Charles Bonnet syndrome and the association with dementia
Anuncio
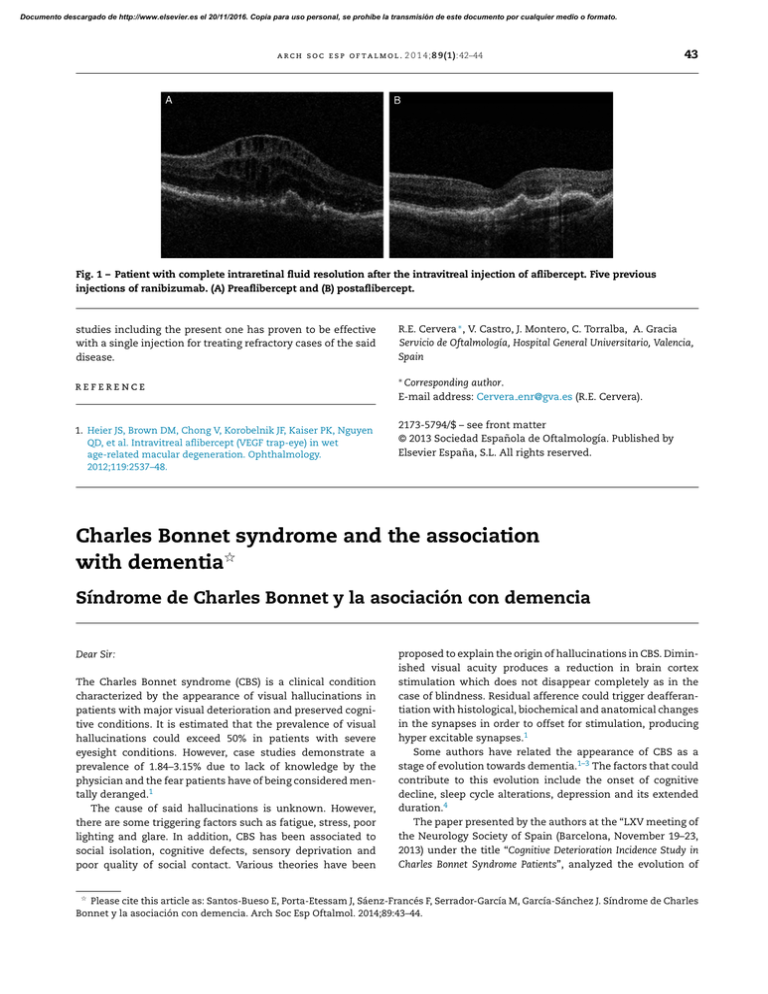
Documento descargado de http://www.elsevier.es el 20/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. a r c h s o c e s p o f t a l m o l . 2 0 1 4;8 9(1):42–44 43 Fig. 1 – Patient with complete intraretinal fluid resolution after the intravitreal injection of aflibercept. Five previous injections of ranibizumab. (A) Preaflibercept and (B) postaflibercept. studies including the present one has proven to be effective with a single injection for treating refractory cases of the said disease. R.E. Cervera ∗ , V. Castro, J. Montero, C. Torralba, A. Gracia Servicio de Oftalmología, Hospital General Universitario, Valencia, Spain reference ∗ Corresponding author. E-mail address: Cervera enr@gva.es (R.E. Cervera). 1. Heier JS, Brown DM, Chong V, Korobelnik JF, Kaiser PK, Nguyen QD, et al. Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology. 2012;119:2537–48. 2173-5794/$ – see front matter © 2013 Sociedad Española de Oftalmología. Published by Elsevier España, S.L. All rights reserved. Charles Bonnet syndrome and the association with dementia夽 Síndrome de Charles Bonnet y la asociación con demencia Dear Sir: The Charles Bonnet syndrome (CBS) is a clinical condition characterized by the appearance of visual hallucinations in patients with major visual deterioration and preserved cognitive conditions. It is estimated that the prevalence of visual hallucinations could exceed 50% in patients with severe eyesight conditions. However, case studies demonstrate a prevalence of 1.84–3.15% due to lack of knowledge by the physician and the fear patients have of being considered mentally deranged.1 The cause of said hallucinations is unknown. However, there are some triggering factors such as fatigue, stress, poor lighting and glare. In addition, CBS has been associated to social isolation, cognitive defects, sensory deprivation and poor quality of social contact. Various theories have been proposed to explain the origin of hallucinations in CBS. Diminished visual acuity produces a reduction in brain cortex stimulation which does not disappear completely as in the case of blindness. Residual afference could trigger deafferantiation with histological, biochemical and anatomical changes in the synapses in order to offset for stimulation, producing hyper excitable synapses.1 Some authors have related the appearance of CBS as a stage of evolution towards dementia.1–3 The factors that could contribute to this evolution include the onset of cognitive decline, sleep cycle alterations, depression and its extended duration.4 The paper presented by the authors at the “LXV meeting of the Neurology Society of Spain (Barcelona, November 19–23, 2013) under the title “Cognitive Deterioration Incidence Study in Charles Bonnet Syndrome Patients”, analyzed the evolution of Please cite this article as: Santos-Bueso E, Porta-Etessam J, Sáenz-Francés F, Serrador-García M, García-Sánchez J. Síndrome de Charles Bonnet y la asociación con demencia. Arch Soc Esp Oftalmol. 2014;89:43–44. 夽 Documento descargado de http://www.elsevier.es el 20/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 44 a r c h s o c e s p o f t a l m o l . 2 0 1 4;8 9(1):42–44 24 diagnosed CBS cases in the Neuroophthalmology Unit of the San Carlos Clinic Hospital of Madrid. The CBS diagnostic was reached by Ophthalmology, Neurology and Psychiatry and was reviewed after one and 2 years with anamnesis, complete exploration and specific neurological tests. Some of the conclusions of said study emphasize that the rate of cognitive decline incidence was 25 times higher than the rate of the Spanish population for the same age range, with statistically significant differences. To conclude, knowledge of CBS and cooperation with Neurology and Psychiatry are of crucial importance to preempt incorrect diagnostics and treatments. Referring patients to these specialties is essential to obtain an early diagnostic of cognitive decline in many of them and prescribe adequate and specific treatments to contribute to substantial improvements in their life quality and expectancy. 2. Guerra-García H. Charles Bonnet syndrome and early dementia. J Am Geriatr Soc. 1997;45:893–4. 3. Terao T, Collinson S. Charles Bonnet syndrome and dementia. Lancet. 2000;355:2168. 4. Fenelon G, Mahleux F, Huon R, Ziegle M. Hallucinations in Parkinson’ disease: prevalence, phenomenology and risk factors. Brain. 2000;123:733–45. E. Santos-Bueso a,∗ , J. Porta-Etessam b , F. Sáenz-Francés a , M. Serrador-García a , J. García-Sánchez a a Unidad de Neurooftalmología, Servicio de Oftalmología, Instituto de Investigación Sanitaria, Hospital Clínico San Carlos (IdISSC), Madrid, Spain b Servicio de Neurología, Hospital Clínico San Carlos, Madrid, Spain ∗ Corresponding reference author. E-mail address: esbueso@hotmail.com (E. Santos-Bueso). 1. Schadlu AP, Schadlu R, Shepherd JB. Charles Bonnet syndrome: a review. Curr Opin Ophthalmol. 2009;20:219–22. 2173-5794/$ – see front matter © 2013 Sociedad Española de Oftalmología. Published by Elsevier España, S.L. All rights reserved.