Sarcoidosis and True Vocal Fold Paresis: 2 Cases and a Review of
Anuncio
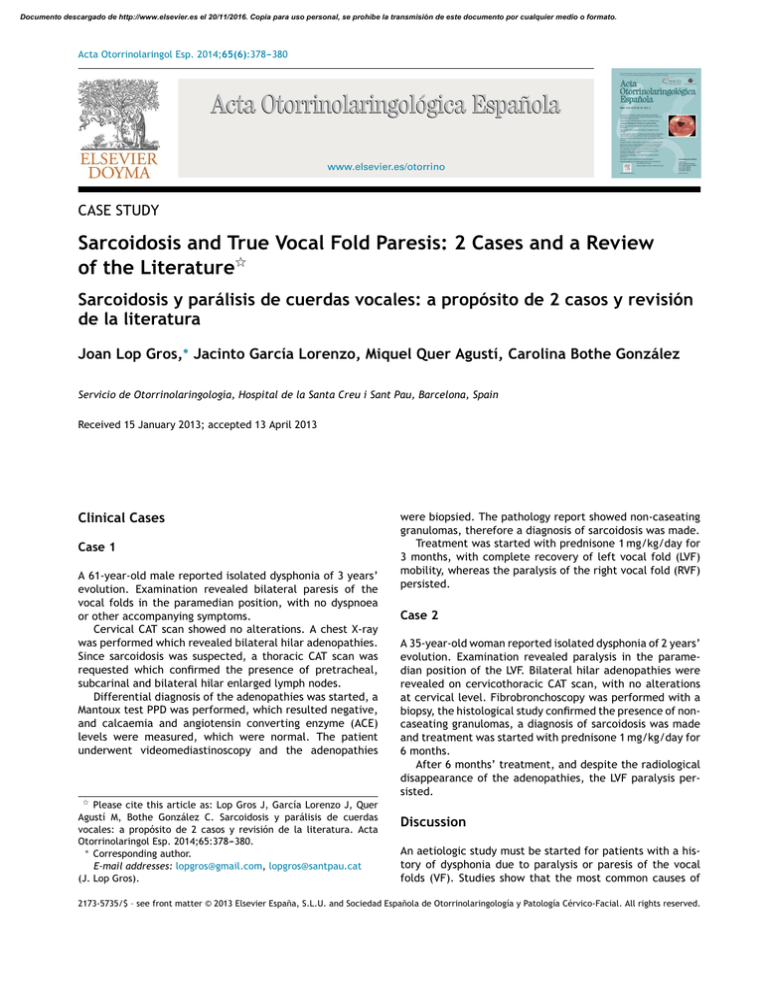
Documento descargado de http://www.elsevier.es el 20/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. Acta Otorrinolaringol Esp. 2014;65(6):378---380 www.elsevier.es/otorrino CASE STUDY Sarcoidosis and True Vocal Fold Paresis: 2 Cases and a Review of the Literature夽 Sarcoidosis y parálisis de cuerdas vocales: a propósito de 2 casos y revisión de la literatura Joan Lop Gros,∗ Jacinto García Lorenzo, Miquel Quer Agustí, Carolina Bothe González Servicio de Otorrinolaringología, Hospital de la Santa Creu i Sant Pau, Barcelona, Spain Received 15 January 2013; accepted 13 April 2013 Clinical Cases Case 1 A 61-year-old male reported isolated dysphonia of 3 years’ evolution. Examination revealed bilateral paresis of the vocal folds in the paramedian position, with no dyspnoea or other accompanying symptoms. Cervical CAT scan showed no alterations. A chest X-ray was performed which revealed bilateral hilar adenopathies. Since sarcoidosis was suspected, a thoracic CAT scan was requested which confirmed the presence of pretracheal, subcarinal and bilateral hilar enlarged lymph nodes. Differential diagnosis of the adenopathies was started, a Mantoux test PPD was performed, which resulted negative, and calcaemia and angiotensin converting enzyme (ACE) levels were measured, which were normal. The patient underwent videomediastinoscopy and the adenopathies 夽 Please cite this article as: Lop Gros J, García Lorenzo J, Quer Agustí M, Bothe González C. Sarcoidosis y parálisis de cuerdas vocales: a propósito de 2 casos y revisión de la literatura. Acta Otorrinolaringol Esp. 2014;65:378---380. ∗ Corresponding author. E-mail addresses: lopgros@gmail.com, lopgros@santpau.cat (J. Lop Gros). were biopsied. The pathology report showed non-caseating granulomas, therefore a diagnosis of sarcoidosis was made. Treatment was started with prednisone 1 mg/kg/day for 3 months, with complete recovery of left vocal fold (LVF) mobility, whereas the paralysis of the right vocal fold (RVF) persisted. Case 2 A 35-year-old woman reported isolated dysphonia of 2 years’ evolution. Examination revealed paralysis in the paramedian position of the LVF. Bilateral hilar adenopathies were revealed on cervicothoracic CAT scan, with no alterations at cervical level. Fibrobronchoscopy was performed with a biopsy, the histological study confirmed the presence of noncaseating granulomas, a diagnosis of sarcoidosis was made and treatment was started with prednisone 1 mg/kg/day for 6 months. After 6 months’ treatment, and despite the radiological disappearance of the adenopathies, the LVF paralysis persisted. Discussion An aetiologic study must be started for patients with a history of dysphonia due to paralysis or paresis of the vocal folds (VF). Studies show that the most common causes of 2173-5735/$ – see front matter © 2013 Elsevier España, S.L.U. and Sociedad Española de Otorrinolaringología y Patología Cérvico-Facial. All rights reserved. Documento descargado de http://www.elsevier.es el 20/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. Sarcoidosis and True Vocal Fold Paresis Table 1 379 Published Cases of Vocal Fold Paralysis Associated With Sarcoidosis. Reference Findings Age, gender Aetiology Treatment Coffey et al. Bilateral VF paralysis bilateral hilar, peritracheal and subcarinal lymphadenopathies Bilateral VF paralysis; mediastinal, peritracheal and apical lymphadenopathies; polyneuritis LVF paralysis; hilar lymphadenopathies 35, male Bilateral compressive lymphadenopathies Methylprednisolone 1 Complete resolution, 2 41, female Cranial polyneuropathy and compressive lymphadenitis Methylprednisolone 36 Complete resolution, 1 Hughes and McGavin Jaffe LVF paralysis; paratracheal, et al. pretracheal and hilar lymphadenopathies Tobias LVF paralysis; right-sided et al. bilateral hilar and paratracheal lymphadenopathies Kassimi LVF paralysis; et al. paratracheal lymphadenopathies Povedano LVF paralysis; bilateral et al. hilar adenopathies 64, female Compressive adenopathy N/A N/A N/A 64, male Compressive lymphadenopathies Prednisone N/A Paralysis persists, 32 49, male Compressive lymphadenopathies Prednisone N/A Complete resolution 45, female Compressive lymphadenopathies Prednisolone 3 53, male Compressive lymphadenopathies Prednisone 4 Lop et al. 61, male Compressive lymphadenopathies Prednisone 150 Complete resolution, 1.5 Complete resolution, 6 Partial resolution, 12 35, female Compressive lymphadenopathies Prednisone 100 Witt Lop et al. Bilateral VF paralysis; bilateral pretracheal, subcarinal and hilar lymphadenopathies LVF paralysis; left paratracheal and bilateral hilar lymphadenopathies Diagnostic delay (weeks) Response, weeks Persists, 24 Source: Modified from Coffey CS, Vallejo SL, Farrar EK, Judson MA, Halstead LA. Sarcoidosis presenting as bilateral vocal fold paralysis from bilateral compression of the recurrent laryngeal nerves from thoracic adenopathy. J Voice. 2009;23:631---4. vocal fold paralysis in adults are endothoracic neoplasias and trauma (iatrogenic or otherwise) to the larynx, these 2 cases constitute more than half the cases of paralysis. However, between 10% and 42% of vocal fold paralyses are considered idiopathic; this is a percentage greater than 3%---17% of which represents the group of ‘‘rare’’ causes (e.g. granulomatous diseases). Paralysis of the left vocal fold is the most common.1 Therefore, aetiologic study of a case of vocal fold paralysis starts by ruling out the presence of endothoracic oncological processes and laryngeal trauma. Once these have been discounted, the rare causes of vocal fold paralysis should be considered, such as neurological, rheumatic, autoimmune or granulomatous disease. Granulomatous diseases are divided into infectious, principally tuberculosis, and non-infectious, beriliosis and sarcoidosis, for example. We perform laboratory tests to make a differential diagnosis; PPD and ACE and calcaemia levels are useful. The diagnosis of sarcoidosis is based on the following criteria: (a) suggestive clinico-radiological features, (b) non-caseating granulomas shown in histology or a positive Kveim/Siltzbach test, (c) the exclusion of other granulomatous diseases and (d) compatible clinical evolution.2 However, the definitive diagnosis will be histopathological. Sarcoidosis is a granulomatous disease of unknown aetiology which can affect any organ. The intra-thoracic region is most commonly affected (80%---90% of cases)3 with hilar, mediastinal lymph node and/or pulmonary infiltration. Granulomas affecting the cervicofacial region in sarcoidosis occur in 9% of cases.4 Although laryngeal involvement can occur primarily due to granulomatous infiltration,4 several cases have been described of paralysis due to compression of the recurrent nerves caused by mediastinal adenopathies.5 Povedano et al.,6 based on the clinical and pathogenic characteristics of described cases of Documento descargado de http://www.elsevier.es el 20/11/2016. Copia para uso personal, se prohíbe la transmisión de este documento por cualquier medio o formato. 380 the disease, suggest 3 mechanisms of paralysis of the vocal folds in the context of sarcoidosis: (1) primary fixation due to granulomas, (2) neuropathy due to primary involvement of the vagus nerve, and (3) neuropathy due to compression of the recurrent nerve secondary to adenopathies. The distinction between these 3 possibilities will be made depending on the findings accompanying the vocal fold paralysis. We opt for the neuropathy group when other cranial nerves are involved, and for the group of primary fixation due to granulomas in the case of sarcoidosis of the larynx itself. Since the laryngeal CAT scans in the 2 cases which we present were normal, and there were no other neurological alterations, we assume that we can include them in the group of paralysis secondary to compressive adenopathy of the recurrent nerve. A great many of the cases published on vocal fold paralysis in the context of sarcoidosis fall into the compression neuropathy group. Coffey et al.5 revised most of the published cases (Table 1) of recurring paralysis in the context of sarcoidosis and found that these were largely left-sided recurrent paralyses; this data is to be expected given the long intra-thoracic route of the left recurrent nerve.7 However, the same authors describe a case of bilateral recurrent paralysis which is justified by the existence of adenopathies at paratracheal level and of the right subclavian artery, where the lower right laryngeal nerve recurs.5 Witt8 and Alon9 also presented cases of bilateral or right-sided recurrent paralysis in sarcoidosis, but these were associated with other cranial neuropathies, and constitute examples of neurosarcoidosis and therefore could be included in group 2 of those proposed by Povedano et al.6 Despite the disparity in laterality, both the unilateral and the bilateral cases showed an excellent response to treatment with corticosteroids, given the reversion of inflammation and lymph node oedema. However, in the cases where introduction of treatment was delayed, J. Lop Gros et al. the response to corticosteroids was reduced.8 This observation is reinforced in the two cases which we present, both share a long evolution time prior to diagnosis (2 years). In conclusion, it is important to include granulomatous diseases in the differential diagnosis of recurrent paralysis. Conflict of Interests The authors have no conflict of interest to declare. References 1. Hillel AT, Samlan RA, Flint PW. Diagnosis and evaluation of laryngeal paralysis and paresis. In: Andrew B, Brin MF, Ramig LO, editors. Neurologic disorders of the larynx. 2nd ed. New York: Thieme Medical Publisher Inc.; 2009. p. 107---15. 2. Baughman RP, Culver DA, Judson MA. A concise review of pulmonary sarcoidosis. Am J Respir Crit Care Med. 2011;183: 573---81. 3. Rey Mañá J. Sarcoidosis. In: Farreras P, Rozman C, editors. Medicina Interna. 15th ed. Elsevier; 2004. p. 1133---6. 4. Dean CM, Sataloff RT, Hawkshaw MJ, Pribitkin E. Laryngeal sarcoidosis. J Voice. 2002;16:283---8. 5. Coffey CS, Vallejo SL, Farrar EK, Judson MA, Halstead LA. Sarcoidosis presenting as bilateral vocal cord paralysis from bilateral compression of the recurrent laryngeal nerves from thoracic adenopathy. J Voice. 2009;23:631---4. 6. Povedano Rodríguez V, Seco Piñero MI, Jaramillo Perez J. Sarcoidosis como causa de parálisis del nervio laríngeo recurrente. Presentación de un caso. An Otorrinolaringol Ibero Am. 1992;19:443---8. 7. Ardito G, Revelli L, D’Alatri L, Lerro V, Guidi ML, Ardito F. Revisited anatomy of the recurrent laryngeal nerves. Am J Surg. 2004;187:249---53. 8. Witt RL. Sarcoidosis presenting as bilateral fold cord paralysis. J Voice. 2003;17:265---8. 9. Alon EE, Ekbom DC. Neurosarcoidosis affecting the vagus nerve. Ann Otol Rhinol Laryngol. 2010;119:641---5.