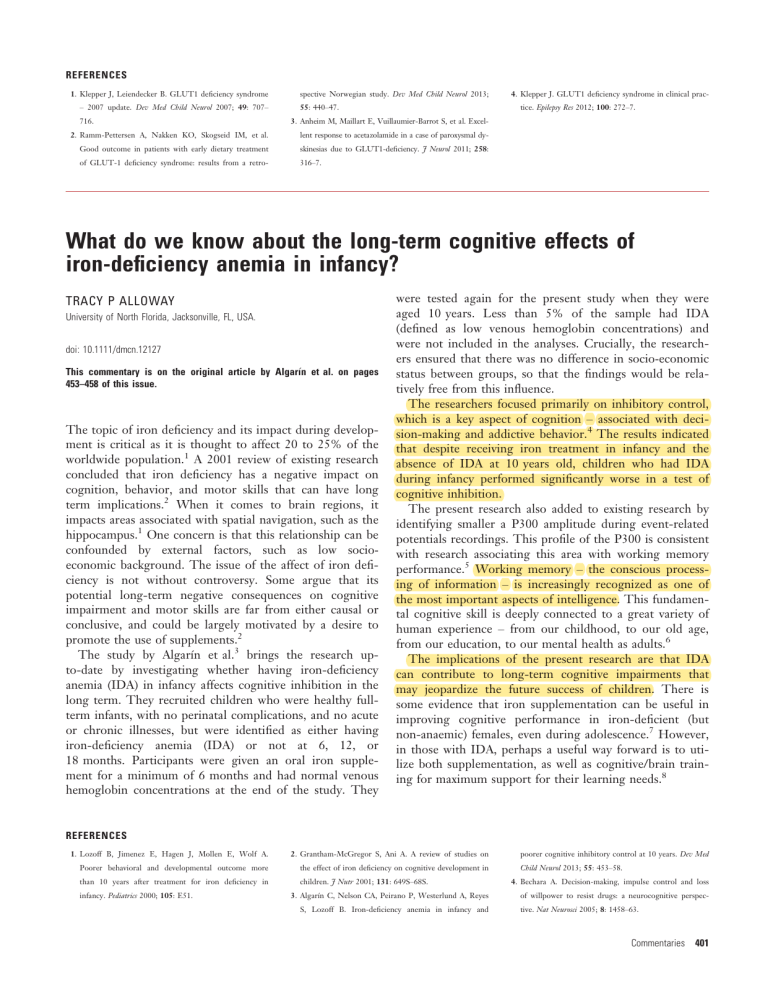
REFERENCES 1. Klepper J, Leiendecker B. GLUT1 deficiency syndrome – 2007 update. Dev Med Child Neurol 2007; 49: 707– 716. spective Norwegian study. Dev Med Child Neurol 2013; 4. Klepper J. GLUT1 deficiency syndrome in clinical practice. Epilepsy Res 2012; 100: 272–7. 55: 440–47. 3. Anheim M, Maillart E, Vuillaumier-Barrot S, et al. Excel- 2. Ramm-Pettersen A, Nakken KO, Skogseid IM, et al. lent response to acetazolamide in a case of paroxysmal dy- Good outcome in patients with early dietary treatment skinesias due to GLUT1-deficiency. J Neurol 2011; 258: of GLUT-1 deficiency syndrome: results from a retro- 316–7. What do we know about the long-term cognitive effects of iron-deficiency anemia in infancy? TRACY P ALLOWAY University of North Florida, Jacksonville, FL, USA. doi: 10.1111/dmcn.12127 This commentary is on the original article by Algarın et al. on pages 453–458 of this issue. The topic of iron deficiency and its impact during development is critical as it is thought to affect 20 to 25% of the worldwide population.1 A 2001 review of existing research concluded that iron deficiency has a negative impact on cognition, behavior, and motor skills that can have long term implications.2 When it comes to brain regions, it impacts areas associated with spatial navigation, such as the hippocampus.1 One concern is that this relationship can be confounded by external factors, such as low socioeconomic background. The issue of the affect of iron deficiency is not without controversy. Some argue that its potential long-term negative consequences on cognitive impairment and motor skills are far from either causal or conclusive, and could be largely motivated by a desire to promote the use of supplements.2 The study by Algarın et al.3 brings the research upto-date by investigating whether having iron-deficiency anemia (IDA) in infancy affects cognitive inhibition in the long term. They recruited children who were healthy fullterm infants, with no perinatal complications, and no acute or chronic illnesses, but were identified as either having iron-deficiency anemia (IDA) or not at 6, 12, or 18 months. Participants were given an oral iron supplement for a minimum of 6 months and had normal venous hemoglobin concentrations at the end of the study. They were tested again for the present study when they were aged 10 years. Less than 5% of the sample had IDA (defined as low venous hemoglobin concentrations) and were not included in the analyses. Crucially, the researchers ensured that there was no difference in socio-economic status between groups, so that the findings would be relatively free from this influence. The researchers focused primarily on inhibitory control, which is a key aspect of cognition – associated with decision-making and addictive behavior.4 The results indicated that despite receiving iron treatment in infancy and the absence of IDA at 10 years old, children who had IDA during infancy performed significantly worse in a test of cognitive inhibition. The present research also added to existing research by identifying smaller a P300 amplitude during event-related potentials recordings. This profile of the P300 is consistent with research associating this area with working memory performance.5 Working memory – the conscious processing of information – is increasingly recognized as one of the most important aspects of intelligence. This fundamental cognitive skill is deeply connected to a great variety of human experience – from our childhood, to our old age, from our education, to our mental health as adults.6 The implications of the present research are that IDA can contribute to long-term cognitive impairments that may jeopardize the future success of children. There is some evidence that iron supplementation can be useful in improving cognitive performance in iron-deficient (but non-anaemic) females, even during adolescence.7 However, in those with IDA, perhaps a useful way forward is to utilize both supplementation, as well as cognitive/brain training for maximum support for their learning needs.8 REFERENCES 1. Lozoff B, Jimenez E, Hagen J, Mollen E, Wolf A. 2. Grantham-McGregor S, Ani A. A review of studies on Poorer behavioral and developmental outcome more the effect of iron deficiency on cognitive development in than 10 years after treatment for iron deficiency in children. J Nutr 2001; 131: 649S–68S. infancy. Pediatrics 2000; 105: E51. 3. Algarın C, Nelson CA, Peirano P, Westerlund A, Reyes S, Lozoff B. Iron-deficiency anemia in infancy and poorer cognitive inhibitory control at 10 years. Dev Med Child Neurol 2013; 55: 453–58. 4. Bechara A. Decision-making, impulse control and loss of willpower to resist drugs: a neurocognitive perspective. Nat Neurosci 2005; 8: 1458–63. Commentaries 401 5. Patel SH, Azzam PN. Characterization of N200 and 7. Bruner AB, Joffe A, Duggan AK, Casella J, Brandt J. 8. Alloway TP, Bibile V, Lau G. Computerized working P300: selected studies of the Event-Related Potential. Randomised study of cognitive effects of iron supple- memory training: can it lead to gains in cognitive skills Int J Med Sci 2005; 2: 147–54. mentation in non-anaemic iron-deficient adolescent in 2 students? Comput Hum Behav 2013; 29: 632–638. 6. Alloway TP, Alloway RG. Working Memory: The Con- girls. Lancet 1996; 348: 992–6. nected Intelligence. New York: Psychology Press, 2012. Proper stratification of survival curves by level of gross motor function STEVEN M DAY Mortality Research and Consulting Inc., Newport Beach, CA, USA. doi: 10.1111/dmcn.12136 This commentary is on the original article by Touyama et al. on pages 459–463 of this issue. Touyama et al. report on long-term survival of cerebral palsy (CP) in Okinawa, Japan.1 The authors stratified Kaplan-Meier survival curves by Gross Motor Function Classification System (GMFCS) level.2 Stratification by GMFCS level is valuable for two reasons: (1) level of gross motor function is a strong predictor of long-term survival in CP; and (2) the GMFCS is a validated and widely employed measure of gross motor functioning in CP. Proper stratification by GMFCS level could allow for more meaningful between-study comparisons of survival. Unfortunately, the method of stratification in various studies may make comparisons of survival curves problematic. In Touyama et al.1 GMFCS level was ascertained ‘as closely as possible to the follow-up termination date’ of their study, whereas follow-up began at age 2. If GMFCS level is determined at an older age and then groups are formed at age 2 on this basis, a bias in the Kaplan-Meier survival analysis may result. It is not clear in which direction this bias may work. I will consider two extreme (hypothetical) possibilities to illustrate the point. First, suppose that every 2-year-old child with CP who lives long enough eventually is at GMFCS level V and remains so thereafter. In this case, late ascertainment of GMFCS level would bias survival estimates for 2-year-olds at GMFCS level V toward longer survival. This is because children of all GMFCS levels (at age 2) would be included in the analysis, and survival is undoubtedly better for 2-year-olds at a GMFCS lower than level V. Furthermore, children who died before reaching GMFCS level V would be excluded from the analysis. Thus, not only would higher functioning children be included in the analysis, but many who died would be excluded. 402 Developmental Medicine & Child Neurology 2013, 55: 397–404 Another extreme possibility is that all children at GMFCS level V who live long enough eventually improve to one of levels I to IV. In this case, late ascertainment of GMFCS level would bias results for 2-year-olds at GMFCS level V toward shorter survival: only children who died before improving or who never improved during the follow-up period would contribute to the analysis. A third possibility is that GMFCS level is stable over a child’s lifespan. In this case, the timing of ascertainment of GMFCS level would not matter. The truth lies somewhere between the two extremes: over time, some 2-year-olds at GMFCS levels I to IV will decline to level V, and some initially at GMFCS level V will improve.3 Touyama et al.,1 in a communication to the editors of the journal, have clarified that all children at GMFCS level V at first ascertainment remained at level V throughout the study period; eight children changed from GMFCS level IV at first ascertainment to level V at last ascertainment, all of whom were alive at the termination of the study; and no children at GMFCS levels I to III at first ascertainment become level V at last ascertainment. My interpretation is that GMFCS level was fairly stable for this study, and thus the impact of late ascertainment on the survival curves was not likely to be dramatic. (Note: A DMCN statistical advisor rightly pointed out that the foregoing issues of possible bias apply when the question at hand is: what impact does GMFCS level now have on long-term survival in the future. If GMFCS level is understood to change over time, a different question is: what impact does level of GMFCS at any time have on survival at that moment? For this question, modeling methods that handle time-varying covariates, e.g. Cox proportional hazards or logistic regression, could be used to estimate the impact.) Brooks et al.4 compared survival in CP at GMFCS level V in California and in Sweden. The 16-year Kaplan-Meier survival was 67% in California and 63% in Sweden, a result the authors suggested was, ‘a significant additional piece of evidence that survival probabilities are remarkably similar for children with severe disability in developed countries.’ Now in Touyama et al. we find 74% 16-year survival (from 2 to 18y) for GMFCS level V. Neither Brooks et al. nor the authors of the original Swedish study by Westbom et al.5 make clear how or