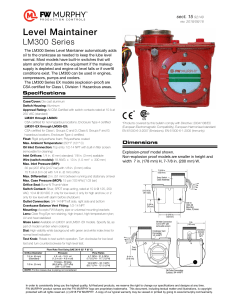
DOI: 10.5301/ejo.5000005 Eur J Ophthalmol 2011 ; 21 ( 6): 826-829 CASE REPORT Prevention of hyperopic surprise after LASIK in patients with refractive multifocal intraocular lenses César Albarrán-Diego1, Gonzalo Muñoz1, Teresa Ferrer-Blasco2, Santiago García-Lázaro2 Refractive Surgery Department, Marqués de Sotelo Ophthalmological Center and Hospital NISA Valencia al Mar, Valencia - Spain 2 Optometry Research Group (G.I.O.), Department of Optics, University of Valencia, Valencia - Spain 1 Refractive Surgery Department, Marqués de Sotelo Ophthalmological Center and Hospital NISA Valencia al Mar, Valencia - Spain Optometry Research Group (G.I.O.), Department of Optics, University of Valencia, Valencia - Spain Purpose. Three cases of patients who developed a similar hyperopic defect in refraction following laser in situ keratomileusis (LASIK) after multifocal intraocular lens (IOL) implantation are described. Methods. Ophthalmologic evaluation including refractive status, corrected and uncorrected visual acuity (both at far and near), and corneal topography in patients presenting similar hyperopic refractive surprise in one eye as a result of LASIK refinement of residual ametropia after refractive multifocal IOL implantation. Results. Laser in situ keratomileusis enhancement for residual ametropia of –1.00 to –1.50 D in patients with a prior implantation of refractive multifocal IOL resulted in a refractive surprise of +2.25 to +2.50 D. After excluding other possible sources of error, an explanation for such a refractive surprise is suggested, and a simple method for avoiding this error is presented. Conclusions. Proper knowledge of the defocus curve and the use of a systematic method for determining subjective refraction in patients implanted with refractive multifocal IOLs will reduce the possibility of refractive surprise after LASIK enhancement in a bioptics procedure. Key Words. Defocus curve, LASIK, Refractive multifocal IOL, Refractive surprise Accepted: May 12, 2011 INTRODUCTION Multifocal intraocular lenses (IOLs) are designed to reduce dependence on eyeglasses after cataract surgery or clear lens extraction. Refractive multifocal IOLs use surfaces of different optical power to provide multifocality. The ReZoom IOL (Abbott Medical Optics, Santa Ana, CA) uses 5 concentric rings of varying optical power. The near addition of the lens is +3.5 D at the lens plane which results in approximately +2.6 D at the glasses plane. The ReZoom lens has been developed from the previous Array multifocal IOL providing better image quality particularly at distant focus (6). The ReZoom lens has been widely used alone or in combination with diffractive multifocal IOLs in the mix and match technique. 826 The Lentis Mplus IOL (Oculentis GmbH, Berlin) is a onepiece refractive multifocal lens made of hydrosmart with an aspheric posterior surface. The multifocality is achieved by implementing a distance part and a distinct near sector of +3.0 D in the lower IOL segment, comparable to a bifocal spectacle lens. In general, patients implanted with multifocal IOLs are less dependent on eyeglasses, but it is often necessary to combine multifocal IOL with other refractive techniques such as laser in situ keratomileusis (LASIK) to achieve optimum results in the so-called bioptics approach (1). In bioptics, IOL implantation is followed by corneal refractive surgery so that the greatest amount of ametropia is corrected with the lens and the residual refraction is treated on the cornea taking advantage of the precision of the excimer laser correction. © 2011 Wichtig Editore - ISSN 1120-6721 Albarrán-Diego et al In the present report, 3 patients who developed a hyperopic defect in refraction following LASIK in eyes containing a ReZoom multifocal IOL (2 eyes) or a Lentis Mplus multifocal IOL (1 eye) are described and discussed. Case reports Two patients presenting a hyperopic surprise after LASIK in one eye were referred to the clinic for a second opinion. A similar patient who presented consecutive hyperopia after LASIK for low residual myopia after clear lens extraction with multifocal IOL implantation had been previously seen. The 3 eyes shared the presence of a refractive multifocal IOL: ReZoom IOL (2 eyes) and Lentis Mplus IOL (1 eye). The characteristics of the 3 eyes involved in the present report are summarized in Table I. Case 1 A 56-year-old woman had LASIK in her right eye 1 month after cataract surgery with a ReZoom multifocal IOL of +27.0 D implanted. Before LASIK, corrected distance visual acuity (CDVA) was 20/25 with –1.25 –0.50 × 175º. Automated refraction was –0.75 –075 × 175º. Near vision was not measured at that time. Topography was within normal limits with a mean keratometry of 44.1 D and central ultrasonic pachymetry was 522 µm. Laser in situ keratomileusis flap was created using an Amadeus II microkeratome (Ziemer Ophthalmics Systems AG) with a nasally placed hinge. Ablation was performed with the Visx S4 Star excimer laser (Abbott Medical Optics). The procedure was uneventful, but 24 hours postoperatively the patient showed an uncorrected distance visual acuity (UCDVA) of 20/60 corrected to 20/20 with +2.50 D. Uncorrected near visual acuity (UCNVA) was very poor at 20/200 and best distancecorrected near visual acuity (BDCNVA) was 20/30. Topography showed a well-centered myopic ablation and mean keratometry of 42.9 D. Refraction remained stable through the following months. Case 2 A 53-year-old man had LASIK done in the right eye after clear lens extraction with implantation of a Lentis Mplus MIOL of 17.5 D. Before LASIK, CDVA was 20/25 with –1.00 D. Automated refraction was not reliable, offering values that ranged between +0.50 and –1.50 D for the sphere and variable cylinder both in magnitude and axis. No data about near vision were available. Topography was normal and showed a mean keratometry of 45.3 D. Central ultrasonic pachymetry was 589 µm. Laser in situ keratomileusis flap was created with a Moria One microkeratome (Moria) with a nasally placed hinge, and ablation was performed with a Technolas 217z100 excimer laser (Bausch & Lomb). One week postoperatively, the patient showed UCDVA of 20/30 corrected to 20/20 with +2.25 D, and refraction remained stable since. Uncorrected near vision was 20/100 whereas BDCNVA achieved 20/25. Postoperative topography showed a well-centered myopic ablation and mean keratometry of 44.4 D. Case 3 A 56-year-old woman had LASIK in her left eye after clear lens extraction with a ReZoom MIOL of 28.0 D implanted. Preoperative CDVA was 20/32 with –1.25 –0.25 × 90º. Au- TABLE I - CHARACTERISTICS OF THE 3 EYES CONTAINING A REFRACTIVE MULTIFOCAL INTRAOCULAR LENS (IOL) THAT PRESENTED A HYPEROPIC OUTCOME AFTER LASER IN SITU KERATOMILEUSIS (LASIK) Case no. Age, y Eye Multifocal Preop K Preop IOL (power) pachymetry Pre-LASIK subjective refraction Microkeratome/ excimer laser Postop K Postop Post-LASIK pachymetry subjective refraction 1 56 R ReZoom (27.0) 44.1 522 –1.25 –0.50 × 175º Amadeus II/Visx S4 Star 42.9 501 +2.50 2 53 R Lentis Mplus (17.5) 45.3 589 –1 Moria One/Technolas 217z100 44.4 573 +2.25 3 56 L ReZoom (28.0) 43.3 543 –1.25 –0.25 × 90º Carriazo-Barraquer/Visx S2 Star 41.9 538 +2.25 © 2011 Wichtig Editore - ISSN 1120-6721 827 Defocus curve analysis as a help in subjective refraction Fig. 1 - Defocus curves for the two refractive bifocal intraocular lenses (solid line for the AMO ReZoom and dashed line for the Oculentis M-Plus). A is the far focus and B is the near focus of the IOL. Refraction for far can be achieved using both foci of the lens. If B is used for far vision, refraction will be -2.50 D more myopic than the real refraction using A. If a corneal excimer procedure is performed based on the refraction obtained with B, the patient will develop yatrogenic secondary hyperopia. Units are in Snellen decimal notation for visual acuity and diopters for defocus. tomated refraction was –0.75 –075 × 90º. Near vision had not been tested. Topography was normal with mean keratometry of 43.3 D and central ultrasonic pachymetry was 543 µm. Laser in situ keratomileusis flap was created with a Carriazo-Barraquer microkeratome (Moria) with a superior hinge. Ablation was performed with the Visx S2 Star excimer laser (Abbott Medical Optics). One week after the procedure, the patient showed UCDVA of 20/50 corrected to 20/20 with +2.25 D, UCNVA of 20/200, and BDCNVA of 20/30. Refraction remained stable throughout the following months. DISCUSSION Three cases of 3 patients who developed a hyperopic surprise after LASIK in eyes implanted with a refractive multifocal IOL are reported. Subjective refraction before LASIK ranged between –1.00 and –1.50 D spherical equivalent achieving a CDVA ranging between 20/32 and 20/25. After otherwise uneventful myopic LASIK, the 3 patients presented a hyperopic outcome ranging between +2.25 and 828 +2.50 D achieving a CDVA of 20/20 in every case. Retrospective examination of ablation reports (and keratometric change achieved with LASIK procedures) performed in the 3 cases excluded other possible sources of error. The following explanation for the hyperopic outcome in the 3 cases described is proposed: subjective refraction for CDVA was achieved using the near focus of the multifocal IOL, so that the eyes were not really myopic of –1.00 to –1.50 D, but hyperopic of +1.00 to +1.50 D. Hence, the myopic treatment resulted in a more hyperopic residual defect. It must be kept in mind that in the presence of a multifocal IOL far vision can be corrected by using the 2 principal foci of the IOL, but only if the far focus is in focus for far vision will the near focus be useful for near vision. If the near focus is in focus for far vision, obviously the near focus does not provide useful near vision. The subjective refraction value when using the near focus for far vision is equal to the real refractive error minus the addition of the IOL for near vision, which is between +2.25 and +2.50 D at the spectacle plane depending upon the multifocal IOL design and power (Fig. 1). For instance, for a patient with a real –1.00 D of myopia after refractive multifocal IOL implantation DCVA can be achieved using a –1.00 D (point A in Figure 1: far focus in focus for far and near focus in focus for near) or using a –3.25 D (point B in Figure 1: far focus out focus for far and near focus in focus for far and out focus for near); for a patient with a real +1.00 D of hyperopia after refractive multifocal IOL implantation DCVA can be achieved using a +1.00 D (point A in Figure 1: far focus in focus for far and near focus in focus for near) or using a –1.25 D (point B in Figure 1: far focus out focus for far and near focus in focus for far and out focus for near). Subjective refraction remains the method of choice for determining the refractive status after surgery with IOLs including multifocal; however, it can be time consuming and requires trained technicians. Automated refraction and retinoscopy can be used to determine the start point for subjective refraction (2, 3). In the general population retinoscopy is superior to automated refraction (4) but it requires experienced clinicians, while automated refraction does not. It has been previously reported (5, 6) that automated refraction in eyes with refractive multifocal IOLs shows some kind of instrument myopia which is a false tendency towards more negative spherical values compared to manifest refraction of approximately 1 D. Therefore great caution should be exercised when autorefraction is carried out in eyes implanted with refractive multifocal IOL. © 2011 Wichtig Editore - ISSN 1120-6721 Albarrán-Diego et al In order to prevent this unwanted outcome after LASIK enhancement of a refractive multifocal IOL procedure, it is necessary to be sure that the far focus of the multifocal IOL is the one that the patient is using for distance vision in subjective refraction. The following 3-step technique to prevent this complication is proposed: 1) Once CDVA is achieved, near vision should always be tested using the far refraction, which is BDCNVA. If BDCNVA is not within the expected values for the IOL, the possibility of having used the near focus of the IOL for far vision correction must be considered. However, in patients implanted with refractive multifocal IOLs, UCNVA and BDCNVA improve over time by a neuroadaptation process in which the brain reduces the noise-to-signal ratio produced by multifocality (7). This means that poor distance-corrected near vision does not always mean that refraction was performed using the near focus for distance. This step may be therefore not very practical sometimes, so the following steps may be used. 2) Once CDVA is achieved, a +2.25 or +2.50 lens is placed on top of it and distance vision tested again. If CDVA decreases to 20/100 or below, subjective refraction was achieved using the far focus of the IOL and was correct. If CDVA does not fall but remains similar or even increases, CDVA was achieved with the near focus of the multifocal IOL and was accordingly a wrong refraction for far vision. 3) Once CDVA is achieved, a –2.25 or –2.50 lens is placed on top of it and distance vision tested again. If CDVA falls to 20/100 or less, refraction was wrong and the patient was using the near focus of the multifocal IOL for distance. If CDVA remains similar or decreases 1–2 lines, refraction was right and the patient was using the far focus of the multifocal IOL for distance. It is of utmost importance to be familiar with the defocus curve of the multifocal IOL being used (Fig. 1). In the case of refractive multifocal IOL the 2 peaks of maximum visual acuity are separated by +2.25 to +2.50 D, while in the case of diffractive multifocal IOLs both peaks are separated further and hence addition of +2.75 to +3 D (or –2.75 to –3 D) should be used in steps 2 and 3, respectively (or even 3.25 D). In summary, in the presence of a refractive multifocal IOL, it is mandatory to test BDCNVA once subjective refraction for far has finished. If near vision with distance refraction is not within the expected values for the specific IOL, the possibility of having used the near focus of the IOL to provide far vision should be ruled out. This research was supported in part by Ministerio de Ciencia e Innovación Research grants (SAF2008-01114 and SAF2009-13342). The authors report no proprietary interest. Address for correspondence: César Albarrán-Diego Centro Oftalmológico Marqués de Sotelo Avda. Marqués de Sotelo 5, planta 2ª 46002 Valencia Spain cesar.albarran@gmail.com REFERENCES 1. 2. 3. 4. 5. 6. 7. Zaldivar R, Davidorf JM, Oscherow S, Ricur G, Piezzi V. Combined posterior chamber phakic intraocular lens and laser in situ keratomileusis: bioptics for extreme myopia. J Refract Surg 1999; 15: 299-308. Goss DA, Grosvenor T. Reliability of refraction: a literature review. J Am Optom Assoc 1996; 67: 619-30. Bullimore MA, Fusaro RE, Adams CW. The repeatability of automated and clinician refraction. Optom Vis Sci 1998; 75: 617-22. Jorge J, Queirós A, Almeida JB, Parafita MA. Retinoscopy/ autorefraction: which is the best starting point for a noncycloplegic refraction? Optom Vis Sci 2005; 82: 64-8. Muñoz G, Albarrán-Diego C, Sakla HF. Validity of autorefraction after cataract surgery with multifocal ReZoom intraocular lens implantation. J Cataract Refract Surg 2007; 33: 1573-8. Muñoz G, Albarrán-Diego C, Sakla HF. Autorefraction after multifocal IOLs. Ophthalmology 2007; 114: 2100. Montés-Micó R, Alió JL. Distance and near contrast sensitivity function after multifocal intraocular lens implantation. J Cataract Refract Surg 2003; 29: 703-11. © 2011 Wichtig Editore - ISSN 1120-6721 829