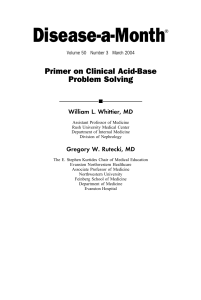
Joint Scientific Statement Harmonizing the Metabolic Syndrome A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity K.G.M.M. Alberti, FRCP; Robert H. Eckel, MD, FAHA; Scott M. Grundy, MD, PhD, FAHA; Paul Z. Zimmet, MD, PhD, FRACP; James I. Cleeman, MD; Karen A. Donato, SM; Jean-Charles Fruchart, PharmD, PhD; W. Philip T. James, MD; Catherine M. Loria, PhD, MS, MA, FAHA; Sidney C. Smith, Jr, MD, FAHA Downloaded from http://ahajournals.org by on November 28, 2019 Abstract—A cluster of risk factors for cardiovascular disease and type 2 diabetes mellitus, which occur together more often than by chance alone, have become known as the metabolic syndrome. The risk factors include raised blood pressure, dyslipidemia (raised triglycerides and lowered high-density lipoprotein cholesterol), raised fasting glucose, and central obesity. Various diagnostic criteria have been proposed by different organizations over the past decade. Most recently, these have come from the International Diabetes Federation and the American Heart Association/National Heart, Lung, and Blood Institute. The main difference concerns the measure for central obesity, with this being an obligatory component in the International Diabetes Federation definition, lower than in the American Heart Association/National Heart, Lung, and Blood Institute criteria, and ethnic specific. The present article represents the outcome of a meeting between several major organizations in an attempt to unify criteria. It was agreed that there should not be an obligatory component, but that waist measurement would continue to be a useful preliminary screening tool. Three abnormal findings out of 5 would qualify a person for the metabolic syndrome. A single set of cut points would be used for all components except waist circumference, for which further work is required. In the interim, national or regional cut points for waist circumference can be used. (Circulation. 2009;120:1640-1645.) Key Words: AHA Scientific Statements 䡲 metabolic syndrome 䡲 risk factors 䡲 diabetes mellitus T elevated triglyceride levels, low high-density lipoprotein cholesterol levels, and obesity (particularly central adiposity). The associations and clustering of these factors have been he metabolic syndrome is a complex of interrelated risk factors for cardiovascular disease (CVD) and diabetes. These factors include dysglycemia, raised blood pressure, The International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity make every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest. This statement was approved by the International Diabetes Federation Task Force on Epidemiology and Prevention on June 19, 2009; the National Heart, Lung, and Blood Institute on May 8, 2009; the American Heart Association Science Advisory and Coordinating Committee on March 23, 2009; the World Heart Federation on July 13, 2009; the International Atherosclerosis Society on June 22, 2009; and the International Association for the Study of Obesity on June 18, 2009. The American Heart Association requests that this document be cited as follows: Alberti KGMM, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart J-C, James WPT, Loria CM, Smith SC Jr. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640 –1645. Copies: This document is available on the World Wide Web site of the American Heart Association (my.americanheart.org). A copy of the document is available at http://www.americanheart.org/presenter.jhtml?identifier⫽3003999 by selecting either the “topic list” link or the “chronological list” link (No. KJ-0730). To purchase additional reprints, call 843-216-2533 or e-mail kelle.ramsay@wolterskluwer.com. Expert peer review of AHA Scientific Statements is conducted at the AHA National Center. For more on AHA statements and guidelines development, visit http://www.americanheart.org/presenter.jhtml?identifier⫽3023366. Permissions: Multiple copies, modification, alteration, enhancement, and/or distribution of this document are not permitted without the express permission of the American Heart Association. Instructions for obtaining permission are located at http://www.americanheart.org/presenter.jhtml?identifier⫽ 4431. A link to the “Permission Request Form” appears on the right side of the page. © 2009 American Heart Association, Inc. Circulation is available at http://circ.ahajournals.org DOI: 10.1161/CIRCULATIONAHA.109.192644 1640 Alberti et al Downloaded from http://ahajournals.org by on November 28, 2019 known for decades. Recent interest has focused on the possible involvement of insulin resistance as a linking factor, although the pathogenesis remains unclear, as does the establishment of diagnostic criteria. With these risk factors, it has been demonstrated clearly that the syndrome is common and that it has a rising prevalence worldwide, which relates largely to increasing obesity and sedentary lifestyles. As a result, the metabolic syndrome is now both a public health and a clinical problem. In the public health arena, more attention must be given to modification of lifestyles of the general public of all nations to reduce obesity and to increase physical activity. At a clinical level, individual patients with the metabolic syndrome need to be identified so that their multiple risk factors, including lifestyle risk factors, can be reduced. Although there is general agreement in the medical community that obesity and its medical complications, including the metabolic syndrome, deserve greater attention, there has been considerable disagreement over the terminology and diagnostic criteria related to the metabolic syndrome. Despite this disagreement, there appears to be a consensus in the medical field that the term metabolic syndrome is acceptable for the condition of the presence of multiple metabolic risk factors for CVD and diabetes. On the other hand, several clinical definitions of the metabolic syndrome have been proposed. This has led to some confusion on the part of clinicians regarding how to identify patients with the syndrome. Some controversy also exists about whether the metabolic syndrome is a true syndrome or a mixture of unrelated phenotypes. A syndrome is simply a clustering of factors that occur together more often than by chance alone and for which the cause is often uncertain. The metabolic syndrome fulfills these criteria. The metabolic syndrome is not an absolute risk indicator, because it does not contain many of the factors that determine absolute risk, for example, age, sex, cigarette smoking, and low-density lipoprotein cholesterol levels. Nonetheless, patients with the metabolic syndrome are at twice the risk of developing CVD over the next 5 to 10 years as individuals without the syndrome. The risk over a lifetime undoubtedly is even higher. Furthermore, the metabolic syndrome confers a 5-fold increase in risk for type 2 diabetes mellitus. The most widely recognized of the metabolic risk factors are atherogenic dyslipidemia, elevated blood pressure, and elevated plasma glucose. In addition, persons with these characteristics commonly manifest a prothrombotic state and a proinflammatory state. Atherogenic dyslipidemia consists of an aggregation of lipoprotein abnormalities that includes elevated serum triglyceride and apolipoprotein B, increased small lowdensity lipoprotein particles, and a reduced level of highdensity lipoprotein cholesterol. Most persons with the metabolic syndrome have abdominal obesity and insulin resistance. Both of the latter conditions appear to contribute to the development of metabolic risk factors, although the mechanisms underlying these contributions are not fully understood. The first formalized definition of the metabolic syndrome was proposed in 1998 by a consultation group on the Harmonizing the Metabolic Syndrome 1641 definition of diabetes for the World Health Organization (WHO).1 This group emphasized insulin resistance as the major underlying risk factor and required evidence of insulin resistance for diagnosis. A diagnosis of the syndrome by WHO criteria could thus be made on the basis of several markers of insulin resistance plus 2 additional risk factors, including obesity, hypertension, high triglyceride level, reduced high-density lipoprotein cholesterol level, or microalbuminuria. Patients with type 2 diabetes mellitus were not excluded from diagnosis. The other major criteria came from the National Cholesterol Education Program Adult Treatment Panel III (ATP III)2 in 2001. ATP III criteria did not require demonstration of insulin resistance per se. Moreover, no single factor was required for diagnosis, but instead, ATP III made the presence of 3 of the following 5 factors the basis for establishing the diagnosis: Abdominal obesity (which is highly correlated with insulin resistance), elevated triglyceride, reduced high-density lipoprotein cholesterol, elevated blood pressure, and elevated fasting glucose (impaired fasting glucose or type 2 diabetes mellitus). In the absence of CVD or diabetes, the metabolic syndrome is a predictor of these conditions. Once CVD or diabetes develops, the metabolic syndrome is often present, and the number of components of the metabolic syndrome contributes to disease progression and risk. In 2005, both the International Diabetes Federation (IDF)3 and the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI)4 attempted to reconcile the different clinical definitions. In spite of this effort, their separate recommendations contained differences related to waist circumference. The IDF dropped the WHO requirement for insulin resistance but made abdominal obesity necessary as 1 of 5 factors required in the diagnosis, with particular emphasis on waist measurement as a simple screening tool; the remainder of the criteria were essentially identical to those provided by ATP III. The AHA/NHLBI slightly modified the ATP III criteria but did not mandate abdominal obesity as a required risk factor. The remaining 4 risk factors were identical in definition to those of the IDF. Moreover, there was no agreement on the definition of abdominal obesity between the IDF and AHA/NHLBI. The IDF recommended that the threshold for waist circumference to define abdominal obesity in people of European origin (Europids) should be ⱖ94 cm for men and ⱖ80 cm for women; the AHA/NHLBI, in contrast, recommended cut points of ⱖ102 and ⱖ88 cm, respectively, for the 2 sexes. The latter values are consistent with the definitions of abdominal obesity found in National Institutes of Health obesity guidelines,5 which equate to a body mass index of approximately 30 kg/m2 in males. The IDF values are closer to a body mass index of 25 kg/m2 in males. The IDF guidelines also stressed the need to adopt different values for waist measurement in different ethnic groups based on the relationship of waist measurement either to the other metabolic syndrome components or to longer-term outcome studies such as those on the risk of type 2 diabetes mellitus and CVD. Recently, IDF and AHA/NHLBI representatives held discussions to attempt to resolve the remaining differences between definitions of metabolic syndrome. Both sides 1642 Circulation October 20, 2009 Table 1. Criteria for Clinical Diagnosis of the Metabolic Syndrome Measure Categorical Cut Points Elevated waist circumference* Population- and country-specific definitions Elevated triglycerides (drug treatment for elevated triglycerides is an alternate indicator†) ⱖ150 mg/dL (1.7 mmol/L) Reduced HDL-C (drug treatment for reduced HDL-C is an alternate indicator†) ⬍40 mg/dL (1.0 mmol/L) in males; ⬍50 mg/dL (1.3 mmol/L) in females Elevated blood pressure (antihypertensive drug treatment in a patient with a history of hypertension is an alternate indicator) Elevated fasting glucose‡ (drug treatment of elevated glucose is an alternate indicator) Systolic ⱖ130 and/or diastolic ⱖ85 mm Hg ⱖ100 mg/dL HDL-C indicates high-density lipoprotein cholesterol. *It is recommended that the IDF cut points be used for non-Europeans and either the IDF or AHA/NHLBI cut points used for people of European origin until more data are available. †The most commonly used drugs for elevated triglycerides and reduced HDL-C are fibrates and nicotinic acid. A patient taking 1 of these drugs can be presumed to have high triglycerides and low HDL-C. High-dose -3 fatty acids presumes high triglycerides. ‡Most patients with type 2 diabetes mellitus will have the metabolic syndrome by the proposed criteria. Downloaded from http://ahajournals.org by on November 28, 2019 agreed that abdominal obesity should not be a prerequisite for diagnosis but that it is 1 of 5 criteria, so that the presence of any 3 of 5 risk factors constitutes a diagnosis of metabolic syndrome. This would result in the common definition shown in Table 1. Defining thresholds for abdominal obesity is complicated, in part because of differences in the relation of abdominal obesity to other metabolic risk factors. In Table 2. addition, predictive values for various levels of abdominal obesity for CVD and diabetes may differ. There is also the problem of generating cut points for continuous variables, although this is true for all components of the syndrome. However, what is particularly needed is evidence based on both cross-sectional and longitudinal data relating waist circumference to risk for both CVD and type 2 diabetes. It is clear that there are and will continue to be differences between sexes and ethnic groups. In addition, there is the practical consideration of what threshold justifies the expenditure of national medical resources for clinical intervention (eg, nutritional and physical activity counseling) in contrast to public health intervention. Of course, this does not mean that there should not be agreed-upon international criteria based on evidence but rather that a particular health system might adopt different cutoff points locally for pragmatic or economic reasons. Long-term prospective studies are required to reach more reliable waist circumference cut points for different ethnic groups, particularly for women. Neither ATP III nor IDF criteria excluded hyperglycemia in the diabetes range as 1 of the 5 criteria for diagnosis of the metabolic syndrome. By these criteria, most patients with type 2 diabetes mellitus have the metabolic syndrome. Moreover, those with type 2 diabetes mellitus are at higher long-term risk for developing CVD. The same is true for patients with type 1 diabetes mellitus. Therefore, any patient with diabetes mellitus who has other metabolic risk factors should be treated with lifestyle intervention, followed by drugs if necessary, to favorably modify other components of the syndrome. Table 2 shows current international recommendations proposed by the IDF for thresholds of abdominal obesity to be used as 1 component of the metabolic syndrome.3 Table 2 also lists waist circumference thresholds currently being recommended in several different populations and ethnic Current Recommended Waist Circumference Thresholds for Abdominal Obesity by Organization Recommended Waist Circumference Threshold for Abdominal Obesity Population Europid Caucasian United States Canada European Asian (including Japanese) Asian Japanese China Middle East, Mediterranean Organization (Reference) Men Women IDF (4) ⱖ94 cm ⱖ80 cm WHO (7) ⱖ94 cm (increased risk) ⱖ80 cm (increased risk) ⱖ102 cm (still higher risk) ⱖ88 cm (still higher risk) AHA/NHLBI (ATP III)* (5) ⱖ102 cm ⱖ88 cm Health Canada (8,9) ⱖ102 cm ⱖ88 cm European Cardiovascular Societies (10) ⱖ102 cm ⱖ88 cm IDF (4) ⱖ90 cm ⱖ80 cm WHO (11) ⱖ90 cm ⱖ80 cm Japanese Obesity Society (12) ⱖ85 cm ⱖ90 cm Cooperative Task Force (13) ⱖ85 cm ⱖ80 cm IDF (4) ⱖ94 cm ⱖ80 cm Sub-Saharan African IDF (4) ⱖ94 cm ⱖ80 cm Ethnic Central and South American IDF (4) ⱖ90 cm ⱖ80 cm *Recent AHA/NHLBI guidelines for metabolic syndrome recognize an increased risk for CVD and diabetes at waist-circumference thresholds of ⱖ94 cm in men and ⱖ80 cm in women and identify these as optional cut points for individuals or populations with increased insulin resistance. Alberti et al Downloaded from http://ahajournals.org by on November 28, 2019 groups. One key question is whether the same criteria should be applied to someone of a particular ethnic group regardless of their country of residence. This would be logical. IDF waist circumference recommendations for the metabolic syndrome are the same for women everywhere owing in part to the paucity of good data, but they are somewhat higher for men of European origin (Europids) than for those of Asian origin. Levels for Asian populations are based on WHO recommendations.6 Fewer data are available for other regions, but Europid male recommendations are applied to men of the Middle East, Eastern Mediterranean region, and Sub-Saharan Africa pending the provision of new data. WHO7 identifies 2 levels of abdominal obesity in Europids depending on risk for metabolic complications. An increased risk occurs at waist circumferences of ⱖ94 cm in men and ⱖ80 cm in women, but risk is substantially higher at ⱖ102 cm in men and ⱖ88 cm in women. Higher thresholds generally are used to define abdominal obesity in the United States,7 Canada,8,9 and Europe.10 These higher thresholds also are used as the waist circumference cut points to identify the metabolic syndrome in the United States. Compared with Europids, an expert consultation for WHO indicated that cut points in the Asian population should be ⱖ90 cm for men and ⱖ80 cm for women.6 Several different levels have been suggested in Japan,11,12 with cutoff points of ⬎85 to 90 cm for men and ⬎80 cm for women suggested by the newest studies in contrast with the original cutoff points.13 In China, cutoff points of ⱖ85 cm in men and ⱖ80 cm in women have been suggested,14 and slightly lower values have been suggested in India. If the higher waist circumference cut points are used to diagnose the metabolic syndrome, fewer individuals should be identified as having the syndrome than if the lower cut point is used. This is true for some countries of the world.15 However, when the NHLBI/AHA definition is used for the United States with the higher or lower cut points, the difference in metabolic syndrome prevalence is relatively small, both because abdominal obesity is highly correlated with the other 4 components of the syndrome16 and because the prevalence of obesity is so high (Figure). We now propose common criteria for the clinical diagnosis of the metabolic syndrome based on the criteria shown in Table 1. This definition recognizes that the risk associated with a particular waist measurement will differ in different populations. Whether it is better at this time to set the level at which risk starts to increase or at which there is already substantially increased risk will be up to local decision-making groups. However, for international comparisons and to facilitate the etiology, it is critical that a commonly agreed-upon set of criteria be used worldwide, with agreed-upon cut points for different ethnic groups and sexes. Obviously, there are many people in the world of mixed ethnicity, and in these cases, pragmatic decisions will have to be made. 50% 45% 40% 35% 30% 25% 20% 15% 10% 5% 0% Harmonizing the Metabolic Syndrome 41.9% 40.1% 35.2% Total 34.8% 35.5% Men Women Total AHA/NHLBI 2005 Men 1643 38.3% Women Revised IDF 2005 Figure. Unadjusted prevalence (95% confidence interval) of the metabolic syndrome among US adults ⱖ20 years of age, National Health and Nutrition Examination Survey 1999 to 2004. Revised IDF 2005 eliminates elevated waist circumference as a requirement for diagnosis of the metabolic syndrome. In both AHA/NHLBI 2005 and revised IDF 2005 definitions, the presence of any 3 of 5 risk factors constitutes a diagnosis of the metabolic syndrome. Analysis performed by Dr E.S. Ford of the Centers for Disease Control and Prevention. It is expected that new expert groups will be formed to assess the evidence with regard to waist circumference thresholds and associated risk in the near future. These include WHO and NHLBI. Both organizational bodies are reconsidering the definition of metabolic syndrome, and we hope that the present scientific statement will provide a useful platform for their discussions. We believe that current recommended waist thresholds should be used pro tempore, although it would be helpful if both the lower and higher criteria for Europids were cited for comparative studies. Some new data are available for different ethnic groups, but it is thought advisable to await the outcomes of the deliberations of WHO and NHLBI, when our group will reconvene to produce a further statement with the intention of having a single agreed-upon set of diagnostic criteria. We would stress that the process is evolutionary. In the interim, further studies exploring the relation of waist circumference thresholds to metabolic risk and cardiovascular outcomes in different populations are encouraged, and we continue to recommend the use of waist measurement as a useful screening tool in many primary care situations. Acknowledgments The authors wish to thank the following people for their valuable contribution to this statement: A. Cameron, J. Chan, S. Del Prato, J.-P. Despres, E. Ford, T. Kadowaki, S.E. Kahn, F. Kaufman, P. Lefèbvre, J.C. Mbanya, F.X. Pi-Sunyer, L. Rydén, S. Sadikot, M.I. Schmidt, J. Shaw, E. Standl, and P.W.F. Wilson. The authors also wish to thank Colette Kon, who has worked closely with the project coordinators and who helped prepare the manuscript for publication. Sources of Funding The development of this statement was sponsored by the IDF, which received unrestricted educational grants from AstraZeneca, Bristol-Myers Squibb, sanofi-aventis, and Metabolic Syndrome Institute (Solvay Pharmaceuticals and Abbott Laboratories). No companies had a role in the development of the statement or the review or approval of the manuscript. 1644 Circulation October 20, 2009 Disclosures Writing Group Disclosures Employment Research Grant Other Research Support Imperial College, St Mary’s Campus (London, UK) None None None None None None None James I. Cleeman NHLBI/NIH None None None None None None None Karen A. Donato NHLBI/NIH None None None None None None None Robert H. Eckel University of Colorado HSC Sanofi-Aventis† None INNOVIA (Sanofi-Aventis sponsored)*; Vindico (Merck sponsored)*; SciMed, LLC*; Cardiometabolic Health Congress* None None Sanofi-Aventis* None Retired None None None None None Solvay†; Kowa†; AstraZeneca† None Scott M. Grundy University of Texas Southwestern Medical Center Donald W. Reynolds grant†; Merck Project†; Abbott† None None None None Merck*; Merck Schering Plough*; AstraZeneca*; Pfizer*; GlaxoSmithKline* None W. Philip T. James London School of Hygiene and Tropical Medicine None None Roche*; Sanofi-Aventis* None None Abbott Laboratories†; Sanofi-Aventis*; GlaxoSmithKline* None Writing Group Member K.G.M.M. Alberti Jean-Charles Fruchart Speakers’ Bureau/Honoraria Expert Witness Ownership Interest Consultant/ Advisory Board Other Downloaded from http://ahajournals.org by on November 28, 2019 Catherine M. Loria NHLBI None None None None None None None Sidney C. Smith, Jr University of North Carolina at Chapel Hill None None None None None None None Paul Z. Zimmet Baker IDI Heart and Diabetes Institute None None None None None Member of Metabolic Syndrome Institute Advisory Group funded by Solvay and Abbott* None This table represents the relationships of writing group members that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire, which all members of the writing group are required to complete and submit. A relationship is considered to be “significant” if (1) the person receives $10 000 or more during any 12-month period, or 5% or more of the person’s gross income; or (2) the person owns 5% or more of the voting stock or share of the entity, or owns $10 000 or more of the fair market value of the entity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition. *Modest. †Significant. References 1. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications, part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539 –553. 2. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. 3. Alberti KG, Zimmet P, Shaw J; IDF Epidemiology Task Force Consensus Group. The metabolic syndrome: a new worldwide definition. Lancet. 2005;366:1059 –1062. 4. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F; American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement [published corrections appear in Circulation. 2005; 112:e297 and Circulation. 2005;112:e298]. Circulation. 2005;112: 2735–2752. 5. National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report [published correction appears in Obes Res. 1998;6:464]. Obes Res. 1998;6(suppl 2):51S–209S. 6. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies [pub- Alberti et al 7. 8. 9. 10. lished correction appears in Lancet. 2004;363:902]. Lancet. 2004;363: 157–163. World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report on a WHO Consultation (WHO Technical Report Series 894). Geneva, Switzerland: World Health Organization; 2000. Health Canada. Canadian Guidelines for Body Weight Classification in Adults. Ottawa, Canada: Health Canada Publications Centre; 2003. Publication ID No. 4645. ISBN 0-662-33431-0. Khan NA, McAlister FA, Rabkin SW, Padwal R, Feldman RD, Campbell NR, Leiter LA, Lewanczuk RZ, Schiffrin EL, Hill MD, Arnold M, Moe G, Campbell TS, Herbert C, Milot A, Stone JA, Burgess E, Hemmelgarn B, Jones C, Larochelle P, Ogilvie RI, Houlden R, Herman RJ, Hamet P, Fodor G, Carruthers G, Culleton B, Dechamplain J, Pylypchuk G, Logan AG, Gledhill N, Petrella R, Tobe S, Touyz RM; Canadian Hypertension Education Program. The 2006 Canadian Hypertension Education Program recommendations for the management of hypertension, part II: therapy. Can J Cardiol. 2006;22:583–593. Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, Dallongeville J, De Backer G, Ebrahim S, Gjelsvik B, Herrmann-Lingen C, Hoes A, Humphries S, Knapton M, Perk J, Priori SG, Pyorala K, Reiner Z, Ruilope L, Sans-Menendez S, Op Reimer WS, Weissberg P, Wood D, Yarnell J, Zamorano JL; ESC Committee for Practice Guidelines. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Atherosclerosis. 2007;194:1– 45. Harmonizing the Metabolic Syndrome 1645 11. Hara K, MatsushitaY, Horikoshi M, Yoshiike N, Yokoyama T, Tanaka H, Kadowaki T. A proposal for the cutoff point of waist circumference for the diagnosis of metabolic syndrome in the Japanese population. Diabetes Care. 2006;29:1123–1124. 12. Oka R, Kobayashi J, Yagi K, Tanii H, Miyamato S, Asano A, Hagishita T, Mori M, Moriuchi T, Kobayashi M, Katsuda S, Kawashiri M, Nohara A, Takeda Y, Mabuchi H, Yamagishi M. Reassessment of the cutoff values of waist circumference and visceral fat for identifying Japanese subjects at risk for the metabolic syndrome. Diabetes Res Clin Pract. 2008;79:474 – 481. 13. Examination Committee of Criteria for “Obesity Disease” in Japan; Japan Society for the Study of Obesity. New criteria for “obesity disease” in Japan. Circ J. 2002;66:987–992. 14. Zhou BF; Cooperative Meta-Analysis Group of the Working Group on Obesity in China. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults: study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15:83–96. 15. Grundy SM. Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol. 2008;28:629 – 636. 16. Assmann G, Guerra R, Fox G, Cullen P, Schulte H, Willett D, Grundy SM. Harmonizing the definition of the metabolic syndrome: comparison of the criteria of the Adult Treatment Panel III and the International Diabetes Federation in United States American and European populations. Am J Cardiol. 2007;99:541–548. Downloaded from http://ahajournals.org by on November 28, 2019