-404 Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the multicenter criteria committee. Arthritis Rheum 1990;33:160-72 Hunt IM, Silman AJ, Benjamin S, et al. The prevalence and associated features of chronic widespread pain in the community using the ‘Manchester’ definition of chronic widespread pain. Rheumatology 1999;38:275-79 Von Korff M, Dunn KM. Chronic pain reconsidered. Pain 2008;138:267-76 Briggs AM, Smith AJ, Straker LM, et al. Thoracic spine pain in the general population: prevalence, incidence and associated factors in children, adolescents and adults. A systematic review. BMC Musculoskelet Disord 2009; 10:77 The prevalence, correlates and treatment of pain Langley 35. Yunus MB. Gender differences in fibromyalgia and other related syndromes. J Gend Specif Med 2002;5:42-7 36. Sturm R, Geresenz CR. Relations of income inequality and family income to chronic medical conditions and mental health disorders: national survey. BMJ 2002;324:1-5 37. Krueger A, Stone A. Assessment of pain: a community-based diary survey in the USA. Lancet 2008;371:1519-25 38. Shiri R, Karppinen J, Leino-Arjas P, et al. The association between smoking and low back pain. Am J Med 2010;123:87.e7-35 39. Castro M, Kraychete D, Daltro C, et al. Comorbid anxiety and depression disorders in patients with chronic pain. Arq Neuropsiquiatr 2009;67:982-5 40. Buse DC, Manack A, Serrano D, et al. Sociodemographic and comorbidity profiles of chronic migraine and episodic migraine sufferers. J Neurol Neurosurg Psychiatry 2010;81:428-32 41. Turk DC, Audette J, Levy RM, et al. Assessment and treatment of psychosocial comorbidities in patients with neuropathic pain. Mayo Clin Proc 2010;85(3 Suppl.):S42-50 42. Rehm SE, Koroschetz J, Gockel U, et al. A cross-sectional survey of 3035 patients with fibromyalgia: subgroups of patients with typical comorbidities and sensory system profiles. Rheumatology (Oxford) 2010;49:1146-52 43. Broekmans S, Dobbels F, Milisen K, et al. Medication adherence in patients with non-malignant pain: is there a problem? Eur J Pain 2009;13:115-23 44. Tzeng J, Chang C, Chang C, et al. Assessing analgesic regimen adherence with the Morisky medication adherence measure for Taiwanese patients with cancer pain. J of Pain Symptom Manag 2008;36:157-66 45. Smith BH, Torrance N, Bennett MI, et al. Health and quality of life associated with chronic pain of predominantly neuropathic origin in the community. Clin J Pain 2007;23:143-9 46. Jensen MP, Chodroff MJ, Dworkin RH. The impact of neuropathic pain on health-related quality of life. Neurology 2007;68:1178-82 47. O’Connor AB. Neuropathic Pain. Pharmacoecon 2009;27:95-112 48. Blyth F. Chronic pain in Australia: a prevalence study. Pain 2001;89:127-34 49. Campolieti M. Disability and the labor force participation of older men in Canada. Labour Economics 2002;9:405-32 50. Stewart WF, Ricci J, Chee E, et al. Lost productive time and cost due to common pain conditions in the US workforce. JAMA 2003;290:2443-54 51. Roy S. Loss of productive time due to pain. JAMA 2004;62:694 52. Manchikanti L, Singh V, Datta S, et al. Comprehensive review of epidemiology, scope and impact of spinal pain. Pain Physician 2009;12:E35-70 53. Sullivan PW, Ghushchyan V, Huang X-Y, et al. Influence of rheumatoid arthritis on employment, function, and productivity in a nationally representative sample in the United States. J Rheumatol 2010;37:385-92 54. Niv D, Devor M. Chronic pain as a disease in its own right. Pain Practice 2004; 4:179-81 www.cmrojournal.com ! 2011 Informa UK Ltd