Sobbing spasm
Anuncio

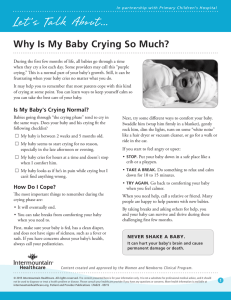
Pediatric criteria Acta Pediátr Mex 2014;35:152-154. Sobbing spasm Matilde Ruíz-García Head of Neurology Service Instituto Nacional de Pediatría Definition Sobbing spasm is the most common non-epileptic paroxystic phenomenon in infants and preschool age children; it is observed in 5 to 7% of infants and preschool age children.1 It is secondary to episodes of acute cerebral hypoxia precipitated by crying, pain, surprise, or frustration. Following a deep inspiration a spasm is produced, which stops respiration and conditions apnea. The patient goes rigid, with cyanosis of lips and fingers and toes, or flaccid and pallid. It often begins between 6 and 12 months of life; in the large majority of cases it disappears before 6 years of age. The greatest frequency occurs between one year and two years of age.2,3 Classification Two types of sobbing spasm are recognized: A. Cyanotic: episodes that begin in the course of crying due to frustration, pain, or anger. After one or several respiratory movements during crying, it is interrupted, the child goes into apnea, and after a few seconds turns cyanotic, and may even lose consciousness. Loss of consciousness may be associated with generalized hypotonia or hypertonia with opisthotonos, and subsequently short seizures. This sequence may be complete or incomplete. In any case, recuperation is immediate. After a few seconds the child regains full wakefulness. The total duration is 1-4 minutes.4,5 Four grades are distinguished: Accepted: March, 2014 Correspondence Grade 2. Crying, prolonged inspiration, apnea and acrocyanosis. Dra. Matilde Ruíz García Jefa del Servicio de Neurología Clínica de Epilepsia del Instituto Nacional de Pediatría matilderuizg@hotmail.com Grade 3. Crying, prolonged inspiration, apnea, cyanosis, and hypotonia or hypertonia. This article must be quoted Ruiz García M. Espasmo del sollozo. Acta Pediat Mex 2014;35:166-169. Grade 1. Crying with prolonged inspiration and brief apnea. 152 Received: February, 2014 www.actapediatricademexico.org Ruiz García M. Sobbing spasm Grade 4. Crying, prolonged inspiration, apnea, cyanosis, hypertonia and generalized clonic seizures. Recommended medical evaluation B. Pallid or reflex anoxic seizure: following minor trauma (especially to the head) or a situation of fear or surprise, the patient starts crying and loses consciousness; the patient is pallid with generalized hypotonia and may also present clonic seizures of extremities. This is due to an increased cardioinhibitory response, secondary to an increase in vagal tone. 2. Physical examination. In some cases, the two forms alternate in the same patient. Some children with pallid spasms will subsequently present infant juvenile syncope as a hypervagotonic reflex reaction to situations of stress.2,3 5. Electrocardiogram in case of pallid sobbing spasm. To rule out arrhythmias or long QT syndrome. C. Mixed. Pallid and cyanotic sobbing spasms may coexist in a patient, although it is uncommon.5 1. Keep calm. Pathophysiology Sobbing spasm has been related to a primitive childhood respiratory reflex; it has a certain degree of family aggregation, because one in every four children with sobbing spasm has a direct family member who suffered it in infancy.6 Some authors have related iron deficiency anemia to the genesis of sobbing spasm and hemoglobin below 8 g/100 mL has been reported in up to 23.5% of children with sobbing spasms. Iron deficiency may play a role in the pathophysiology of sobbing spasm because iron is important for catecholamine metabolism and the functioning of neurotransmitters.7 It has been suggested that a delay in maturation of brainstem myelination, measured through brainstem evoked potentials, may influence the development of sobbing spasm.6,8 1. Complete clinical history. 3. Blood biometry in case of suspected anemia. 4. An electroencephalogram should be performed if epilepsy is suspected, when there is no evident triggering phenomenon, in patients under 6 months or over 6 years of age. Management of sobbing spasm 2. Remove objects the child has in his or her mouth. 3. Place the patient on his or her side and remove any objects with which he or she could hit himself/herself. 4. Maintain a well-ventilated environment, loosen the patient’s clothing. 5. Do not attempt to stop the spasm. 6. Speak softly. 7. When the spasm ends let the patient take a short nap. 8. If the spasm is caused by pain offer consolation and relief. If a child has several sobbing spasms a day behavioral management is probably inappropriate. 153 Volume 35, No. 2, March-April 2014 Acta Pediátrica de México Some children use spasms as an inappropriate form of communication. Some authors recommend the use of piracetam in patients with recurrent sobbing spasm.9 What should be avoided? Antiepileptic treatment is not justified. 1. Resuscitation maneuvers. Long-term follow-up suggests that sobbing spasms are alleviated spontaneously. Patients present a higher incidence of attention problems, and in the case of pallid spasms, may present a higher incidence of syncope.10 2. Striking or bathing the child with cold water. There is a risk of bronchoaspiration and pulmonary complications. 3. Do not place objects in the child’s mouth, as they can cause injury or suffocation. REFERENCES 1. Visser AM, Jaddoe VW, Arends LR, Tiemeier H, Hofman A, Moll HA, Steegers EA, Breteler MM, Arts WF. Paroxysmal disorders in infancy and their risk factors in a populationbased cohort: the Generation R Study. Dev Med Child Neurol 2010;52:1014-20. 2. Martinez A. Chapter 14: Trastornos paroxísticos no epilépticos en los primeros años. En: Campistol J. Neurología para pediatras, enfoque y manejo práctico. Barcelona: Editorial Médica Panamericana, 2011. pp. 191-202. 3. Swaiman KF, Ashwal S, Ferreiro DM. Cap 65. Movement Disorders. In: Pediatric Neurology; Principles and Practice. Philadelphia: Elsevier, 2012. pp. 880-925. 4. Yılmaz Ü, Serdaroğlu A, Gürkaş E, Hirfanoğlu T, Cansu A. Childhood paroxysmal nonepileptic events. Epilepsy and Behavior 2013;27:124-9. 5. Malagon-J Trastornos paroxísticos no epilépticos durante el sueño. Rev Neurol 2013;57(Suppl 1):S115-S123. 6. Vurucu S, Karaoglu A, Paksu SM, Oz O, Yaman H, Gulgun M, Babacan O, Unay B, Akin R. Breath-Holding Spells May be Associated With Maturational Delay in Myelination of Brain Stem. J Clin Neurophysiol. 2014;31:99-101. 7. Fejerman N, Medina CS, Caraballo RN. Trastornos paroxísticos y síntomas episódicos no epilépticos. In: Fejerman N, Fernández Álvarez E. Neurología Pediátrica. Buenos Aires: Editorial Médica Panamericana, 2010. pp. 660-673. 8. There is no specific medication; it is recommended to provide extensive information to the family and use educational strategies for control and inhibition of sobbing spasms. Arslan H, Torun E, Akkan JC, Guler S, Bayraktar S. The Evaluation of Physiological and Biochemical Parameters and the Autonomic Nervous Systems of Children with BreathHolding Spells. Neuropediatrics 2013 Dec 13. [Epub ahead of print] 9. Sawires H, Botrous O. Double-blind, placebo-controlled trial on the effect of piracetam on breath-holding spells. Eur J Pediatr. 2012;171:1063-7. doi: 10.1007/s00431-0121680-1. If iron deficiency anemia is confirmed management with diet and ferrous sulfate is suggested.5,7 10. Olsen AL, Mathiasen R, Rasmussen NH, Knudsen FU. Longterm prognosis for children with breath-holding spells. Dan Med Bull 2010;57:A4217. 4. It is very important not to confuse sobbing spasm with other convulsive disorders; avoid administering antiepileptic drugs as much as possible. When is medical reevaluation needed? 1. When episodes occur without a triggering factor or during sleep. 2. In case of convulsive movements. 3. In case of onset before 5 months or after 6 years of age. 4. When there is diagnostic doubt. The prognosis is good, sobbing spasm is not associated with subsequent development of epilepsy or cognitive alterations. Treatment 154