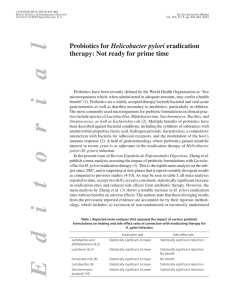
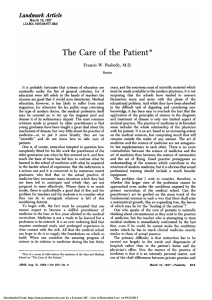
H. pylori Infection, Gastric Cancer and Related Pathologies Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 Helicobacter pylori and Gastric Cancer Jan Bornschein a, b Peter Malfertheiner a a Department of Gastroenterology, Hepatology and Infectious Diseases, Otto von Guericke University of Magdeburg, Magdeburg, Germany; b MRC Cancer Unit, University of Cambridge, Hutchison/MRC Research Centre, Cambridge, UK Abstract Infection with Helicobacter pylori is established as the major risk factor for gastric cancer development. Damage of the mucosal barrier due to H. pylori-induced inflammation enhances the carcinogenic effect of other risk factors such as salt intake or tobacco smoking. The genetic disposition of both the bacterial strain and the host can increase the potential towards gastric cancer formation. Genetic variance of the bacterial proteins CagA and VacA is associated with a higher gastric cancer risk, as are polymorphisms and epigenetic changes in host gene coding for interleukins (IL1β, IL8), transcription factors (CDX2, RUNX3) and DNA repair enzymes. Application of high-throughput assays for genomewide assessment of either genetic structural variance or gene expression patterns may lead to a better understanding of the pathobiological background of these processes, including the underlying signaling pathways. Understanding of the stepwise alterations that take place in the transition from chronic atrophic gastritis, via metaplastic changes, to invasive neoplasia is vital to define the ‘point of no return’ before which eradication of H. pylori has the potential to prevent gastric cancer. Currently, eradication as preventive © 2014 S. Karger AG, Basel 0257–2753/14/0323–0249$39.50/0 E-Mail karger@karger.com www.karger.com/ddi strategy is only recommended for high-incidence regions in Asia; large population studies with an adequate follow-up are required to demonstrate the effectiveness of such an approach in Western populations. © 2014 S. Karger AG, Basel Helicobacter pylori – Epidemiological Background In 1994, the WHO classified Helicobacter pylori as class I carcinogen based on epidemiological evidence for its role in the pathogenesis of gastric cancer, which has been reinforced in 2010 [1, 2]. In 1998, H. pylori was first shown to act as a complete carcinogen, inducing gastric adenocarcinomas without the influence of any cocarcinogens, in a Mongolian gerbil animal model [3, 4]. However, supplementation of the animals with nitrosamines led to higher rates of cancer incidence and a more rapid carcinogenesis suggesting a multifactorial process [5, 6]. The attributable risk of H. pylori infection for gastric carcinogenesis in humans has long been debated. In earlier studies based on H. pylori serology, the odds ratio (OR) for gastric cancer development ranged between 2 and 6 [7]. In a 7.8-years observational study of 1,526 patients who underwent gastroscopy for dyspepsia, gastric adenocarcinoma developed only in 36 patients (2.9%) infected with H. pylori, and not in noninProf. Dr. med. Dr. h. c. mult. Peter Malfertheiner Department of Gastroenterology, Hepatology and Infectious Diseases Otto von Guericke University of Magdeburg Leipziger Strasse 44, DE–39120 Magdeburg (Germany) E-Mail peter.malfertheiner @ med.ovgu.de Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM Key Words Gastric cancer · Gastritis · Helicobacter pylori · Interleukin-1β · Intestinal metaplasia · CagA protein 250 Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 H. pylori and Environmental Risk Factors In 1997, a combined analysis of 16 case-control studies demonstrated an association between salt intake and the risk of gastric cancer [19–21]. Animal studies had previously indicated that ingested salt can affect the gastric mucosal barrier leading to inflammation, diffuse erosions and epithelial degeneration [22–24]. There is a lively debate which carcinogen is the leading agent if both H. pylori infection and high-salt diet are present. In a mouse model, high salt intake led to severe gastritis and a higher degree of epithelial proliferation compared to the low-salt group, but H. pylori-induced intraepithelial neoplasia developed in both diet groups at a similar rate [25]. In Mongolian gerbils, the incidence of gastric cancer increased with rising concentration of salt in the animals’ diet [26]. This was independent of H. pylori infection status, but only in the presence of N-methyl-N-nitrosurea as additional strong carcinogen. Salt intake can lead to an upregulation of the expression of iNOS (inducible nitric oxide synthetase) and COX2 (cyclooxygenase 2) synergistically to the induction by H. pylori [27]. Salt furthermore increases the colonization of the gastric mucosa with H. pylori and enhances CagA-related inflammatory effects and their consequences including the proinflammatory cytokine milieu and later mucosal changes like atrophic gastritis [28, 29]. Exposition to high salt concentrations leads to an increased expression of CagA and increasing levels of interleukin-8 (IL8) as epithelial response [30]. This effect is confirmed for H. pylori strains that carry two copies of a specific motif of their cagA promotor region (TAATGA) [31]. Human studies demonstrated a significant salt effect only in H. pylori-positive patients in whom the gastric mucosa was already ‘pre-damaged’ by H. pylori-induced chronic active inflammation [21, 32]; a prospective study suggested that high salt intake had the strongest effect on gastric carcinogenesis in patients with both H. pylori infection and glandular atrophy in the stomach [32]. However, a case control study on 422 gastric cancer patients and 649 controls demonstrated a 2-fold increase in gastric cancer in patients with high salt intake, which was independent of other risk factors like H. pylori infection of smoking [33]. Despite the increasing knowledge, the exact interplay between salt-related damage of the gastric mucosa and H. pylori-driven inflammation needs further elucidation. H. pylori infection reduces the bioavailability of vitamin C, leading subsequently to decreased concentrations in plasma and gastric juice [34], whereas the luminal conBornschein /Malfertheiner Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM fected individuals [8]. A meta-analysis from Asia of 19 studies with approximately 2,500 gastric cancer patients and almost 4,000 matched controls showed an OR of 1.92 (95% confidence interval, CI: 1.32–2.78) for the development of non-cardia gastric cancer in H. pylori-positive patients [9], which was in concordance with a previous meta-analysis [10]. In 2003, the Helicobacter and Cancer Collaborative Group combined data from all available case control studies nested with prospective cohorts. Overall, 1,228 patients were included, and H. pylori infection was shown to be associated with non-cardia gastric cancer (OR 3.0, 95% CI: 2.3–3.8). The association was strengthened when H. pylori serology was performed ≥10 years before the cancer diagnosis (OR 5.9; 95% CI: 3.4–10.3) [11]. The explanation for the increased OR is that if sera were taken before disease manifestation, H. pylori colonization would likely disappear in the presence of atrophic gastritis and intestinal metaplasia (IM), and thus gastric cancer patients may present with a loss of anti-H. pylori antibodies at the time of disease manifestation. In fact, patients with early gastric cancer have a much higher prevalence of H. pylori antibodies when compared to those with advanced gastric cancer, resulting in a different attributable risk [9]. The time of serum sampling is crucial as was further proven by another study in which development of gastric cancer in the case of H. pylori infection was significantly higher if serum samples were taken within 90 days after tumor gastrectomy [12]. The attributable risk totally changed with the study of Ekström et al. [13] who reported an increase of the H. pylori-attributable OR for non-cardia cancer from 2.2 to 21.0 if the expression of the cytotoxic antigen A (CagA), a bacterial virulence factor, was coevaluated with anti-H. pylori serology by immunoblot analysis. In this analysis, 71–91% of gastric cancer was attributable to H. pylori infection. Antibodies to CagA persist longer in the serum than anti-H. pylori IgG so that evaluation of certain bacterial virulence factors may provide more precise results for the H. pylori-attributable risk for gastric carcinogenesis [14]. While early studies claim that H. pylori infection is only related to distal or ‘non-cardia’ gastric cancer, this is no longer true since there is clear evidence now for the pathogenetic relevance also in proximal gastric cancer or adenocarcinomas at the esophagogastric junction, if proper allocation of the tumor and assessment of the relevant risk factor are performed [15–17]. The risk for gastric carcinogenesis by H. pylori infection is similar for intestinal- and diffuse-type gastric cancers [15, 18]. H. pylori Virulence Factors Bacterial virulence factors influence the malignant potential of H. pylori [48]. Best investigated is the cag pathogenicity island (cagPAI) type IV secretion system necesH. pylori and Gastric Cancer sary for translocation of pathogenetic factors of H. pylori (e.g. CagA) into the epithelial cell [49, 50], which can induce a more severe inflammatory response, also increasing the risk for gastric carcinogenesis [51–53]. Injected CagA is rapidly phosphorylated by host Src kinases and has the potential to change intracellular signal transduction and to disrupt epithelial cell junctions [54, 55]. CagA leads to the activation of the Ras-mitogen-activated protein kinase pathway, involving the Ras-dependent kinases ERK1 and ERK2 with further transactivation of hostrelated pathways [56–58]. CagA-dependent activation of the Ras-ERK cascade increases also IL8 release and NFκB activation inducing the invasion of neutrophil granulocytes into the gastric mucosa [59]. NFκB-related carcinogenesis is enhanced by H. pylori-associated release of tumor necrosis factor-α-inducing protein (Tipα) enhancing the expression of TNFα with further involvement of IL8- and COX2-dependent pathways [60, 61]. Interaction of CagA with the E-cadherin/β-catenin system can lead to a direct transactivation of CDX1 and by this to metaplastic changes in the mucosa [62]. CagA is further thought to contribute to epithelial-mesenchymal transition, a hallmark of epithelial-derived carcinogenesis [63, 64]. Once intracellular, CagA is phosphorylated at certain glutamate-isoleucine-tyrosine-alanine (EPIYA) motifs. Four distinct EPIYA motifs are described (EPIYA-A, -B, -C, -D) [65, 66] whose prevalence varies by geographical region. They further influence the CagA-induced immune response as well as the related cancer risk. The OR for gastric cancer is about 7.3 in the case of one EPIYA-C segment, and can be up to 51 in the case of two or more segments [67, 68]. Relatives of patients with gastric cancer have been shown to carry H. pylori strains with a higher frequency of EPIYA-C segments [69]. Recently, genetic variations in further cagPAI-related genes have been demonstrated to be associated with gastric cancer [70]. A similar diversity has been identified for the vacuolating cytotoxin A (VacA) showing variations in its gene structure which can be divided into a signaling (s), a middle (m), and an intermediate (i) region [48]. After the first identification of s1/m1 strains showing a higher attributable risk for gastric cancer development, also i1 strains have been demonstrated to be associated with not only dysplastic but also malignant invasive tissue formation [67, 69, 71]. VacA has an inhibitory effect on GSK3β (glycogen synthase kinase 3-β)-regulated signaling pathways by phosphorylation through an Akt/PI3K (phosphatidylinositol-3-kinase)-mediated pathway, which leads to Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 251 Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM centration of reactive oxygen species in the stomach is increased [35]. Supplementation of vitamin C after H. pylori eradication can lead to a regression of premalignant lesions [36]. However, the EPIC (European Prospective Investigation into Cancer and Nutrition) study of more than 500,000 participants in 10 countries could not confirm an association of plasma vitamin C levels with gastric cancer development when confounding factors like body mass index, total energy intake, smoking, and H. pylori status were considered [37]. More than 40 mostly retrospective epidemiological studies have not confirmed the association between chronic alcohol consumption and gastric adenocarcinomas including cardia cancer [38–40]. However, a recent publication from the EPIC cohort reported an increased risk for gastric carcinogenesis for heavy alcohol consumption (>60 g per day) compared to very low intake (0.1–4.9 g per day) with a hazard ratio (HR) of 1.65 (95% CI: 1.06–2.58) [41]. Results of a systematic review analyzing the relation between cigarette smoking and gastric cancer including 42 cohort, case-cohort and case-control studies demonstrated that smoking is significantly associated with an elevated relative risk (RR) for both gastric cardia (RR = 1.87; 95% CI: 1.31–2.67) and non-cardia cancers (RR = 1.60; 95% CI: 1.41–1.80) [42]. This agrees with a previous meta-analysis [43] and the EPIC study which estimated that 17.6% (95% CI: 10.5–29.5%) of gastric cancers are related to smoking [42]. In a review analyzing the interaction of alimentary carcinogenic agents with H. pylori infection, the OR for the combined presence of both H. pylori and cocarcinogens was highest in all studies (2.3– 19.0), although no trial revealed an additive effect, and the statistical analysis for risk factor interaction was negative [44]. In comparison, the increased risk for gastric carcinogenesis in persons with a high intake of meat (total meat, processed meat and red meat: OR 1.93–5.32) was demonstrated only in H. pylori-positive subjects [45]. The postulated protective effect of fruits and vegetables, with high plasma levels of vitamin C, vitamin E and retinol as surrogate indicators, was only confirmed for H. pylori-positive individuals, although this interaction could not be statistically confirmed [37, 46, 47]. Host-Related Factors Epigenetic Changes H. pylori-driven inflammation can lead to methylation of CpG islands in gene promoters through the release of reactive oxygen species and nitric oxide, and by activation of the DNA methyltransferase [82, 83]. These epigenetic changes correlate with the degree of gastric inflammation and increase with the development of premalignant changes of the gastric mucosa and finally gastric neoplasia [84–86]. Eradication of the infection can decrease general methylation levels [87], but this effect is not consistent for all affected genes [88]. H. pylori-related methylation alters not only the function of common oncogenes or tumor suppressor genes but also transcription factors like forkhead box proteins (FOX) and the Runt-related transcription factor 3 (RUNX3), which show an association of the degree of methylation with distinct stages of gastric cancer progression and local invasive behavior [89, 90]. It seems that the respective methylation profiles are different for intestinal- and diffuse-type gastric cancer [91]. Global demethylation of the tumor cell genome in gastric cancer occurs in parallel to abnormal hypermethylation of tumor suppressor genes [92]. The global methylation patterns which can also be assessed by a serumbased test can define different gastric cancer subtypes 252 Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 [93] and show a potential to be used as a marker to detect metastasis and therefore may reflect the malignant potential of gastric cancer [86, 94]. Gene Polymorphisms of Immune Response Genes Hereditary gastric cancer is generally of the diffuse type and characterized by mutation in the CDH1 gene that is coding for E-cadherin [95]. However, sporadic genetic alterations, mainly single nucleotide polymorphisms (SNPs) of factors that modulate and mediate the inflammatory response to H. pylori infection, have been reported to have a broad influence on gastric cancer susceptibility [96, 97]. Among these are cytokine genes involved in the adaptive immune system [98–100] and pattern recognition factors initiating the innate immune system [101, 102]. Furthermore, variation of genes encoding for proteases [103], xenobiotic metabolism enzymes [104], cell cycle regulators [105, 106], mucins [107], HLA molecules [108], transcription factors [109], DNA repair enzymes [105, 110, 111], and micro-RNAs [112] has been reported to bear an increased risk for gastric cancer. Besides a ‘single gene’ approach, also pathway-related pattern searches can be performed to allow a broader assessment of the pathobiological background [113]. The identified SNPs might also have an effect on gastric cancer risk in relatives of the index patients [114]. IL1β, the most powerful proinflammatory cytokine produced in response to H. pylori infection, is known to also act as a strong acid inhibitor [115]. It has been postulated that carriers of specific SNPs in the IL1β gene or the gene of the IL1 receptor antagonist (IL1RN) have an up to 4-fold increased risk for developing gastric cancer [116]. Numerous studies in various ethnic groups have been published since the first report revealing conflicting results [117–120]. A meta-analysis demonstrated a decreasing association of these polymorphisms with gastric cancer risk for the accumulative data up to 2006 [121]. The OR for gastric cancer in the case of present IL1β gene mutation varies from 0.82 to 1.99 depending on the geographic region, the histological cancer subtype and the genetic locus that is altered [121]. More recent meta-analyses report an increased risk for gastric cancer with SNPs of the locus IL1β-511T and of IL1RN only in Caucasians [122–124]. There are further hints of an association between these SNPs and premalignant changes of the gastric mucosa, as well as an interaction with polymorphisms of the COX2 gene [125, 126]. Other cytokines which might bear functional relevance of defined haplotypes include IL10 [127, 128], TNFα [125, 129] and IL8 [130–132]. In most cases (except Bornschein /Malfertheiner Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM β-catenin release and furthermore modulation of apoptosis and cell cycle regulation [72, 73]. The outer membrane protein BabA (blood group antigen-binding adhesin) mediates the adherence to the ABO/Lewis b antigen in the gastric pit and is expressed by 40–95% of the H. pylori strains, also varying by geographic region [74, 75]. Patients infected with a BabApositive strain show a higher density of bacterial colonization in the stomach and enhanced inflammation due to increased IL8 levels [76]. Although BabA can mediate epithelial transdifferentiation to IM in response to H. pylori, a clear association to gastric cancer development has not yet been shown [75, 77]. However, H. pylori strains expressing all three factors (CagA, VacA, BabA) are associated with the highest risk for developing gastric cancer [78]. The genotype of the recently described factor iceA (induced by contact with epithelium A) might also be associated with gastric carcinogenesis [79, 80], and further H. pylori risk factors are under investigation with varying results depending on the method of detection and the time frame of tissue or blood sampling [81]. IL10), these cytokine polymorphisms result in a higher secretion of the corresponding cytokine leading to a stronger Th1-dominant immune response. A meta-analysis of 18 studies on polymorphisms in the IL8 gene revealed an overall increased risk, but this was particularly remarkable in Asian populations [132]. In contrast, polymorphisms of the IL10 gene seem to have a mainly protective effect concerning gastric cancer development, especially in Asian populations [128]. There is also interaction with other risk factors like H. pylori infection or smoking tobacco [133]. Intensive research has been performed on polymorphisms of pattern recognition receptors, e.g. Toll-like receptors (TLRs) and nucleotide-binding oligomerization domain (NOD) receptors [134, 135]. TLR variations may have a different effect on gastric cancer susceptibility. Polymorphisms in the TLR1 gene are associated with different gastric diseases including a protective effect against gastric cancer development (OR 0.4; 95% CI: 0.22–0.72), and are furthermore related with alterations of downstream cytokine signaling [136]. Results on TLR2 are conflicting, whereas TLR4 alterations seem to increase the risk for gastric adenocarcinoma and premalignant changes as shown by a recent meta-analysis [137–139]. Both ethnicity of the respective study population and H. pylori infection status have an impact on the results of these analyses [137, 139]. Results on polymorphisms of NOD1 or NOD2 and the effect on related downstream regulation, including NFκB-related signaling, are inconsistent [117, 135, 140]. activation of major oncogenic pathways include regulators of stem cell proliferation, NFκB-, and Wnt/β-catenin-related signaling, and are deregulated in more than 70% of the analyzed cancer samples [149]. The involved regulatory processes show different patterns depending on the tumor localization. Differences could be identified for proximal versus distal gastric cancer of the intestinal type, especially when compared with diffuse-type neoplasias [150, 151]. Lei et al. [152] suggested a stratification into three different gastric cancer subtypes showing not only specific pathobiological characteristics but also remarkable differences concerning the response to treatment with either 5-fluorouracil or compounds targeting the PI3K-Akt-mTOR axis. These data may facilitate the design of clinical trials using novel therapeutic agents [153]. Recently, by application of the genome-wide association studies approach, also SNPs in the TLR1 gene have been identified to determine susceptibility for H. pylori infection [154]. Complex protein level changes can be assessed by high-throughput techniques like matrix-assisted laser desorption/ionization imaging, and changes shown using hierarchical clustering or principal component analysis [155]. The related protein signatures are also capable of differentiating between tumor types, organ sites and even biological behavior of metastases and treatment response [156–159]. Genome-Wide Approach By genome-wide association studies of structural gene aberrations or specific expression profiles, classifiers for diagnostic purposes, an individual prognostic assessment, or a treatment susceptibility profile can be generated [96, 141, 142]. Instead of using de novo data, a computational ‘in silico’ analysis of publicly available (i.e. previously published) data can be performed to generate target signatures that can be correlated with any tumorspecific feature, like the degree of differentiation, general tumor stage, or survival and outcome after surgical treatment [143–145]. A focus on genes that are targets of therapeutic compounds (e.g. epithelial growth factor receptor, EGFR, HER2) might allow the prediction of the prognostic outcome with neoadjuvant or even palliative therapy regimens [146, 147]. A further task is the identification of mechanisms that make the carcinoma prone to local invasion and/or metastatic spread [148]. Gene expression signatures that lead to The inflammatory environment in the gastric mucosa mirrored by the cytokine milieu has a major influence on the initiation of gastric carcinogenesis (fig. 1). IL1β, mostly secreted by macrophages and to a lesser extent by epithelial and dendritic cells, induces the expression of other cytokines such as IL12, TNFα, IL2 and interferons (IFN) that subsequently shift the immune balance towards a mixed or Th1-predominant inflammation as it is seen in H. pylorimediated gastritis [160–162]. The subsequent infiltration of granulocytes and lymphocytic cells leads to a chronic inflammatory condition and lasts as long as the bacterium colonizes the gastric mucosa. The degree of colonization and gastritis is dependent on various factors, such as the presence and activity of regulatory T cells (Tregs) or the initial (naive) parietal cell mass (which reflects the acid-secreting capacity) [160–165]. Tregs are associated with increasing bacterial colonization [166], chronic inflammatory changes [167, 168] and the expression of immunosuppressive cytokines like IL10, IL17 and TGF-β [163, 169]. In H. pylori and Gastric Cancer Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 253 Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM Response to H. pylori in the Gastric Mucosa the case of gastric cancer, Tregs are increased both in the gastric mucosa and the peripheral blood [170–173]. As shown by immunohistochemistry, increasing numbers of FOXP3-expressing CD4+CD25+CD117lowTreg cells are associated with vascular, lymphatic and perineural invasion of gastric tumor cells, as well as with advanced tumor stage [174]. The ratio of Th1/Th2-derived cytokines is the highest in asymptomatic gastritis showing a steady decrease in gastric atrophy, IM and intraepithelial neoplasia progression to gastric adenocarcinoma. This is associated with a concomitant increase in the Treg cell compartment in the peripheral blood as well as persistence of CagA-positive strains that favors a Treg-mediated chronic inflammation [170]. When H. pylori infection is predominantly located in the antrum, the acid secretion is usually unchanged or can even be increased, resulting in ‘hyperchlorhydria’ which predisposes to duodenal and gastric ulcer formation. If H. pylori colonizes predominantly the gastric body, the antisecretory effect of IL1β leads to a vicious cycle by induction of hypochlorhydria which in turn fa254 Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 cilitates the further spread of H. pylori in the mucosa of the corpus and fundus. The resulting corpus-predominant inflammation leads to mucosal atrophy and IM. An additional impact of IL1β is given by its cytoprotective, antiulcerative effects and capability to modulate gastric motility and therefore delay gastric emptying [115]. Figueiredo et al. [175] analyzed different CagA and VacA genotypes of H. pylori strains isolated from patients with gastric cancer or nonatrophic gastritis in the context of the presence of an ‘IL1 proinflammatory genotype’, and identified combinations with either low or high risk for gastric cancer, resulting in a variable OR of 6–87. The ‘proinflammatory’ genotype is associated with elevated IL1β levels in the gastric mucosa [176]. The scores for mucosal atrophy and related gastritis are higher in H. pylori-infected patients with the proinflammatory IL1β-511 T/T genotype which also present with an elevation of the gastric juice pH as well as decreased pepsinogen I/II ratios as surrogate for mucosal atrophy [177]. The IL1β genotype seems to have no effect on physiological or histoBornschein /Malfertheiner Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM Fig. 1. Mucosal response to H. pylori infection. The inflammatory response of the gastric mucosa to H. pylori infection and other cocarcinogens is mediated by a shift towards a proinflammatory cytokine milieu, which leads to further mucosal damage and finally altered life cycle of the epithelial cells. These processes are enhanced in the presence of both bacterial virulence factors (e.g. CagA, VacA) and gene alterations that change the host’s susceptibility to further malignant tissue transformation. H. pylori and Gastric Cancer It is not yet clarified to which extent gastric epithelial stem cells as well as bone marrow-derived stem cells contribute to the processes mentioned above [202–204]. The local mucosal environment, like the mucin pattern, has a further influence on the H. pylori-related response pattern [205]. Eradication of H. pylori for Gastric Cancer Prevention In a meta-analysis on 6,695 patients, eradication of H. pylori infection decreased the RR of developing gastric cancer by 35% [206]. At present, most trials assessing the preventive effect of H. pylori eradication on gastric cancer incidence have been undertaken in high-incidence regions within Asia (table 1). In a prospective interventional study from Japan, patients with H. pylori-induced peptic ulcer disease (n = 1,342) were followed for a median of 3.4 years [207]. Gastric cancer occurred in 0.8% of the successfully eradicated patients in contrast to 2.3% of patients with eradication failure [207]. So far, the only prospective, randomized, placebo-controlled primary prevention study has been performed in China with 1,630 H. pylori-positive individuals being randomized on either eradication or placebo treatment [208]. Within a follow-up period of 7.5 years, there were 18 new cases of gastric cancer, 7 in the eradication group and 11 in the placebo group. Subgroup analysis revealed that all patients with newly diagnosed gastric cancer presented with preneoplastic changes of the gastric mucosa (gastric atrophy, IM) at baseline, whereas no case of gastric cancer was diagnosed in patients without baseline mucosal changes [208]. In a prospective observational study from Japan (1,787 patients; 9 years’ followup), all patients who still developed gastric adenocarcinoma after eradication presented with severe atrophic gastritis at baseline [209]. The risk of gastric carcinogenesis is significantly correlated with the degree of baseline atrophy that is induced by H. pylori-driven inflammation [210, 211]. In a prospective study from Japan, 4,655 healthy, asymptomatic individuals were followed up endoscopically for 7.7 years presenting an HR for gastric cancer of 7.1 in the case of H. pylori infection without glandular atrophy, 14.9 if both conditions had been detected and 61.9 if H. pylori infection could not be detected any more due to the severe atrophic changes of the gastric mucosa [212]. In multiple logistic regression analysis, degree and distribution of IM have also been demonstrated to be independent risk factors for gastric cancer development [213]. A nationwide cohort study from the Netherlands, including more than 90,000 participants, demonstrated a stepwise increase Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 255 Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM logical parameters of gastric mucosa in H. pylori-negative patients. In a study from Thailand, IL1β-511 TT carriers had significantly higher IL1β levels in the antrum than corresponding controls, also influenced by bacterial factors (e.g. CagA type) [178]. In contrast, data from Korea showed higher mucosal IL1β levels in patients with ‘wildtype haplotype’ compared to those with ‘proinflammatory haplotype’ [179]. The immune response can be modulated by further mechanisms. H. pylori-induced activation of NOD1 can lead to higher expression of IL8- and IFNγ-related signaling [180]. An increased gene expression of IL8, IL10 and TNFα that is induced by H. pylori-dependent TLR activation has been shown in adult patients with gastritis or further advanced diseases stages but also already in children positive for the infection [181–183]. These processes are mainly NFκB mediated, also leading to an increase in IL32 levels in a cagPAI-dependent manner [136, 182, 184]. Functional relevance has been attributed to CagL which can regulate the host’s production of IL1β via TLR2 and NOD2 activation [185]. These inflammatory processes are also related to the induction of certain transcription factors (e.g. CDX2) in the gastric mucosa that lead to transdifferentiation into spasmolytic polypeptide-expressing metaplasia or IM [186–188]. RUNX3 is deregulated in IM by tyrosine phosphorylation due to CagA-induced c-Scr activation leading to reduced expression at both the mRNA and protein levels [189, 190]. Downstream signaling involves ERK/ mitogen-activated protein kinase pathways that are also involved in the activation of the gastrin promoter by CagA [191]. Further induction of gastrin expression is mediated by CagL binding to an integrin-αvβ5/integrinlinked kinase complex of the host [192]. Gastrin itself is important for homeostasis in the intact gastric mucosa, and it has a complex role in gastric carcinogenesis, including the mediation of proliferation, angiogenesis and tissue invasion [193]. The gastrin receptor expression is increased in H. pylori gastritis [194] partly due to an IL1βinduced downregulation of gastrin and histamine levels in the stomach to inhibit acid secretion from parietal cells [115, 195, 196]. A further effect of epithelial contact with the cagPAI type IV secretion system is higher expression of the EGFR and its activation leading to downstream activation of COX2 [197, 198]. This is accompanied by a shift towards a proapoptotic homeostasis with increased expression of bax and decreased expression of bcl2 [199, 200]. The induction of oncogenes like cmyc is also interfering with these processes [199, 201]. Table 1. Effect of H. pylori eradication on gastric cancer incidence and preneoplastic conditions First author Year Country End point: regression atrophy/IM Ruiz [237] 2001 Colombia Schenk [220] 2000 Study type Population prosp. cohort 132 Netherlands prosp. cohort China case control 57 Lu [238] 2005 Lee [239] 2013 Taiwan You [240] 2006 China Ito [241] 2002 179 case control prosp. cohort 2,603 Japan prosp. cohort 22 Yamada [242] 2003 Japan 116 Ohkusa [224] 2001 Japan Cho [218] Korea prosp. cohort prosp. cohort prosp. cohort case control 80,255 case control prosp. cohort prosp. cohort 268 2013 End point: GC incidence Wu [226] 2009 Taiwan 3,365 163 190 Maehata [243] 2012 Japan Zhou [244] 2005 China Wong [208] 2004 China Saito [245] 2000 Japan Uemura [216] 1997 Japan Fukase [227] 2008 Japan prosp. cohort 544 Take [210] 2007 Japan 1,131 Uemura [8] 2001 Japan Kamada [209] 2005 Japan Leung [246] 2004 China Sung [217] 2000 China prosp. cohort prosp. cohort prosp. cohort prosp. cohort prosp. cohort prosp. cohort prosp. cohort 552 1,630 64 132 1,526 1,787 435 587 Groups Follow- Outcome up, years Special characteristics treatm. 29; control 82 6.0 regression of atrophy successful erad. 33; erad. failure 24 treatm. 92; control 87 1.0 no change in atrophy 1.8 regression of atrophy (–28.26%); IM with mixed results treatm. 841; control 1,762 Hp erad., vitamin supplements, garlic extract one arm 13.0 regression of atrophy (–77.2%); no change in IM only positive effect on regression of severe atrophy successful erad. 87; erad. failure 29 successful erad. 115; erad. failure 48 active treatm. 95; placebo 95 1.8 ‘early erad.’ 54,576; ‘late erad.’ 25,679 7.3 5.0 morphometric analogue scale evaluation – partly regression/ progression also for controls 5 year interval assessment – regression of atrophy (antrum, corpus); regression of IM (antrum, corpus) regression of atrophy (corpus); no change in IM regression of atrophy (–89%, corpus); regression of IM (–61%, antrum) regression of atrophy (–58.6%); regression of IM (–60.5%) by erad. – 5.9 – 7.2 GC incidence: 136/54,576 (2.5%) vs. 113/25,679 (4.4%) treatm. 177; control 91 Hp neg. 246; Hp pos. 306 active treatm. 817; placebo 813 3.0 GC incidence: 15/177 (8.5%) vs. 13/91 (14.3%) GC incidence: 1/246 (0.4%) vs. 5/306 (1.6) GC incidence: 7/817 (0.9%) vs. 11/813 (1.4%) eradication after peptic ulcer; ‘early’: within 1 year, HR 0.77 – treatm. 32; control 32 treatm. 65; control 67 2.0 treatm. 255; control 250 3.0 successful erad. 953; erad. failure 178 Hp neg. 280; Hp pos. 1,246 one arm 3.9 treatm. 220; control 215 active treatm. 295; placebo 292 5.0 1.3 3.0 5.0 7.5 3.0 7.8 9.0 1.0 – – intervention after subtotal gastrectomy population-based study no GC in subgroup without preneoplastic conditions GC incidence: 0/32 (0%) vs. progression of gastric 4/32 (12.5%) adenoma GC incidence: 0/65 (0.0%) vs. end point: 6/67 (9.0; IM regression after 2 years) metachronous GC after EMR for EGC GC incidence: 9/255 (3.5%) vs. end point: 24/250 (9.6%) metachronous GC after EMR for EGC GC incidence: 9/953 (0.9%) vs. risk increase for GC 4/178 (2.2) with baseline atrophy GC incidence: 0/280 (0%) vs. – 36/1,246 (2.9%) GC incidence: 20/1,787 (1.1%) all GC patients with severe baseline atrophy IM progression: 41.3 vs. 60.1% H. pylori persistence as negative predictor regression of IM in antrum – 256 Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 Bornschein /Malfertheiner Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM EGC = Early gastric cancer; EMR = endoscopic mucosal resection; erad. = eradication; GC = gastric cancer; Hp neg./pos. = H. pylori negative/positive; prosp. cohort = prospective cohort study; treatm. = eradication treatment. Point of no return? Chronic atrophic gastritis H. pylori infection IM Dysplasia Intestinal type Growth factors HIF1į9(*)(*)3'*),*) Inflammation IL1DŽ,/,/71)į,)1Dž ,/7*)DŽ Chronic active gastritis Transcription factors &';&'; 7)) 62; Oncogenes Tumor suppressor genes FPHWFP\F Gastric cancer $3&SSS581;)+,7 Invasion-related factors 003003003 (FDGKHULQ Diffuse type nogenesis. There are two major histological types of gastric adenocarcinoma, the intestinal and the diffuse type. Both are associated with H. pylori infection and certain pathobiological mechanisms including the activation of growth factors, a shift of certain transcription factors and an imbalance in tumor suppressor genes and oncogenes. The development of intestinal-type cancer follows distinct steps of histopathological changes of the mucosa. However, this sequence does not necessarily have to be complete or follow the specific order indicated here. No precursors of diffuse-type cancers are currently known. in gastric cancer incidence within 5 years’ follow-up that was 0.1% in patients with chronic atrophic gastritis, 0.25% in patients with IM, 0.6% in the case of mild or moderate dysplasia and 6% in the case of severe dysplasia at baseline assessment (HR 40.1; 95% CI: 32.2–50.1) [214]. What defines the point of no return, when eradication of H. pylori will no longer prevent further progression of IM and atrophic gastritis towards gastric cancer [215]? Several trials assessed to which degree preneoplastic changes could be reversed by H. pylori eradication. The degree of IM decreased after eradication therapy in patients endoscopically or surgically treated for early gastric cancer in a 3-year follow-up [216–218]. The data about the actual regression of IM or glandular atrophy are controversial. Several authors report an improvement only of the degree of inflammation within one year after eradication but no effect on metaplasia or atrophy [219, 220]. Rokkas et al. [221] presented a meta-analysis on the longterm effect of eradication therapy on gastric histology. The risk associated with atrophic gastritis was reduced by 45% in total (OR 0.55; 95% CI: 0.37–0.83), and by almost 80% for alterations in the gastric body (OR 0.21; 95% CI: 0.08–0.54). An influence on IM could not be confirmed in this study or in a recent meta-analysis of 12 studies [222] which showed that eradication of H. pylori led to significant improvement of atrophy in the gastric corpus, but not in the antrum, and to no improvement of IM. However, in this analysis the degree of mucosal changes is not mentioned, which is crucial since only extensive atrophic alterations impact on gastric function. A recent study from Taiwan demonstrated a reduction of atrophic changes by 77.2% after population mass eradication without a significant effect on IM prevalence [223]. In the same observation period, gastric cancer incidence was reduced by 25%. It has been suggested that the decisive factor whether or not H. pylori eradication has an effect is the length of follow-up since an improvement of mucosal inflammation can be documented within the first 6–12 months after eradication; however, a follow-up period of more than one year is necessary to demonstrate an effect on IM and atrophic changes [224, 225]. The site of biopsy sampling may also be an important factor [225]. The point of time at which H. pylori eradication can still contribute to gastric cancer prevention remains the burning question in this debate (fig. 2). In a cohort study of 80,255 patients, the risk for gastric cancer development was smaller with earlier H. pylori eradication after peptic H. pylori and Gastric Cancer Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 257 Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM Fig. 2. Histopathological and molecular changes in gastric carci- ulcer disease. Compared to the general population, patients that received early H. pylori eradication had no increased gastric cancer risk [226]. Even after endoscopic resection of early gastric adenocarcinoma, recurrence of metachronous gastric cancer is significantly reduced by H. pylori eradication [227]. A recent retrospective analysis on 268 H. pylori-positive patients after endoscopic cancer resection could not confirm these results [228]. However, the period of follow-up was identified as an independent risk factor. Conclusions H. pylori represents the main carcinogen in gastric neoplasia. For an individual risk assessment, the interaction between bacterial virulence factors and the host’s susceptibility profile must be taken into account. In spite of the proof that H. pylori eradication is effective in gastric cancer prevention in several studies, an ultimate study on a large population and a considerably longer observation time would convince all those who are reluctant to include H. pylori eradication in preventive strategies [229, 230]. In addition, a close and effective endoscopic follow-up and surveillance are mandatory in the case of present mucosal alterations at baseline assessment, even after successful H. pylori eradication [231–233]. Although this has already been recommended in European consensus guidelines [234, 235], it will be a matter of debate if this approach can be considered as cost-effective in low-incidence regions like central Europe or North America [236]. Disclosure Statement The authors declare that no financial or other conflict of interest exists in relation to the content of the article. 1 Schistosomes, liver flukes and Helicobacter pylori. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Lyon, 7–14 June 1994. IARC Monogr Eval Carcinog Risks Hum 1994;61:1–241. 2 Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, et al: A review of human carcinogens – part B: biological agents. Lancet Oncol 2009;10:321–322. 3 Watanabe T, Tada M, Nagai H, Sasaki S, Nakao M: Helicobacter pylori infection induces gastric cancer in Mongolian gerbils. Gastroenterology 1998;115:642–648. 4 Honda S, Fujioka T, Tokieda M, Satoh R, Nishizono A, Nasu M: Development of Helicobacter pylori-induced gastric carcinoma in Mongolian gerbils. Cancer Res 1998;58:4255– 4259. 5 Maruta F, Sugiyama A, Ishida K, Ikeno T, Murakami M, Kawasaki S, et al: Timing of Nmethyl-N-nitrosourea administration affects gastric carcinogenesis in Mongolian gerbils infected with Helicobacter pylori. Cancer Lett 2000;160:99–105. 6 Shimizu N, Inada K, Nakanishi H, Tsukamoto T, Ikehara Y, Kaminishi M, et al: Helicobacter pylori infection enhances glandular stomach carcinogenesis in Mongolian gerbils treated with chemical carcinogens. Carcinogenesis 1999;20:669–676. 7 Malfertheiner P, Sipponen P, Naumann M, Moayyedi P, Megraud F, Xiao SD, et al: Helicobacter pylori eradication has the potential to prevent gastric cancer: a state-of-the-art critique. Am J Gastroenterol 2005; 100: 2100– 2115. 8 Uemura N, Okamoto S, Yamamoto S, Matsumura N, Yamaguchi S, Yamakido M, et al: He- 258 Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 9 10 11 12 13 14 15 16 licobacter pylori infection and the development of gastric cancer. N Engl J Med 2001; 345:784–789. Huang JQ, Sridhar S, Chen Y, Hunt RH: Meta-analysis of the relationship between Helicobacter pylori seropositivity and gastric cancer. Gastroenterology 1998;114:1169–1179. Eslick GD, Lim LL, Byles JE, Xia HH, Talley NJ: Association of Helicobacter pylori infection with gastric carcinoma: a meta-analysis. Am J Gastroenterol 1999;94:2373–2379. Gastric cancer and Helicobacter pylori: a combined analysis of 12 case control studies nested within prospective cohorts. Gut 2001; 49: 347–353. Brenner H, Arndt V, Stegmaier C, Ziegler H, Rothenbacher D: Is Helicobacter pylori infection a necessary condition for noncardia gastric cancer? Am J Epidemiol 2004; 159: 252– 258. Ekström AM, Held M, Hansson LE, Engstrand L, Nyrén O: Helicobacter pylori in gastric cancer established by CagA immunoblot as a marker of past infection. Gastroenterology 2001;121:784–791. Huang JQ, Zheng GF, Sumanac K, Irvine EJ, Hunt RH: Meta-analysis of the relationship between cagA seropositivity and gastric cancer. Gastroenterology 2003;125:1636–1644. Bornschein J, Selgrad M, Warnecke M, Kuester D, Wex T, Malfertheiner P: H. pylori infection is a key risk factor for proximal gastric cancer. Dig Dis Sci 2010;55:3124–3131. Abrams JA, Gonsalves L, Neugut AI: Diverging trends in the incidence of reflux-related and Helicobacter pylori-related gastric cardia cancer. J Clin Gastroenterol 2013; 47: 322– 327. 17 Kamada T, Kurose H, Yamanaka Y, Manabe N, Kusunoki H, Shiotani A, et al: Relationship between gastroesophageal junction adenocarcinoma and Helicobacter pylori infection in Japan. Digestion 2012;85:256–260. 18 Hansen S, Vollset SE, Derakhshan MH, Fyfe V, Melby KK, Aase S, et al: Two distinct aetiologies of cardia cancer; evidence from premorbid serological markers of gastric atrophy and Helicobacter pylori status. Gut 2007; 56: 918–925. 19 Glade MJ: Food, nutrition, and the prevention of cancer: a global perspective. American Institute for Cancer Research/World Cancer Research Fund, American Institute for Cancer Research, 1997. Nutrition 1999; 15: 523– 526. 20 Kim HJ, Chang WK, Kim MK, Lee SS, Choi BY: Dietary factors and gastric cancer in Korea: a case-control study. Int J Cancer 2002;97: 531–535. 21 Lee SA, Kang D, Shim KN, Choe JW, Hong WS, Choi H: Effect of diet and Helicobacter pylori infection to the risk of early gastric cancer. J Epidemiol 2003;13:162–168. 22 Tatematsu M, Takahashi M, Hananouchi M, Shirai T, Hirose M: Protective effect of mucin on experimental gastric cancer induced by N-methyl-N′-nitro-N-nitrosoguanidine plus sodium chloride in rats. Gann 1976; 67: 223– 229. 23 Liu C, Russell RM: Nutrition and gastric cancer risk: an update. Nutr Rev 2008; 66: 237– 249. 24 Takahashi M, Hasegawa R: Enhancing effects of dietary salt on both initiation and promotion stages of rat gastric carcinogenesis. Princess Takamatsu Symp 1985;16:169–182. Bornschein /Malfertheiner Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM References H. pylori and Gastric Cancer 37 Jenab M, Riboli E, Ferrari P, Sabate J, Slimani N, Norat T, et al: Plasma and dietary vitamin C levels and risk of gastric cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST). Carcinogenesis 2006;27:2250–2257. 38 Boeing H: Epidemiological research in stomach cancer: progress over the last ten years. J Cancer Res Clin Oncol 1991;117:133–143. 39 Franke A, Teyssen S, Singer MV: Alcohol-related diseases of the esophagus and stomach. Dig Dis 2005;23:204–213. 40 Pollack ES, Nomura AM, Heilbrun LK, Stemmermann GN, Green SB: Prospective study of alcohol consumption and cancer. N Engl J Med 1984;310:617–621. 41 Duell EJ, Travier N, Lujan-Barroso L, ClavelChapelon F, Boutron-Ruault MC, Morois S, et al: Alcohol consumption and gastric cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Am J Clin Nutr 2011;94:1266–1275. 42 Ladeiras-Lopes R, Pereira AK, Nogueira A, Pinheiro-Torres T, Pinto I, Santos-Pereira R, et al: Smoking and gastric cancer: systematic review and meta-analysis of cohort studies. Cancer Causes Control 2008;19:689–701. 43 Tredaniel J, Boffetta P, Buiatti E, Saracci R, Hirsch A: Tobacco smoking and gastric cancer: review and meta-analysis. Int J Cancer 1997;72:565–573. 44 Gonzalez CA, Lopez-Carrillo L: Helicobacter pylori, nutrition and smoking interactions: their impact in gastric carcinogenesis. Scand J Gastroenterol 2010;45:6–14. 45 Gonzalez CA, Jakszyn P, Pera G, Agudo A, Bingham S, Palli D, et al: Meat intake and risk of stomach and esophageal adenocarcinoma within the European Prospective Investigation Into Cancer and Nutrition (EPIC). J Natl Cancer Inst 2006;98:345–354. 46 Epplein M, Nomura AM, Hankin JH, Blaser MJ, Perez-Perez G, Stemmermann GN, et al: Association of Helicobacter pylori infection and diet on the risk of gastric cancer: a casecontrol study in Hawaii. Cancer Causes Control 2008;19:869–877. 47 Jenab M, Riboli E, Ferrari P, Friesen M, Sabate J, Norat T, et al: Plasma and dietary carotenoid, retinol and tocopherol levels and the risk of gastric adenocarcinomas in the European prospective investigation into cancer and nutrition. Br J Cancer 2006;95:406–415. 48 Wroblewski LE, Peek RM Jr, Wilson KT: Helicobacter pylori and gastric cancer: factors that modulate disease risk. Clin Microbiol Rev 2010;23:713–739. 49 Backert S, Ziska E, Brinkmann V, ZimnyArndt U, Fauconnier A, Jungblut PR, et al: Translocation of the Helicobacter pylori CagA protein in gastric epithelial cells by a type IV secretion apparatus. Cell Microbiol 2000; 2: 155–164. 50 Odenbreit S, Puls J, Sedlmaier B, Gerland E, Fischer W, Haas R: Translocation of Helicobacter pylori CagA into gastric epithelial cells by type IV secretion. Science 2000;287:1497–1500. Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 51 Blaser MJ, Perez-Perez GI, Kleanthous H, Cover TL, Peek RM, Chyou PH, et al: Infection with Helicobacter pylori strains possessing cagA is associated with an increased risk of developing adenocarcinoma of the stomach. Cancer Res 1995;55:2111–2115. 52 Enroth H, Kraaz W, Engstrand L, Nyren O, Rohan T: Helicobacter pylori strain types and risk of gastric cancer: a case-control study. Cancer Epidemiol Biomarkers Prev 2000;9:981–985. 53 Parsonnet J, Friedman GD, Orentreich N, Vogelman H: Risk for gastric cancer in people with CagA positive or CagA negative Helicobacter pylori infection. Gut 1997;40:297–301. 54 Saadat I, Higashi H, Obuse C, Umeda M, Murata-Kamiya N, Saito Y, et al: Helicobacter pylori CagA targets PAR1/MARK kinase to disrupt epithelial cell polarity. Nature 2007;447: 330–333. 55 Stein M, Bagnoli F, Halenbeck R, Rappuoli R, Fantl WJ, Covacci A: c-Src/Lyn kinases activate Helicobacter pylori CagA through tyrosine phosphorylation of the EPIYA motifs. Mol Microbiol 2002;43:971–980. 56 Hatakeyama M: Oncogenic mechanisms of the Helicobacter pylori CagA protein. Nat Rev Cancer 2004;4:688–694. 57 Tsutsumi R, Higashi H, Higuchi M, Okada M, Hatakeyama M: Attenuation of Helicobacter pylori CagA × SHP-2 signaling by interaction between CagA and C-terminal Src kinase. J Biol Chem 2003;278:3664–3670. 58 Higashi H, Tsutsumi R, Muto S, Sugiyama T, Azuma T, Asaka M, et al: SHP-2 tyrosine phosphatase as an intracellular target of Helicobacter pylori CagA protein. Science 2002; 295:683–686. 59 Brandt S, Kwok T, Hartig R, Konig W, Backert S: NF-kappaB activation and potentiation of proinflammatory responses by the Helicobacter pylori CagA protein. Proc Natl Acad Sci USA 2005;102:9300–9305. 60 Kim H, Lim JW, Kim KH: Helicobacter pyloriinduced expression of interleukin-8 and cyclooxygenase-2 in AGS gastric epithelial cells: mediation by nuclear factor-kappaB. Scand J Gastroenterol 2001;36:706–716. 61 Kuzuhara T, Suganuma M, Kurusu M, Fujiki H: Helicobacter pylori-secreting protein Tipalpha is a potent inducer of chemokine gene expressions in stomach cancer cells. J Cancer Res Clin Oncol 2007;133:287–296. 62 Murata-Kamiya N, Kurashima Y, Teishikata Y, Yamahashi Y, Saito Y, Higashi H, et al: Helicobacter pylori CagA interacts with E-cadherin and deregulates the beta-catenin signal that promotes intestinal transdifferentiation in gastric epithelial cells. Oncogene 2007; 26: 4617–4626. 63 Katoh M: Epithelial-mesenchymal transition in gastric cancer (review). Int J Oncol 2005;27: 1677–1683. 64 Oliveira C, Bordin MC, Grehan N, Huntsman D, Suriano G, Machado JC, et al: Screening Ecadherin in gastric cancer families reveals germline mutations only in hereditary diffuse gastric cancer kindred. Hum Mutat 2002;19:510–517. 259 Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM 25 Rogers AB, Taylor NS, Whary MT, Stefanich ED, Wang TC, Fox JG: Helicobacter pylori but not high salt induces gastric intraepithelial neoplasia in B6129 mice. Cancer Res 2005;65: 10709–10715. 26 Kato S, Tsukamoto T, Mizoshita T, Tanaka H, Kumagai T, Ota H, et al: High salt diets dosedependently promote gastric chemical carcinogenesis in Helicobacter pylori-infected Mongolian gerbils associated with a shift in mucin production from glandular to surface mucous cells. Int J Cancer 2006;119:1558–1566. 27 Toyoda T, Tsukamoto T, Hirano N, Mizoshita T, Kato S, Takasu S, et al: Synergistic upregulation of inducible nitric oxide synthase and cyclooxygenase-2 in gastric mucosa of Mongolian gerbils by a high-salt diet and Helicobacter pylori infection. Histol Histopathol 2008;23:593–599. 28 Fox JG, Dangler CA, Taylor NS, King A, Koh TJ, Wang TC: High-salt diet induces gastric epithelial hyperplasia and parietal cell loss, and enhances Helicobacter pylori colonization in C57BL/6 mice. Cancer Res 1999; 59: 4823–4828. 29 Gaddy JA, Radin JN, Loh JT, Zhang F, Washington MK, Peek RM Jr, et al: High dietary salt intake exacerbates Helicobacter pylori-induced gastric carcinogenesis. Infect Immun 2013;81:2258–2267. 30 Loh JT, Torres VJ, Cover TL: Regulation of Helicobacter pylori cagA expression in response to salt. Cancer Res 2007;67:4709–4715. 31 Loh JT, Friedman DB, Piazuelo MB, Bravo LE, Wilson KT, Peek RM Jr, et al: Analysis of Helicobacter pylori cagA promoter elements required for salt-induced upregulation of CagA expression. Infect Immun 2012; 80: 3094–3106. 32 Shikata K, Kiyohara Y, Kubo M, Yonemoto K, Ninomiya T, Shirota T, et al: A prospective study of dietary salt intake and gastric cancer incidence in a defined Japanese population: the Hisayama study. Int J Cancer 2006; 119: 196–201. 33 Peleteiro B, Lopes C, Figueiredo C, Lunet N: Salt intake and gastric cancer risk according to Helicobacter pylori infection, smoking, tumour site and histological type. Br J Cancer 2011;104:198–207. 34 Woodward M, Tunstall-Pedoe H, McColl K: Helicobacter pylori infection reduces systemic availability of dietary vitamin C. Eur J Gastroenterol Hepatol 2001;13:233–237. 35 Drake IM, Mapstone NP, Schorah CJ, White KL, Chalmers DM, Dixon MF, et al: Reactive oxygen species activity and lipid peroxidation in Helicobacter pylori associated gastritis: relation to gastric mucosal ascorbic acid concentrations and effect of H. pylori eradication. Gut 1998;42:768–771. 36 Correa P, Fontham ET, Bravo JC, Bravo LE, Ruiz B, Zarama G, et al: Chemoprevention of gastric dysplasia: randomized trial of antioxidant supplements and anti-Helicobacter pylori therapy. J Natl Cancer Inst 2000;92:1881– 1888. 260 Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 78 Gerhard M, Lehn N, Neumayer N, Boren T, Rad R, Schepp W, et al: Clinical relevance of the Helicobacter pylori gene for blood-group antigen-binding adhesin. Proc Natl Acad Sci USA 1999;96:12778–12783. 79 Wei GC, Chen J, Liu AY, Zhang M, Liu XJ, Liu D, et al: Prevalence of Helicobacter pylori vacA, cagA and iceA genotypes and correlation with clinical outcome. Exp Ther Med 2012;4:1039–1044. 80 Shiota S, Watada M, Matsunari O, Iwatani S, Suzuki R, Yamaoka Y: Helicobacter pylori iceA, clinical outcomes, and correlation with cagA: a meta-analysis. PLoS One 2012; 7:e30354. 81 Epplein M, Zheng W, Xiang YB, Peek RM Jr, Li H, Correa P, et al: Prospective study of Helicobacter pylori biomarkers for gastric cancer risk among Chinese men. Cancer Epidemiol Biomarkers Prev 2012;21:2185–2192. 82 Niwa T, Ushijima T: Induction of epigenetic alterations by chronic inflammation and its significance on carcinogenesis. Adv Genet 2010;71:41–56. 83 Liu JB, Wu XM, Cai J, Zhang JY, Zhang JL, Zhou SH, et al: CpG island methylator phenotype and Helicobacter pylori infection associated with gastric cancer. World J Gastroenterol 2012;18:5129–5134. 84 Yoshida T, Kato J, Maekita T, Yamashita S, Enomoto S, Ando T, et al: Altered mucosal DNA methylation in parallel with highly active Helicobacter pylori-related gastritis. Gastric Cancer 2013;16:488–497. 85 Zou XP, Zhang B, Zhang XQ, Chen M, Cao J, Liu WJ: Promoter hypermethylation of multiple genes in early gastric adenocarcinoma and precancerous lesions. Hum Pathol 2009; 40:1534–1542. 86 Compare D, Rocco A, Liguori E, D’Armiento FP, Persico G, Masone S, et al: Global DNA hypomethylation is an early event in Helicobacter pylori-related gastric carcinogenesis. J Clin Pathol 2011;64:677–682. 87 Nanjo S, Asada K, Yamashita S, Nakajima T, Nakazawa K, Maekita T, et al: Identification of gastric cancer risk markers that are informative in individuals with past H. pylori infection. Gastric Cancer 2012;15:382–388. 88 Shin CM, Kim N, Lee HS, Park JH, Ahn S, Kang GH, et al: Changes in aberrant DNA methylation after Helicobacter pylori eradication: a long-term follow-up study. Int J Cancer 2013;133:2034–2042. 89 Cheng AS, Li MS, Kang W, Cheng VY, Chou JL, Lau SS, et al: Helicobacter pylori causes epigenetic dysregulation of FOXD3 to promote gastric carcinogenesis. Gastroenterology 2013;144:122–133 e9. 90 Lu XX, Yu JL, Ying LS, Han J, Wang S, Yu QM, et al: Stepwise cumulation of RUNX3 methylation mediated by Helicobacter pylori infection contributes to gastric carcinoma progression. Cancer 2012;118:5507–5517. 91 Selaru FM, David S, Meltzer SJ, Hamilton JP: Epigenetic events in gastrointestinal cancer. Am J Gastroenterol 2009;104:1910–1912. 92 Balassiano K, Lima S, Jenab M, Overvad K, Tjonneland A, Boutron-Ruault MC, et al: Aberrant DNA methylation of cancer-associated genes in gastric cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST). Cancer Lett 2011;311:85–95. 93 Zheng Z, Andersson AF, Ye W, Nyren O, Normark S, Engstrand L: A method for metagenomics of Helicobacter pylori from archived formalin-fixed gastric biopsies permitting longitudinal studies of carcinogenic risk. PLoS One 2011;6:e26442. 94 Shigematsu Y, Niwa T, Yamashita S, Taniguchi H, Kushima R, Katai H, et al: Identification of a DNA methylation marker that detects the presence of lymph node metastases of gastric cancers. Oncol Lett 2012;4:268–274. 95 Guilford P, Hopkins J, Harraway J, McLeod M, McLeod N, Harawira P, et al: E-cadherin germline mutations in familial gastric cancer. Nature 1998;26;392:402–405. 96 Saeki N, Ono H, Sakamoto H, Yoshida T: Genetic factors related to gastric cancer susceptibility identified using a genome-wide association study. Cancer Sci 2013;104:1–8. 97 Wex T, Bornschein J, Malfertheiner P: Host polymorphisms of immune regulatory genes as risk factors for gastric cancer. Minerva Gastroenterol Dietol 2009;55:395–408. 98 Machado JC, Figueiredo C, Canedo P, Pharoah P, Carvalho R, Nabais S, et al: A proinflammatory genetic profile increases the risk for chronic atrophic gastritis and gastric carcinoma. Gastroenterology 2003;125:364–371. 99 Crusius JB, Canzian F, Capella G, Pena AS, Pera G, Sala N, et al: Cytokine gene polymorphisms and the risk of adenocarcinoma of the stomach in the European prospective investigation into cancer and nutrition (EPICEURGAST). Ann Oncol 2008;19:1894–1902. 100 Hou L, El-Omar EM, Chen J, Grillo P, Rabkin CS, Baccarelli A, et al: Polymorphisms in Th1-type cell-mediated response genes and risk of gastric cancer. Carcinogenesis 2007; 28:118–123. 101 Santini D, Angeletti S, Ruzzo A, Dicuonzo G, Galluzzo S, Vincenzi B, et al: Toll-like receptor 4 Asp299Gly and Thr399Ile polymorphisms in gastric cancer of intestinal and diffuse histotypes. Clin Exp Immunol 2008; 154:360–364. 102 Wex T, Ebert MP, Kropf S, Dierkes J, Schuttler K, Rocken C, et al: Gene polymorphisms of the NOD-2/CARD-15 gene and the risk of gastric cancer in Germany. Anticancer Res 2008;28:757–762. 103 Ye S: Polymorphism in matrix metalloproteinase gene promoters: implication in regulation of gene expression and susceptibility of various diseases. Matrix Biol 2000; 19: 623–629. 104 Geddert H, Kiel S, Zotz RB, Zhang J, Willers R, Gabbert HE, et al: Polymorphism of p16 INK4A and cyclin D1 in adenocarcinomas of the upper gastrointestinal tract. J Cancer Res Clin Oncol 2005;131:803–808. Bornschein /Malfertheiner Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM 65 Higashi H, Yokoyama K, Fujii Y, Ren S, Yuasa H, Saadat I, et al: EPIYA motif is a membrane-targeting signal of Helicobacter pylori virulence factor CagA in mammalian cells. J Biol Chem 2005;280:23130–23137. 66 Naito M, Yamazaki T, Tsutsumi R, Higashi H, Onoe K, Yamazaki S, et al: Influence of EPIYA-repeat polymorphism on the phosphorylation-dependent biological activity of Helicobacter pylori CagA. Gastroenterology 2006; 130:1181–1190. 67 Basso D, Zambon CF, Letley DP, Stranges A, Marchet A, Rhead JL, et al: Clinical relevance of Helicobacter pylori cagA and vacA gene polymorphisms. Gastroenterology 2008;135:91–99. 68 Ferreira RM, Machado JC, Leite M, Carneiro F, Figueiredo C: The number of Helicobacter pylori CagA EPIYA C tyrosine phosphorylation motifs influences the pattern of gastritis and the development of gastric carcinoma. Histopathology 2012;60:992–998. 69 Queiroz DM, Silva CI, Goncalves MH, BragaNeto MB, Fialho AB, Fialho AM, et al: Higher frequency of cagA EPIYA-C phosphorylation sites in H. pylori strains from first-degree relatives of gastric cancer patients. BMC Gastroenterol 2012;12:107. 70 Rizzato C, Torres J, Plummer M, Munoz N, Franceschi S, Camorlinga-Ponce M, et al: Variations in Helicobacter pylori cytotoxinassociated genes and their influence in progression to gastric cancer: implications for prevention. PLoS One 2012;7:e29605. 71 Douraghi M, Talebkhan Y, Zeraati H, Ebrahimzadeh F, Nahvijoo A, Morakabati A, et al: Multiple gene status in Helicobacter pylori strains and risk of gastric cancer development. Digestion 2009;80:200–207. 72 Manente L, Perna A, Buommino E, Altucci L, Lucariello A, Citro G, et al: The Helicobacter pylori’s protein VacA has direct effects on the regulation of cell cycle and apoptosis in gastric epithelial cells. J Cell Physiol 2008;214:582–587. 73 Nakayama M, Hisatsune J, Yamasaki E, Isomoto H, Kurazono H, Hatakeyama M, et al: Helicobacter pylori VacA-induced inhibition of GSK3 through the PI3K/Akt signaling pathway. J Biol Chem 2009;284:1612–1619. 74 Prinz C, Hafsi N, Voland P: Helicobacter pylori virulence factors and the host immune response: implications for therapeutic vaccination. Trends Microbiol 2003;11:134–138. 75 Ishijima N, Suzuki M, Ashida H, Ichikawa Y, Kanegae Y, Saito I, et al: BabA-mediated adherence is a potentiator of the Helicobacter pylori type IV secretion system activity. J Biol Chem 2011;286:25256–25264. 76 Rad R, Gerhard M, Lang R, Schoniger M, Rosch T, Schepp W, et al: The Helicobacter pylori blood group antigen-binding adhesin facilitates bacterial colonization and augments a nonspecific immune response. J Immunol 2002;168:3033–3041. 77 Chen MY, He CY, Meng X, Yuan Y: Association of Helicobacter pylori babA2 with peptic ulcer disease and gastric cancer. World J Gastroenterol 2013;19:4242–4251. H. pylori and Gastric Cancer 117 Kupcinskas J, Wex T, Bornschein J, Selgrad M, Leja M, Juozaityte E, et al: Lack of association between gene polymorphisms of angiotensin converting enzyme, Nod-like receptor 1, Toll-like receptor 4, FAS/FASL and the presence of Helicobacter pylori-induced premalignant gastric lesions and gastric cancer in Caucasians. BMC Med Genet 2011;12: 112. 118 Kupcinskas L, Wex T, Kupcinskas J, Leja M, Ivanauskas A, Jonaitis LV, et al: Interleukin1B and interleukin-1 receptor antagonist gene polymorphisms are not associated with premalignant gastric conditions: a combined haplotype analysis. Eur J Gastroenterol Hepatol 2010;22:1189–1195. 119 Wex T, Leodolter A, Bornschein J, Kuester D, Kahne T, Kropf S, et al: Interleukin 1 beta (IL1B) gene polymorphisms are not associated with gastric carcinogenesis in Germany. Anticancer Res 2010;30:505–511. 120 El Omar EM, Carrington M, Chow WH, McColl KEL, Bream JH, Young HA, et al: Interleukin-1 polymorphisms associated with increased risk of gastric cancer. Nature 2000;404:398–402. 121 Kamangar F, Cheng C, Abnet CC, Rabkin CS: Interleukin-1B polymorphisms and gastric cancer risk – a meta-analysis. Cancer Epidemiol Biomarkers Prev 2006; 15: 1920– 1928. 122 Camargo MC, Mera R, Correa P, Peek RM Jr, Fontham ET, Goodman KJ, et al: Interleukin-1beta and interleukin-1 receptor antagonist gene polymorphisms and gastric cancer: a meta-analysis. Cancer Epidemiol Biomarkers Prev 2006;15:1674–1687. 123 Vincenzi B, Patti G, Galluzzo S, Pantano F, Venditti O, Santini D, et al: Interleukin 1beta-511T gene (IL1beta) polymorphism is correlated with gastric cancer in the Caucasian population: results from a meta-analysis. Oncol Rep 2008;20:1213–1220. 124 Wang P, Xia HH, Zhang JY, Dai LP, Xu XQ, Wang KJ: Association of interleukin-1 gene polymorphisms with gastric cancer: a metaanalysis. Int J Cancer 2007;120:552–562. 125 Tahara T, Shibata T, Yamashita H, Yoshioka D, Okubo M, Yonemura J, et al: Synergistic effect of IL-1beta and TNF-alpha polymorphisms on the H. pylori-related gastric premalignant condition. Hepatogastroenterology 2012;59:2416–2420. 126 da Costa DM, Neves-Filho EH, Alves MK, Rabenhorst SH: Interleukin polymorphisms and differential methylation status in gastric cancer: an association with Helicobacter pylori infection. Epigenomics 2013; 5: 167–175. 127 Suarez A, Castro P, Alonso R, Mozo L, Gutierrez C: Interindividual variations in constitutive interleukin-10 messenger RNA and protein levels and their association with genetic polymorphisms. Transplantation 2003;75:711–717. Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 128 Xue H, Wang YC, Lin B, An J, Chen L, Chen J, et al: A meta-analysis of interleukin-10 -592 promoter polymorphism associated with gastric cancer risk. PLoS One 2012;7:e39868. 129 Wilson AG, Symons JA, McDowell TL, McDevitt HO, Duff GW: Effects of a polymorphism in the human tumor necrosis factor alpha promoter on transcriptional activation. Proc Natl Acad Sci USA 1997; 94: 3195–3199. 130 Ohyauchi M, Imatani A, Yonechi M, Asano N, Miura A, Iijima K, et al: The polymorphism interleukin 8 -251 A/T influences the susceptibility of Helicobacter pylori related gastric diseases in the Japanese population. Gut 2005;54:330–335. 131 Felipe AV, Silva TD, Pimenta CA, Kassab P, Forones NM: lnterleukin-8 gene polymorphism and susceptibility to gastric cancer in a Brazilian population. Biol Res 2012; 45: 369–374. 132 Xue H, Liu J, Lin B, Wang Z, Sun J, Huang G: A meta-analysis of interleukin-8 -251 promoter polymorphism associated with gastric cancer risk. PLoS One 2012;7:e28083. 133 Kim J, Cho YA, Choi IJ, Lee YS, Kim SY, Shin A, et al: Effects of interleukin-10 polymorphisms, Helicobacter pylori infection, and smoking on the risk of noncardia gastric cancer. PLoS One 2012;7:e29643. 134 Hishida A, Matsuo K, Goto Y, Naito M, Wakai K, Tajima K, et al: No associations of Toll-like receptor 2 (TLR2) -196 to -174del polymorphism with the risk of Helicobacter pylori seropositivity, gastric atrophy, and gastric cancer in Japanese. Gastric Cancer 2010;13:251–257. 135 Companioni O, Bonet C, Munoz X, Weiderpass E, Panico S, Tumino R, et al: Polymorphisms of H. pylori signaling pathway genes and gastric cancer risk in the European EPIC-Eurgast cohort. Int J Cancer 2014;134: 92–101. 136 Yang CA, Scheibenbogen C, Bauer S, Kleinle C, Wex T, Bornschein J, et al: A frequent Toll-like receptor 1 gene polymorphism affects NK- and T-cell IFN-gamma production and is associated with Helicobacter pylori-induced gastric disease. Helicobacter 2013;18:13–21. 137 Castano-Rodriguez N, Kaakoush NO, Goh KL, Fock KM, Mitchell HM: The role of TLR2, TLR4 and CD14 genetic polymorphisms in gastric carcinogenesis: a case-control study and meta-analysis. PLoS One 2013;8:e60327. 138 Zou TH, Wang ZH, Fang JY: Positive association between Toll-like receptor 4 gene +896A/G polymorphism and susceptibility to gastric carcinogenesis: a meta-analysis. Tumour Biol 2013;34:2441–2450. 261 Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM 105 Agundez JA: Polymorphisms of human Nacetyltransferases and cancer risk. Curr Drug Metab 2008;9:520–531. 106 Capella G, Pera G, Sala N, Agudo A, Rico F, Del Giudicce G, et al: DNA repair polymorphisms and the risk of stomach adenocarcinoma and severe chronic gastritis in the EPIC-EURGAST study. Int J Epidemiol 2008;37:1316–1325. 107 Silva F, Carvalho F, Peixoto A, Seixas M, Almeida R, Carneiro F, et al: MUC1 gene polymorphism in the gastric carcinogenesis pathway. Eur J Hum Genet 2001;9:548–552. 108 Magnusson PKE, Enroth H, Eriksson I, Held M, Nyren O, Engstrand L, et al: Gastric cancer and human leukocyte antigen: distinct DQ and DR alleles are associated with development of gastric cancer and infection by Helicobacter pylori. Cancer Res 2001; 61: 2684–2689. 109 Lim B, Ju H, Kim M, Kang C: Increased genetic susceptibility to intestinal-type gastric cancer is associated with increased activity of the RUNX3 distal promoter. Cancer 2011; 117:5161–5171. 110 Ikeda S, Sasazuki S, Natsukawa S, Shaura K, Koizumi Y, Kasuga Y, et al: Screening of 214 single nucleotide polymorphisms in 44 candidate cancer susceptibility genes: a casecontrol study on gastric and colorectal cancers in the Japanese population. Am J Gastroenterol 2008;103:1476–1487. 111 Jiang J, Jia Z, Cao D, Jin MS, Kong F, Suo J, et al: Polymorphisms of the DNA methyltransferase 1 associated with reduced risks of Helicobacter pylori infection and increased risks of gastric atrophy. PLoS One 2012; 7:e46058. 112 Song MY, Su HJ, Zhang L, Ma JL, Li JY, Pan KF, et al: Genetic polymorphisms of miR146a and miR-27a, H. pylori infection, and risk of gastric lesions in a Chinese population. PLoS One 2013;8:e61250. 113 Li WQ, Hu N, Wang Z, Yu K, Su H, Wang L, et al: Genetic variants in epidermal growth factor receptor pathway genes and risk of esophageal squamous cell carcinoma and gastric cancer in a Chinese population. PLoS One 2013;8:e68999. 114 Li H, Zang J, Wang P, Dai L, Zhang J, Wang K: Gastric cancer susceptibility in gastric cancer relatives: attributable risks of macrophage migration inhibitory factor promoter polymorphism and Helicobacter pylori. Cytokine 2012;60:346–351. 115 El-Omar EM: The importance of interleukin 1beta in Helicobacter pylori associated disease. Gut 2001;48:743–747. 116 El-Omar EM, Carrington M, Chow WH, McColl KE, Bream JH, Young HA, et al: Interleukin-1 polymorphisms associated with increased risk of gastric cancer. Nature 2000; 404:398–402. 262 Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 152 153 154 155 156 157 158 159 160 161 162 163 164 expression of gastric cardia and noncardia cancers from a high-risk population in china. PLoS One 2013;8:e63826. Lei Z, Tan IB, Das K, Deng N, Zouridis H, Pattison S, et al: Identification of molecular subtypes of gastric cancer with different responses to PI3-kinase inhibitors and 5-fluorouracil. Gastroenterology 2013; 145: 554– 565. Wong H, Yau T: Molecular targeted therapies in advanced gastric cancer: does tumor histology matter? Therap Adv Gastroenterol 2013;6:15–31. Mayerle J, Kuipers EJ, Lerch MM: Genetic variants associated with susceptibility to Helicobacter pylori – reply. JAMA 2013; 310: 976–977. Deininger SO, Ebert MP, Futterer A, Gerhard M, Rocken C: MALDI imaging combined with hierarchical clustering as a new tool for the interpretation of complex human cancers. J Proteome Res 2008; 7: 5230– 5236. Meding S, Nitsche U, Balluff B, Elsner M, Rauser S, Schone C, et al: Tumor classification of six common cancer types based on proteomic profiling by MALDI imaging. J Proteome Res 2012;11:1996–2003. Wang D, Ye F, Sun Y, Li W, Liu H, Jiang J, et al: Protein signatures for classification and prognosis of gastric cancer a signaling pathway-based approach. Am J Pathol 2011;179: 1657–1666. Qian J, Li F, Yu J, Yang Z, Chen J: Mining predictive biomarker for neoadjuvant chemotherapy in gastric cancer by proteomics. Hepatogastroenterology 2011;58:1828–1833. Torti D, Sassi F, Galimi F, Gastaldi S, Perera T, Comoglio PM, et al: A preclinical algorithm of soluble surrogate biomarkers that correlate with therapeutic inhibition of the MET oncogene in gastric tumors. Int J Cancer 2012;130:1357–1366. Dinarello CA: Interleukin-1, interleukin-1 receptors and interleukin-1 receptor antagonist. Int Rev Immunol 1998;16:457–499. Goll R, Gruber F, Olsen T, Cui G, Raschpichler G, Buset M, et al: Helicobacter pylori stimulates a mixed adaptive immune response with a strong T-regulatory component in human gastric mucosa. Helicobacter 2007;12:185–192. Lindholm C, Quiding-Jarbrink M, Lonroth H, Hamlet A, Svennerholm AM: Local cytokine response in Helicobacter pylori-infected subjects. Infect Immun 1998;66:5964–5971. Kandulski A, Wex T, Kuester D, Peitz U, Gebert I, Roessner A, et al: Naturally occurring regulatory T cells (CD4+, CD25high, FOXP3+) in the antrum and cardia are associated with higher H. pylori colonization and increased gene expression of TGF-beta1. Helicobacter 2008;13:295–303. Perasso A, Testino G, de Angelis P, Augeri C, de Grandi R: Gastric chief cell mass in chronic gastritis. Count and relationships to parietal cell mass and functional indices. 165 166 167 168 169 170 171 172 173 174 175 176 Hepatogastroenterology 1991; 38(suppl 1): 63–66. Testino G: Parietal cell mass, hydrochloric acid secretion, and Helicobacter pylori. Am J Gastroenterol 1997;92:1070–1071. Kandulski A, Malfertheiner P, Wex T: Role of regulatory T-cells in H. pylori-induced gastritis and gastric cancer. Anticancer Res 2010;30:1093–1103. Jang S, Jones KR, Olsen CH, Joo YM, Yoo YJ, Chung IS, et al: Epidemiological link between gastric disease and polymorphisms in VacA and CagA. J Clin Microbiol 2010; 48: 559–567. Kindlund B, Sjoling A, Hansson M, Edebo A, Hansson LE, Sjovall H, et al: FOXP3-expressing CD4+ T-cell numbers increase in areas of duodenal gastric metaplasia and are associated to CD4+ T-cell aggregates in the duodenum of Helicobacter pylori-infected duodenal ulcer patients. Helicobacter 2009;14:192–201. Robinson K, Kenefeck R, Pidgeon EL, Shakib S, Patel S, Polson RJ, et al: Helicobacter pylori-induced peptic ulcer disease is associated with inadequate regulatory T cell responses. Gut 2008;57:1375–1385. Wang SK, Zhu HF, He BS, Zhang ZY, Chen ZT, Wang ZZ, et al: CagA+ H. pylori infection is associated with polarization of T helper cell immune responses in gastric carcinogenesis. World J Gastroenterol 2007;13: 2923–2931. Shen LS, Wang J, Shen DF, Yuan XL, Dong P, Li MX, et al: CD4+CD25+CD127low/– regulatory T cells express Foxp3 and suppress effector T cell proliferation and contribute to gastric cancers progression. Clin Immunol 2009;131:109–118. Enarsson K, Lundgren A, Kindlund B, Hermansson M, Roncador G, Banham AH, et al: Function and recruitment of mucosal regulatory T cells in human chronic Helicobacter pylori infection and gastric adenocarcinoma. Clin Immunol 2006;121:358–368. Li Q, Chen J, Liu Y, Zhao X, Tan B, Ai J, et al: Prevalence of Th17 and Treg cells in gastric cancer patients and its correlation with clinical parameters. Oncol Rep 2013; 30: 1215–1222. Perrone G, Ruffini PA, Catalano V, Spino C, Santini D, Muretto P, et al: Intratumoural FOXP3-positive regulatory T cells are associated with adverse prognosis in radically resected gastric cancer. Eur J Cancer 2008; 44: 1875–1882. Figueiredo C, Machado JC, Pharoah P, Seruca R, Sousa S, Carvalho R, et al: Helicobacter pylori and interleukin 1 genotyping: an opportunity to identify high-risk individuals for gastric carcinoma. J Natl Cancer Inst 2002;94:1680–1687. Hwang IR, Kodama T, Kikuchi S, Sakai K, Peterson LE, Graham DY, et al: Effect of interleukin 1 polymorphisms on gastric mucosal interleukin 1beta production in Helicobacter pylori infection. Gastroenterology 2002;123:1793–1803. Bornschein /Malfertheiner Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM 139 Zeng HM, Pan KF, Zhang Y, Zhang L, Ma JL, Zhou T, et al: Genetic variants of toll-like receptor 2 and 5, Helicobacter pylori infection, and risk of gastric cancer and its precursors in a Chinese population. Cancer Epidemiol Biomarkers Prev 2011; 20: 2594– 2602. 140 Wang P, Zhang L, Jiang JM, Ma D, Tao HX, Yuan SL, et al: Association of NOD1 and NOD2 genes polymorphisms with Helicobacter pylori related gastric cancer in a Chinese population. World J Gastroenterol 2012;18:2112–2220. 141 Furuta K, Arao T, Sakai K, Kimura H, Nagai T, Tamura D, et al: Integrated analysis of whole genome exon array and array-comparative genomic hybridization in gastric and colorectal cancer cells. Cancer Sci 2012; 103:221–227. 142 Zhang YZ, Zhang LH, Gao Y, Li CH, Jia SQ, Liu N, et al: Discovery and validation of prognostic markers in gastric cancer by genome-wide expression profiling. World J Gastroenterol 2011;17:1710–1717. 143 Rossi E, Klersy C, Manca R, Zuffardi O, Solcia E: Correlation between genomic alterations assessed by array comparative genomic hybridization, prognostically informative histologic subtype, stage, and patient survival in gastric cancer. Hum Pathol 2011; 42: 1937–1945. 144 Cui J, Li F, Wang G, Fang X, Puett JD, Xu Y: Gene-expression signatures can distinguish gastric cancer grades and stages. PLoS One 2011;6:e17819. 145 Kuroda A, Tsukamoto Y, Nguyen LT, Noguchi T, Takeuchi I, Uchida M, et al: Genomic profiling of submucosal-invasive gastric cancer by array-based comparative genomic hybridization. PLoS One 2011;6:e22313. 146 Deng N, Goh LK, Wang H, Das K, Tao J, Tan IB, et al: A comprehensive survey of genomic alterations in gastric cancer reveals systematic patterns of molecular exclusivity and co-occurrence among distinct therapeutic targets. Gut 2012;61:673–684. 147 Dulak AM, Schumacher SE, van Lieshout J, Imamura Y, Fox C, Shim B, et al: Gastrointestinal adenocarcinomas of the esophagus, stomach, and colon exhibit distinct patterns of genome instability and oncogenesis. Cancer Res 2012;72:4383–4393. 148 Wang YY, Ye ZY, Zhao ZS, Tao HQ, Li SG: Systems biology approach to identification of biomarkers for metastatic progression in gastric cancer. J Cancer Res Clin Oncol 2010; 136:135–141. 149 Ooi CH, Ivanova T, Wu J, Lee M, Tan IB, Tao J, et al: Oncogenic pathway combinations predict clinical prognosis in gastric cancer. PLoS Genet 2009;5:e1000676. 150 Shah MA, Khanin R, Tang L, Janjigian YY, Klimstra DS, Gerdes H, et al: Molecular classification of gastric cancer: a new paradigm. Clin Cancer Res 2011;17:2693–2701. 151 Wang G, Hu N, Yang HH, Wang L, Su H, Wang C, et al: Comparison of global gene H. pylori and Gastric Cancer 188 Bornschein J, Toth K, Selgrad M, Kuester D, Wex T, Molnar B, et al: Dysregulation of CDX1, CDX2 and SOX2 in patients with gastric cancer also affects the non-malignant mucosa. J Clin Pathol 2013;66:819–822. 189 Cinghu S, Goh YM, Oh BC, Lee YS, Lee OJ, Devaraj H, et al: Phosphorylation of the gastric tumor suppressor RUNX3 following H. pylori infection results in its localization to the cytoplasm. J Cell Physiol 2012;227:1071– 1080. 190 Liu Z, Xu X, Chen L, Li W, Sun Y, Zeng J, et al: Helicobacter pylori CagA inhibits the expression of Runx3 via Src/MEK/ERK and p38 MAPK pathways in gastric epithelial cell. J Cell Biochem 2012;113:1080–1086. 191 Zhou J, Xie Y, Zhao Y, Wang S, Li Y: Human gastrin mRNA expression up-regulated by Helicobacter pylori CagA through MEK/ ERK and JAK2-signaling pathways in gastric cancer cells. Gastric Cancer 2011; 14: 322– 331. 192 Wiedemann T, Hofbaur S, Tegtmeyer N, Huber S, Sewald N, Wessler S, et al: Helicobacter pylori CagL dependent induction of gastrin expression via a novel alphavbeta5integrin-integrin linked kinase signalling complex. Gut 2012;61:986–996. 193 Watson SA, Grabowska AM, El-Zaatari M, Takhar A: Gastrin – active participant or bystander in gastric carcinogenesis? Nat Rev Cancer 2006;6:936–946. 194 Takamura A, Ito M, Boda T, Matsumoto Y, Tanaka S, Yoshihara M, et al: High expression of gastrin receptor protein in injured mucosa of Helicobacter pylori-positive gastritis. Dig Dis Sci 2013;58:634–640. 195 Garcia-Zaragoza E, Hernandez C, Barrachina MD, Esplugues JV: Interleukin 1 beta-induced inhibition of gastric acid secretion involves glutamate, NO and cGMP synthesis in the brain. Naunyn Schmiedebergs Arch Pharmacol 2003;367:22–27. 196 Prinz C, Neumayer N, Mahr S, Classen M, Schepp W: Functional impairment of rat enterochromaffin-like cells by interleukin 1 beta. Gastroenterology 1997;112:364–375. 197 Deng J, Liang H, Zhang R, Sun D, Pan Y, Liu Y, et al: STAT3 is associated with lymph node metastasis in gastric cancer. Tumour Biol 2013;34:2791–2800. 198 Sierra JC, Hobbs S, Chaturvedi R, Yan F, Wilson KT, Peek RM Jr, et al: Induction of COX-2 expression by Helicobacter pylori is mediated by activation of epidermal growth factor receptor in gastric epithelial cells. Am J Physiol Gastrointest Liver Physiol 2013; 305:G196–G203. 199 Silva-Fernandes IJ, Alves MK, Lima VP, de Lima MA, Barros MA, Ferreira MV, et al: Differential expression of MYC in H. pylorirelated intestinal and diffuse gastric tumors. Virchows Arch 2011;458:725–731. Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 200 Targosz A, Brzozowski T, Pierzchalski P, Szczyrk U, Ptak-Belowska A, Konturek SJ, et al: Helicobacter pylori promotes apoptosis, activates cyclooxygenase (COX)-2 and inhibits heat shock protein HSP70 in gastric cancer epithelial cells. Inflamm Res 2012;61: 955–966. 201 Qinyu L, Long C, Zhen-Dong D, Min-Min S, Wei-Ze W, Wei-Ping Y, et al: FOXO6 promotes gastric cancer cell tumorigenicity via upregulation of C-myc. FEBS Lett 2013;587: 2105–2111. 202 Houghton J, Stoicov C, Nomura S, Rogers AB, Carlson J, Li H, et al: Gastric cancer originating from bone marrow-derived cells. Science 2004;306:1568–1571. 203 Uehara T, Ma D, Yao Y, Lynch JP, Morales K, Ziober A, et al: H. pylori infection is associated with DNA damage of Lgr5-positive epithelial stem cells in the stomach of patients with gastric cancer. Dig Dis Sci 2013; 58:140–149. 204 Varon C, Dubus P, Mazurier F, Asencio C, Chambonnier L, Ferrand J, et al: Helicobacter pylori infection recruits bone marrow-derived cells that participate in gastric preneoplasia in mice. Gastroenterology 2012;142:281–291. 205 Skoog EC, Sjoling A, Navabi N, Holgersson J, Lundin SB, Linden SK: Human gastric mucins differently regulate Helicobacter pylori proliferation, gene expression and interactions with host cells. PLoS One 2012;7:e36378. 206 Fuccio L, Zagari RM, Eusebi LH, Laterza L, Cennamo V, Ceroni L, et al: Meta-analysis: can Helicobacter pylori eradication treatment reduce the risk for gastric cancer? Ann Intern Med 2009;151:121–128. 207 Take S, Mizuno M, Ishiki K, Nagahara Y, Yoshida T, Yokota K, et al: The effect of eradicating Helicobacter pylori on the development of gastric cancer in patients with peptic ulcer disease. Am J Gastroenterol 2005;100:1037–1042. 208 Wong BC, Lam SK, Wong WM, Chen JS, Zheng TT, Feng RE, et al: Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trial. JAMA 2004;291:187–194. 209 Kamada T, Hata J, Sugiu K, Kusunoki H, Ito M, Tanaka S, et al: Clinical features of gastric cancer discovered after successful eradication of Helicobacter pylori: results from a 9-year prospective follow-up study in Japan. Aliment Pharmacol Ther 2005;21:1121–1126. 210 Take S, Mizuno M, Ishiki K, Nagahara Y, Yoshida T, Yokota K, et al: Baseline gastric mucosal atrophy is a risk factor associated with the development of gastric cancer after Helicobacter pylori eradication therapy in patients with peptic ulcer diseases. J Gastroenterol 2007;42(suppl 17):21–27. 211 Weck MN, Brenner H: Association of Helicobacter pylori infection with chronic atrophic gastritis: meta-analyses according to type of disease definition. Int J Cancer 2008; 123:874–881. 263 Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM 177 Furuta T, El-Omar EM, Xiao F, Shirai N, Takashima M, Sugimura H: Interleukin 1beta polymorphisms increase risk of hypochlorhydria and atrophic gastritis and reduce risk of duodenal ulcer recurrence in Japan. Gastroenterology 2002;123:92–105. 178 Vilaichone RK, Mahachai V, Tumwasorn S, Wu JY, Graham DY, Yamaoka Y: Gastric mucosal cytokine levels in relation to host interleukin-1 polymorphisms and Helicobacter pylori cagA genotype. Scand J Gastroenterol 2005;40:530–539. 179 Chang YW, Jang JY, Kim NH, Lee JW, Lee HJ, Jung WW, et al: Interleukin-1B (IL-1B) polymorphisms and gastric mucosal levels of IL1beta cytokine in Korean patients with gastric cancer. Int J Cancer 2005;114:465–471. 180 Allison CC, Ferrand J, McLeod L, Hassan M, Kaparakis-Liaskos M, Grubman A, et al: Nucleotide oligomerization domain 1 enhances IFN-gamma signaling in gastric epithelial cells during Helicobacter pylori infection and exacerbates disease severity. J Immunol 2013;190:3706–3715. 181 Pimentel-Nunes P, Goncalves N, Boal-Carvalho I, Afonso L, Lopes P, Roncon-Albuquerque R Jr, et al: Helicobacter pylori induces increased expression of Toll-like receptors and decreased Toll-interacting protein in gastric mucosa that persists throughout gastric carcinogenesis. Helicobacter 2013; 18:22–32. 182 Kumar Pachathundikandi S, Brandt S, Madassery J, Backert S: Induction of TLR-2 and TLR-5 expression by Helicobacter pylori switches cagPAI-dependent signalling leading to the secretion of IL-8 and TNF-alpha. PLoS One 2011;6:e19614. 183 Lagunes-Servin H, Torres J, MaldonadoBernal C, Perez-Rodriguez M, HuertaYepez S, Madrazo de la Garza A, et al: Tolllike receptors and cytokines are upregulated during Helicobacter pylori infection in children. Helicobacter 2013;18:423–432. 184 Sakitani K, Hirata Y, Hayakawa Y, Serizawa T, Nakata W, Takahashi R, et al: Role of interleukin-32 in Helicobacter pylori-induced gastric inflammation. Infect Immun 2012; 80:3795–3803. 185 Kim DJ, Park JH, Franchi L, Backert S, Nunez G: The Cag pathogenicity island and interaction between TLR2/NOD2 and NLRP3 regulate IL-1beta production in Helicobacter pylori infected dendritic cells. Eur J Immunol 2013;43:2650–2658. 186 Tsai YC, Hsiao WH, Yang HB, Cheng HC, Chang WL, Lu CC, et al: The corpus-predominant gastritis index may serve as an early marker of Helicobacter pylori-infected patients at risk of gastric cancer. Aliment Pharmacol Ther 2013;37:969–978. 187 Peleteiro B, Lunet N, Wen X, Afonso LP, Mendes N, Barros R, et al: Association between environmental factors and CDX2 expression in gastric cancer patients. Eur J Cancer Prev 2012;21:423–431. 264 Dig Dis 2014;32:249–264 DOI: 10.1159/000357858 224 Ohkusa T, Fujiki K, Takashimizu I, Kumagai J, Tanizawa T, Eishi Y, et al: Improvement in atrophic gastritis and intestinal metaplasia in patients in whom Helicobacter pylori was eradicated. Ann Intern Med 2001; 134: 380– 386. 225 Sugiyama T, Sakaki N, Kozawa H, Sato R, Fujioka T, Satoh K, et al: Sensitivity of biopsy site in evaluating regression of gastric atrophy after Helicobacter pylori eradication treatment. Aliment Pharmacol Ther 2002; 16(suppl 2):187–190. 226 Wu CY, Kuo KN, Wu MS, Chen YJ, Wang CB, Lin JT: Early Helicobacter pylori eradication decreases risk of gastric cancer in patients with peptic ulcer disease. Gastroenterology 2009;137:1641–1648 e1–2. 227 Fukase K, Kato M, Kikuchi S, Inoue K, Uemura N, Okamoto S, et al: Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet 2008;372:392–397. 228 Maehata Y, Nakamura S, Fujisawa K, Esaki M, Moriyama T, Asano K, et al: Long-term effect of Helicobacter pylori eradication on the development of metachronous gastric cancer after endoscopic resection of early gastric cancer. Gastrointest Endosc 2012;75:39–46. 229 Osborn JF, Cattaruzza MS, Ferri AM, De Angelis F, Renzi D, Marani A, et al: How long will it take to reduce gastric cancer incidence by eradicating Helicobacter pylori infection? Cancer Prev Res (Phila) 2013; 6: 695–700. 230 Graham DY, Shiotani A: The time to eradicate gastric cancer is now. Gut 2005;54:735– 738. 231 Fuccio L, Eusebi LH, Zagari RM, Bazzoli F: Helicobacter pylori eradication treatment reduces but does not abolish the risk of gastric cancer. Am J Gastroenterol 2009; 104: 3100; author reply 1–2. 232 de Vries AC, Kuipers EJ, Rauws EA: Helicobacter pylori eradication and gastric cancer: when is the horse out of the barn? Am J Gastroenterol 2009;104:1342–1345. 233 Cannizzaro R, De Paoli P: Helicobacter pylori eradication, endoscopic surveillance, and gastric cancer. Am J Gastroenterol 2009; 104:3100–3101; author reply 1–2. 234 Malfertheiner P, Megraud F, O’Morain CA, Atherton J, Axon AT, Bazzoli F, et al: Management of Helicobacter pylori infection – the Maastricht IV/ Florence Consensus Report. Gut 2012;61:646–664. 235 Dinis-Ribeiro M, Areia M, de Vries AC, Marcos-Pinto R, Monteiro-Soares M, O’Connor A, et al: Management of precancerous conditions and lesions in the stomach (MAPS): guideline from the European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter Study Group (EHSG), European Society of Pathology (ESP), and the Sociedade Portuguesa de Endoscopia Digestiva (SPED). Endoscopy 2012;44:74–94. 236 Areia M, Carvalho R, Cadime AT, Rocha Goncalves F, Dinis-Ribeiro M: Screening for gastric cancer and surveillance of premalignant lesions: a systematic review of cost-effectiveness studies. Helicobacter 2013; 18: 325–337. 237 Ruiz B, Garay J, Correa P, Fontham ET, Bravo JC, Bravo LE, et al: Morphometric evaluation of gastric antral atrophy: improvement after cure of Helicobacter pylori infection. Am J Gastroenterol 2001;96:3281–3287. 238 Lu B, Chen MT, Fan YH, Liu Y, Meng LN: Effects of Helicobacter pylori eradication on atrophic gastritis and intestinal metaplasia: a 3-year follow-up study. World J Gastroenterol 2005;11:6518–6520. 239 Lee YC, Chen TH, Chiu HM, Shun CT, Chiang H, Liu TY, et al: The benefit of mass eradication of Helicobacter pylori infection: a community-based study of gastric cancer prevention. Gut 2013;62:676–682. 240 You WC, Brown LM, Zhang L, Li JY, Jin ML, Chang YS, et al: Randomized double-blind factorial trial of three treatments to reduce the prevalence of precancerous gastric lesions. J Natl Cancer Inst 2006;98:974–983. 241 Ito M, Haruma K, Kamada T, Mihara M, Kim S, Kitadai Y, et al: Helicobacter pylori eradication therapy improves atrophic gastritis and intestinal metaplasia: a 5-year prospective study of patients with atrophic gastritis. Aliment Pharmacol Ther 2002; 16: 1449–1456. 242 Yamada T, Miwa H, Fujino T, Hirai S, Yokoyama T, Sato N: Improvement of gastric atrophy after Helicobacter pylori eradication therapy. J Clin Gastroenterol 2003; 36: 405– 410. 243 Maehata Y, Nakamura S, Fujisawa K, Esaki M, Moriyama T, Asano K, et al: Long-term effect of Helicobacter pylori eradication on the development of metachronous gastric cancer after endoscopic resection of early gastric cancer. Gastrointest Endosc 2012;75: 39–46. 244 Zhou LY, Lin SR, Ding SG, Huang XB, Zhang L, Meng LM, et al: The changing trends of the incidence of gastric cancer after Helicobacter pylori eradication in Shandong area. Chin J Dig Dis 2005;6:114–115. 245 Saito K, Arai K, Mori M, Kobayashi R, Ohki I: Effect of Helicobacter pylori eradication on malignant transformation of gastric adenoma. Gastrointest Endosc 2000;52:27–32. 246 Leung WK, Lin SR, Ching JY, To KF, Ng EK, Chan FK, et al: Factors predicting progression of gastric intestinal metaplasia: results of a randomised trial on Helicobacter pylori eradication. Gut 2004;53:1244–1249. Bornschein /Malfertheiner Downloaded by: NYU Medical Center Library 128.122.253.228 - 4/23/2015 5:31:58 AM 212 Ohata H, Kitauchi S, Yoshimura N, Mugitani K, Iwane M, Nakamura H, et al: Progression of chronic atrophic gastritis associated with Helicobacter pylori infection increases risk of gastric cancer. Int J Cancer 2004;109:138–143. 213 Cassaro M, Rugge M, Gutierrez O, Leandro G, Graham DY, Genta RM: Topographic patterns of intestinal metaplasia and gastric cancer. Am J Gastroenterol 2000; 95: 1431– 1438. 214 de Vries AC, van Grieken NC, Looman CW, Casparie MK, de Vries E, Meijer GA, et al: Gastric cancer risk in patients with premalignant gastric lesions: a nationwide cohort study in the Netherlands. Gastroenterology 2008;134:945–952. 215 Domellof L: Reversal of gastric atrophy after Helicobacter pylori eradication: is it possible or not? Am J Gastroenterol 1998; 93: 1407– 1408. 216 Uemura N, Mukai T, Okamoto S, Yamaguchi S, Mashiba H, Taniyama K, et al: Effect of Helicobacter pylori eradication on subsequent development of cancer after endoscopic resection of early gastric cancer. Cancer Epidemiol Biomarkers Prev 1997;6:639– 642. 217 Sung JJ, Lin SR, Ching JY, Zhou LY, To KF, Wang RT, et al: Atrophy and intestinal metaplasia one year after cure of H. pylori infection: a prospective, randomized study. Gastroenterology 2000;119:7–14. 218 Cho SJ, Choi IJ, Kook MC, Yoon H, Park S, Kim CG, et al: Randomised clinical trial: the effects of Helicobacter pylori eradication on glandular atrophy and intestinal metaplasia after subtotal gastrectomy for gastric cancer. Aliment Pharmacol Ther 2013;38:477–489. 219 Salih BA, Abasiyanik MF, Saribasak H, Huten O, Sander E: A follow-up study on the effect of Helicobacter pylori eradication on the severity of gastric histology. Dig Dis Sci 2005;50:1517–1522. 220 Schenk BE, Kuipers EJ, Nelis GF, Bloemena E, Thijs JC, Snel P, et al: Effect of Helicobacter pylori eradication on chronic gastritis during omeprazole therapy. Gut 2000; 46: 615–621. 221 Rokkas T, Pistiolas D, Sechopoulos P, Robotis I, Margantinis G: The long-term impact of Helicobacter pylori eradication on gastric histology: a systematic review and meta-analysis. Helicobacter 2007; 12(suppl 2):32–38. 222 Wang J, Xu L, Shi R, Huang X, Li SW, Huang Z, et al: Gastric atrophy and intestinal metaplasia before and after Helicobacter pylori eradication: a meta-analysis. Digestion 2011;83:253–260. 223 Lee YC, Chen TH, Chiu HM, Shun CT, Chiang H, Liu TY, et al: The benefit of mass eradication of Helicobacter pylori infection: a community-based study of gastric cancer prevention. Gut 2013;62:676–682.