Acute glycemic and pressure responses of continuous and interval aerobic exercise in patients with type 2 diabetes
Anuncio
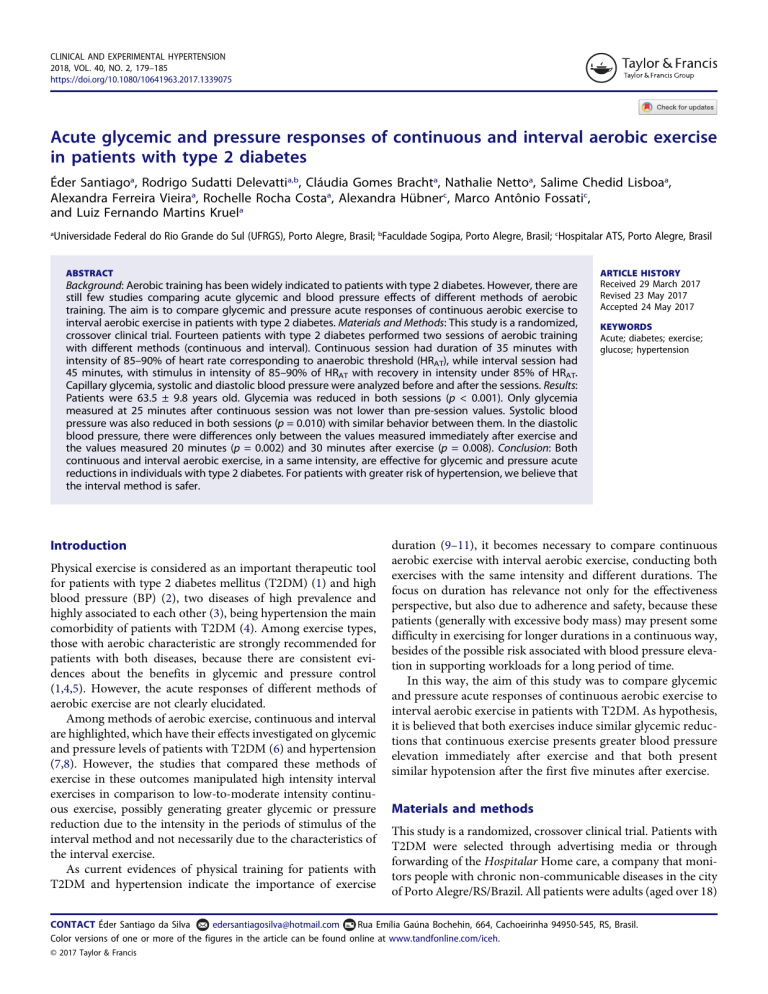
CLINICAL AND EXPERIMENTAL HYPERTENSION 2018, VOL. 40, NO. 2, 179–185 https://doi.org/10.1080/10641963.2017.1339075 Acute glycemic and pressure responses of continuous and interval aerobic exercise in patients with type 2 diabetes Éder Santiagoa, Rodrigo Sudatti Delevattia,b, Cláudia Gomes Brachta, Nathalie Nettoa, Salime Chedid Lisboaa, Alexandra Ferreira Vieiraa, Rochelle Rocha Costaa, Alexandra Hübnerc, Marco Antônio Fossatic, and Luiz Fernando Martins Kruela a Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, Brasil; bFaculdade Sogipa, Porto Alegre, Brasil; cHospitalar ATS, Porto Alegre, Brasil ABSTRACT ARTICLE HISTORY Background: Aerobic training has been widely indicated to patients with type 2 diabetes. However, there are still few studies comparing acute glycemic and blood pressure effects of different methods of aerobic training. The aim is to compare glycemic and pressure acute responses of continuous aerobic exercise to interval aerobic exercise in patients with type 2 diabetes. Materials and Methods: This study is a randomized, crossover clinical trial. Fourteen patients with type 2 diabetes performed two sessions of aerobic training with different methods (continuous and interval). Continuous session had duration of 35 minutes with intensity of 85–90% of heart rate corresponding to anaerobic threshold (HRAT), while interval session had 45 minutes, with stimulus in intensity of 85–90% of HRAT with recovery in intensity under 85% of HRAT. Capillary glycemia, systolic and diastolic blood pressure were analyzed before and after the sessions. Results: Patients were 63.5 ± 9.8 years old. Glycemia was reduced in both sessions (p < 0.001). Only glycemia measured at 25 minutes after continuous session was not lower than pre-session values. Systolic blood pressure was also reduced in both sessions (p = 0.010) with similar behavior between them. In the diastolic blood pressure, there were differences only between the values measured immediately after exercise and the values measured 20 minutes (p = 0.002) and 30 minutes after exercise (p = 0.008). Conclusion: Both continuous and interval aerobic exercise, in a same intensity, are effective for glycemic and pressure acute reductions in individuals with type 2 diabetes. For patients with greater risk of hypertension, we believe that the interval method is safer. Received 29 March 2017 Revised 23 May 2017 Accepted 24 May 2017 Introduction Physical exercise is considered as an important therapeutic tool for patients with type 2 diabetes mellitus (T2DM) (1) and high blood pressure (BP) (2), two diseases of high prevalence and highly associated to each other (3), being hypertension the main comorbidity of patients with T2DM (4). Among exercise types, those with aerobic characteristic are strongly recommended for patients with both diseases, because there are consistent evidences about the benefits in glycemic and pressure control (1,4,5). However, the acute responses of different methods of aerobic exercise are not clearly elucidated. Among methods of aerobic exercise, continuous and interval are highlighted, which have their effects investigated on glycemic and pressure levels of patients with T2DM (6) and hypertension (7,8). However, the studies that compared these methods of exercise in these outcomes manipulated high intensity interval exercises in comparison to low-to-moderate intensity continuous exercise, possibly generating greater glycemic or pressure reduction due to the intensity in the periods of stimulus of the interval method and not necessarily due to the characteristics of the interval exercise. As current evidences of physical training for patients with T2DM and hypertension indicate the importance of exercise KEYWORDS Acute; diabetes; exercise; glucose; hypertension duration (9–11), it becomes necessary to compare continuous aerobic exercise with interval aerobic exercise, conducting both exercises with the same intensity and different durations. The focus on duration has relevance not only for the effectiveness perspective, but also due to adherence and safety, because these patients (generally with excessive body mass) may present some difficulty in exercising for longer durations in a continuous way, besides of the possible risk associated with blood pressure elevation in supporting workloads for a long period of time. In this way, the aim of this study was to compare glycemic and pressure acute responses of continuous aerobic exercise to interval aerobic exercise in patients with T2DM. As hypothesis, it is believed that both exercises induce similar glycemic reductions that continuous exercise presents greater blood pressure elevation immediately after exercise and that both present similar hypotension after the first five minutes after exercise. Materials and methods This study is a randomized, crossover clinical trial. Patients with T2DM were selected through advertising media or through forwarding of the Hospitalar Home care, a company that monitors people with chronic non-communicable diseases in the city of Porto Alegre/RS/Brazil. All patients were adults (aged over 18) CONTACT Éder Santiago da Silva edersantiagosilva@hotmail.com Rua Emília Gaúna Bochehin, 664, Cachoeirinha 94950-545, RS, Brasil. Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/iceh. © 2017 Taylor & Francis 180 É. SANTIAGO ET AL. and were in medical treatment for T2DM. As exclusion criteria, we had severe non-proliferative diabetic retinopathy, uncompensated heart failure, lower-limbs amputation, body mass index (BMI) ≥ 45 kg/m2, kidney insufficiency or any problem that could impair the accomplishment of physical exercises. All patients filled an Informed Consent Form in the terms approved by the Ethics Committee in Research of the Federal University of Rio Grande do Sul (nº 1.571.144). This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors. Experimental procedures After recruitment and selection of the sample, the subjects were informed of all the procedures involved in the study, presented an exercise electrocardiography of the previous six months and were inserted in a program called pre-training, which had the aim to minimally prepare the individuals for the accomplishment of the main exercise sessions with greater safety and in order to know the pressure and glycemic acute effects in slightly trained patients, which is something generally studied in sedentary people. At the end of this period, the patients performed an anthropometric evaluation, only for the characterization of the sample, and a progressive maximal test, in order to determine exercise intensity. After the determination of the exercise intensity, the order of the experimental sessions (continuous and interval) was randomically determined through the software www.randomi zation.com. The patients performed the sessions (one for each regimen—continuous and interval) in the determined order with a minimum of 48 hours of interval between them. Before sessions, the patients remained seated at rest for five minutes, then their glycemia, SBP and DBP were assessed, and after this, they performed the exercise. Finally, the same outcomes were analyzed immediately, five, 10, 15, 20, 25 and 30 minutes after the end of the sessions. Progressive maximal test After the pre-training period, the participants underwent a maximal exercise test for the determination of the heart rate deflection point (HRDP), which is in concordance with the anaerobic threshold in patients with T2DM (14). For the accomplishment of this test, in which protocol was already used in a clinical trial with the same population (15), a treadmill was used with resolution of speed and slope of 0.1 km/h−1 and 1%, respectively. Initial speed was 3 km/h in the first three minutes, and it was incremented by 1 km/h at every two minutes until exhaustion. Heart rate was monitored using a heart rate monitor, and it was registered at each interval of 10 seconds. Food control In the preceding 24 hours of the experimental sessions, the patients registered all the ingested food in a food record of 24 hours. Total energy intake, of macronutrients, of water and sodium was evaluated by a nutritionist and demonstrated using a percentage distribution. Capillary glycemia Capillary glycemia was assessed using a clinical glucometer (Accu-Check Performa, Roche, São Paulo, Brazil), which assessed glycemic levels in approximately five seconds, and disposable lancets (Accu-Check Safe-T-Pro Uno, Roche, São Paulo, Brazil). Systolic and diastolic blood pressure SBP and DBP were assessed using an ambulatory blood pressure monitoring (MAPA) of the brand MEDITECH, model ABPM-04, Budapest, Hungary. Anthropometric measurements For the evaluation of anthropometric variables, a day was scheduled in which the participants attended wearing costumes with two pieces. Initially, the height was measured with metal stadiometer of the brand Filizola, with resolution of 1 mm, and body mass was assessed with analogic scale of the brand Filizola, with resolution of 0,1 kg. With these values body mass index (BMI) was calculated by using the formula body mass(kg)/height2(m). After this, waist circumference was measured with flexible and inelastic tape of the brand Cescorf, with resolution of 1 mm, in the midpoint between the iliac crest and the last rib. With this value, waist/height ratio was calculated. Finally, the measurement of seven skinfolds was taken, with adipometer of the brand Cescorf, with resolution of 1 mm. The seven measured skinfolds were triciptal, subscapular, suprailiac, abdominal, mid-axillary, thigh and leg. With these values, body density was estimated using the appropriate equations for men and women (12). Body fat percentage of both sexes was also estimated (13). The resulting value of the sum of seven skinfolds was considered as the sum of skinfolds. Pre-training period Pre-training period consisted of eight weeks. In the first four weeks, the sessions were of continuous exercise with Borg’s rating of perceived exertion (16) (RPE) between 11 and 13 with progressive volume, starting with 20 minutes and increasing 5 minutes per week. In the last four weeks, the sessions were interval, with 400 m with RPE between 13 and 15 interpersed with 400 m with RPE between 11 and 13. Interventions (continuous and interval sessions) Continuous session had a warm-up period consisted of five minutes of light walk, main part of 35 minutes between 85 and 90% of anaerobic threshold (AT) and stretching for the main muscle groups at the end. Interval session differed only in the main part, which had duration of 45 minutes, with stimuli in the same intensity and recovering at intensity lower than 85% of AT. The structure of the sessions can be visualized on Table 1. CLINICAL AND EXPERIMENTAL HYPERTENSION Table 1. Description of the sessions. Model Duration (min) Description 35 45 85 to 90% of AT 9 x 5 min (4 min 85–90% of AT + 1 min < 85% AT) Continuous Interval AT: Anaerobic Threshold. Statistical analysis Sample characterization data are expressed by mean and standard deviation in continuous variables and by n and percentage in categorical variables. The outcomes (glycemia, SBP and DBP) were presented as mean and standard error. For comparison of the outcomes in different moments and sessions, Generalized Estimating Equations (GEE) with post hoc of Bonferroni was used, adopting a significance level of 0,05. The analyzes were conducted in the statistical program SPSS (Armonk, NY, USA), version 20.0. Results Twenty-four patients initiated the study, and 10 did not conclude the pre-training period, claiming some health problem that impaired the transportation to the training sessions. Of the 14 volunteers able to accomplish the experimental sessions, 10 were randomically distributed to perform the continuous session first and in other day the interval session, and the opposite happened to the other volunteers. Sample characterization, as well as medicines of regular use for the control of diabetes and hypertension, is presented on Table 2. The food records analyses did not demonstrate any difference between the percentage distributions of macronutrients ingested in the 24 hours preceding the continuous and interval exercise sessions (carbohydrates: p = 0.397; proteins: p = 0.993; lipids: 181 Table 2. Sample characterization, consisting of mean ± standard deviation of age, height, body mass, body mass index (BMI), waist circumference, waist/ height ratio (WHtR), fat percentage (%F), fat mass and sum of 7 skinfolds (Σ7 skinfolds). The use of medication is expressed by absolute frequency (“n”). Patients with type 2 diabetes Age (years) 63.58 ± 9.8 Height (m) 1.63 ± 0.1 Body mass (Kg) 81.50 ± 13.8 BMI (Kg) 30.27 ± 4.4 Waist circumference (cm) 102.17 ± 7.4 WHtR 0.62 ± 0.0 %F 23.71 ± 6.2 Fat mass (kg) 19.45 ± 6.5 ∑7 skinfolds(mm) 206.11 ± 58.8 Medication (n) Metformin 10 Sulfonylureas 4 Dipeptidyl peptidase-4 inhibitor 2 Insulin 3 Diuretics 6 ACE inhibitors 10 Beta-blockers 2 ACE: Angiotensin-converting enzyme p = 0.161), as well as in relation to total energetic value (p = 0.061). Glycemia Figure 1 presents glycemic behavior resulting from experimental sessions. In a general way, both exercise prescription models resulted in significant glycemic reductions to the patients (p < 0.001); however, session x time interaction (p = 0.026) demonstrated a distinct behavior over time, given that in the analysis of the continuous session, the only moment that glycemia had the same value of the pre-session occurred at 25 minutes post-session, which is not observed in the interval session, when all post-exercise measurements was shown different and lower than pre-exercise values. In the continuous session, glycemia varied from 168.00 (± 14.69) mg.dl−1 before exercise to 122.79 Figure 1. Glycemic behavior resulting from continuous and interval exercise sessions, presenting mean and standard error for the values of pre-exercise, immediately post-exercise, 5, 10, 15, 20, 25 and 30 minutes after the end of exercise sessions. * Different from Pre-exercise for both models, p < 0,050; † Different from 5 min after the end of exercise in interval session, p < 0,050. 182 É. SANTIAGO ET AL. (± 10.00) mg.dl−1 immediately after exercise (−27.4%), and, in a similar manner, in the interval session, the mean variation was from 179.79 (± 14.12) mg.dl−1 before sessions to 131.43 (± 10.96) mg.dl−1 in the first data collection after the end of session (−26.9%). After the glycemic reductions observed immediately post-exercise, the values remained stable in the following 30 minutes after the end of sessions. Systolic blood pressure The results regarding to SBP are presented on Figure 2. Just as in glycemia, SBP behavior did not show significant difference between sessions (p = 0.064), and however, there was a difference in time effect, which showed significant statistical difference (p = 0.010) in this outcome resulting from both protocols. Time x session interaction did not show significance (p = 0.363). In the continuous session, mean initial SBP values of the participants were 135.29 ± 4.95 mmHg, which showed a nonsignificant increase to 148.46 ± 5.93 mmHg immediately post-exercise. In the following 30 minutes, SBP behavior remained stable, varying from 124.64 ± 3.14 mmHg to 130.92 ± 2.29 mmHg. In the interval session, mean initial SBP value of the participants was 133.71 ± mmHg, with a modest (nonsignificant) alteration to 136.43 ± 3.74 mmHg immediately after exercise session, remaining stable with values that varied in average from 121.14 ± 2.58 mmHg to 123.00 ± 4.98 mmHg. In both models of session, in the last collection—conducted with 30 minutes of rest after the end of exercise—the lowest SBP was measured, which reached 124.64 ± 3.14 mmHg in average in the continuous exercise session and 121.14 ± 2.58 mmHg in average in the interval exercise session, representing reductions of 7.86% and 9.40%, respectively, in relation to the mean values measured before the exercise sessions. Diastolic blood pressure The results referring to DBP are presented on Figure 3. The execution of the different models of aerobic session did not result in significant difference in the DBP behavior (p = 0.357). However, a significant reduction in this outcome over time was observed (p = 0.034). The significant session x time interaction (p < 0.001) indicated that only in the continuous session a significant alteration of the DBP was shown, and this difference only occurred in the comparisons between immediately after exercise and 20 (p = 0.002) and 30 minutes (p = 0.008) after exercise. All the other moments of the continuous session did not show significant difference between them, as well was observed in the interval session. Individual responsiveness Although significant differences were not observed in the glycemic and pressure behavior of the participants between the exercise sessions performed, in an analysis of individual responsiveness, it becomes evident that some of the participants showed glycemic and pressure reductions more expressively in the continuous session and others in the interval one. Continuous session induced better responsiveness in glycemia of half of the participants, and the other half responded better in the interval session. SBP presented better responses in four participants for the continuous session and in ten for the interval session. On the other hand, DBP showed better responses in six participants for the continuous session and in eight for the interval session. Graphically, the individual responsiveness of the glycemia, SBP and DBP of the participants resulting from the exercise sessions proposed can be visualized on Figure 4, in which preexercise and immediately post-exercise data are included. Figure 2. Systolic blood pressure (SBP) behavior resulting from continuous and interval exercise sessions, presenting mean and standard error for the values of pre-exercise, immediately post-exercise, 5, 10, 15, 20, 25 and 30 minutes after the end of exercise sessions. * Different from pre- and post-exercise for both models, p < 0,050. CLINICAL AND EXPERIMENTAL HYPERTENSION 183 Figure 3. Diastolic blood pressure (DBP) behavior resulting from continuous and interval exercise sessions, presenting mean and standard error for the values of preexercise, immediately post-exercise, 5, 10, 15, 20, 25 and 30 minutes after the end of exercise sessions. * Different from post-exercise in interval session, p < 0,050. Figure 4. Individual responsiveness of the glycemia, systolic (SBP) and diastolic blood pressure (DBP) of the participants resulting from exercise sessions in the continuous and interval exercise sessions. Absolute values in the pre-session and immediately post-session moments. Different lines represent different participants of the sample. Discussion In relation to glycemic behavior, our findings confirm our hypothesis, because continuous and interval aerobic exercise sessions induced similar glycemic reductions. This reduction was demonstrated immediately after exercise, and it was maintained during the following 30 minutes in which glycemia was evaluated. SBP behavior was also similar between sessions, in which a reduction occurred 5 minutes post- 184 É. SANTIAGO ET AL. exercise, remaining stable until 25 minutes after exercise, and a further reduction was demonstrated 30 minutes after the end of exercise. Regarding DBP, while the patients showed stability in all measurements made in the interval session, the values registered 20 and 30 minutes after continuous session were smaller than those registered immediately after exercise. Our findings regarding to SBP and DBP only partially support our hypothesis, because despite the nonsignificance, the continuous session seems to result in greater values immediately after the session, although only SBP presented the expected hypotensive effect. We believe that the similarity found between the proposed sessions is due to the identical intensity and similar volume of exercise performed, because whereas continuous session had 35 minutes of stimulus between 85 and 90% of AT, interval session had 36 minutes of stimulus at the same intensity (9 × 5 min – 4 min stimulus: 1 min recovery). Unlike our results, Karstoft et al. (2014) (6) found greater glycemic reduction in the interval session compared to continuous session in patients with T2DM. The characteristics of this study (duration, energy expenditure and similar mean intensity between interval and continuous exercise groups) demonstrated that just the fact that interval group performed excursions in higher intensities provided glycemic reductions in greater magnitude. Thus, intensity is perceived as a characteristic that is more associated to glycemic decreases than just the exercise training method, which was something already expected, because while intensity is a variable with physiological character, the fact that the exercise is performed in a continuous or interval manner has only methodological character, without any relation to metabolic alteration. In the same context, Terada et al. (2013) (17) compared the glycemic response to a continuous exercise session in an intensity lower or equal to 40% of VO2res with an interval exercise session with periods composed of one minute of stimulus at 100% do VO2res and three minutes of recovery in an intensity lower or equal to 20% VO2res and found a bigger reduction after the interval session. In the protocols used by Karstoft et al. (2014) (6) and Terada et al. (2013) (17), the same exercise duration between the continuous and interval methods and the structure of the periods of stimulus (time and magnitude of the stimulus: time and magnitude of the recovery) favored an equalization between the protocols compared. However, when the organism is working in high physiologic intensities during the stimuli periods, the decrease of the physiologic variables in the recovery can be very slow, especially in sedentary individuals, which can explain the superiority of the interval strategy, once it permits the accomplishment of stimuli in high intensities. Along with intensity, the duration of the session is another fundamental variable in the structure of the aerobic training. In chronic studies, this variable has been showing itself very important to glycemic control (9,10) in patients with T2DM, whereas in studies carried out with acute protocols, it has not been focused as primary outcome of the investigations. While some studies (6,17) proposed interval sessions with higher intensities than the continuous sessions, our proposal was to make the interval session longer than the continuous one, by adding 10 minutes in the total duration of the session, which did not result in a greater glycemic reduction. Based on our findings, caution should be exercised when associating glycemic reduction with the aerobic exercise method, because when a method does not represent a substantial energetic contribution in relation to the other method, both seem to promote similar responses, even that the duration of the session is augmented in the interval protocol. The elevation of the SBP immediately after exercise was not significant. However, a clinical overview becomes necessary, because even without statistical difference between the sessions, the continuous model implied in an elevation of the SBP, whereas the interval model showed stabilization; thus, in the pressure point of view, the interval session proved to be safer. Regarding to efficacy, we did not find expressive difference between the sessions, both caused hypotension after exercise from five minutes post-exercise, with a more pronounced effect in the last measurement (30 minutes after exercise). The mechanisms by which aerobic exercise provokes post-exercise hypotension have been well documented, highlighting the decrease of the sympathetic activity, the increase of the nitric oxide vasodilator action and a greater action of the baroreflex system (7). Our findings corroborate with other studies (18–20) that did not find difference in the blood pressure reduction between continuous and interval exercise sessions, even that in these studies the interval sessions had greater intensities than those used in the continuous sessions. By the fact that these studies, as well as our study, were conducted with sedentary or minimally trained, hypertensive individuals and that the greater intensities did not add any effect in the reduction of the blood pressure, we believe that a safe and effective exercise prescription for this public can have moderate intensity (~60%HRres – 85–90%AT), interval method and duration of approximately 40 minutes. Due to the more stable behavior of the BP immediately after exercise in the interval exercise session, we believe that the use of this method might promote a greater safety in the progression of the intensity throughout the training periodizations for these patients. This is because in a trained physiological state, these patients will need a higher training intensity to keep having cardiovascular benefits, which they can achieve in a safer way by not sustaining the intensity in the continuous manner. Although we did not expect an elevation of the DBP in dynamic exercises and this was not demonstrated in the present study, Figure 4 presents a behavior of increase, which is still not expressive. By analyzing the measurements performed from five minutes post-exercise sessions, we can perceive stability in this outcome, because there were minor differences in the continuous sessions (20 and 30 minutes post-exercise) that did not stabilize even in two consecutive moments. This little alteration of the DBP is primarily explained by the amplitude of improvement that it offers, which is lower than SBP. This amplitude can be very attenuated in this study, because although the individuals were hypertensive, they were with a well controlled DBP (presession DBP: 74.25 ± 2.25 mmHg), with values considered normal (60 to 84 mmHg) according to the Brazilian Society of Cardiology (21). The greater stability of the DBP can be explained because while the bigger cardiac output during exercise is a stimulus of increased DBP, the vasodilation derived from exercise reduces peripheral vascular resistance, minimizing or even nullifying the increase in DBP (22). CLINICAL AND EXPERIMENTAL HYPERTENSION Our findings corroborate with those of Tomasi et al. (2008) (23), which conducted a study with 10 men who performed resistance (3 series of 12 repetitions with 60% of 1RM) and aerobic (40 minutes at 60% of HRmax) exercises in distinct days and found a reduction in DBP only 20 minutes after the exercise sessions for normotensive individuals. On the other hand, Reis et al. (2012) (24) evaluated 75 individuals after 60 minutes of aerobic continuous exercise between 50 and 70% of HRmax and did not find any difference in DBP in the individuals with presession DBP lower than 85 mmHg, similar to the present study (74,24 ± 2,26 mmHg). In this way, we considered both sessions positive for DBP, because in patients who have this outcome well controlled, the non-elevation of this outcome can be already considered a positive result. This study had as main limitation the reduced post-session time in which the outcomes evaluated were measured, because we believe that a follow-up longer than 30 minutes would be interesting to enlarge the knowledge about the glycemic and pressure impact of the proposed sessions. However, to our knowledge, the investigation of the acute glycemic and pressure effects of aerobic exercise in patients with T2DM has not been investigated in a same study. As strong points of the present study, we highlight the methods used, with the order of the sessions conducted randomically, having food record and a post-session curve with seven measurements. Conclusion We conclude that both continuous and interval aerobic exercise, in a same intensity, are effective for glycemic and pressure acute reductions in individuals with T2DM. For patients who do not present high blood pressure or maintain it well controlled, the choice of the exercise method can be due to time saving (continuous session) or to less monotony (interval session), thus favoring adherence to exercise. For patients with greater risk of hypertension, we believe that the interval method is safer, with similar efficacy to the continuous method. References 1. American diabetes association. Standards of medical care in diabetes. Diabetes Care 2016;39(Suppl. 1):S14–S80. 2. Pescatello L, MacDonald HV, Ash GI, et al. Assessing the existing professional exercise recommendations for hypertension: A review and recommendations for future research priorities. Mayo Clinic Proceedings Elsevier 2015;90:801–12. 3. Chokshi NP, Grossman E, Messerli FH. Blood pressure and diabetes: Vicious twins. Heart 2013;99:577–85. 4. Qiu S, Cai X, Schumann U, et al. Impact of walking on glycemic control and other cardiovascular risk factors in type 2 diabetes: A meta-analysis. Plos ONE 2014;9:e109767. 5. Yang Z, Scott CA, Mao C, et al. Resistance exercise versus aerobic exercise for type 2 diabetes: A systematic review and meta-analysis. Sports Med 2013;44:487–89. 185 6. Karstoft K, Christensen CS, Pedersen BK, Solomon TPJ. The acute effects of interval- Vs continuous-walking exercise on glycemic control in subjects with type 2 diabetes: A crossover, controlled study. J Clin Endocrinol Metab 2014;99:3334–42. 7. Guimarães GV, Ciolac EC, Carvalho VO, et al. Effects of continuous vs. interval exercise training on blood pressure and arterial stiffness in treated hypertension. Hypertens Res 2010;33:627–32. 8. Ciolac EG, Guimarães GV, D’Ávila VM, et al. Acute effects of continuous and interval aerobic exercise on 24-h ambulatory blood pressure in long-term treated hypertensive patients. Int J Cardiol 2009;133:381–87. 9. Umpierre D, Ribeiro PAB, Kraemer CK, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes. Jama 2011;305:1790e–1799e. 10. Li J, Zhang W, Guo Q, et al. Duration of exercise as key determinant of improvement in insulin sensivity in type 2 diabetes patients. Tokohu J Exp Med 2012;227:189–296. 11. Figueira FR, Umpierre D, Cureau FV, et al. Association between physical activity advice only or structured exercise training with blood pressure levels in patients with type 2 diabetes: A systematic review and meta-analysis. Sports Med 2014;44:1557–72. 12. Petroski EL. Desenvolvimento e validação de equações generalizadas para a estimativa da densidade corporal em adultos. Santa Maria, Tese de Doutorado, Universidade Federal de Santa Maria, 1995. 13. Siri WE. Body composition from fluid spaces and density: Analysis of methods. Nutrition 1993;9:480–91. 14. Delevatti RS, Kanitz AC, Alberton CL, et al. Heart rate deflection point as an alternative method to identify the anaerobic threshold in patients with type 2 diabetes. Apunt Med Esport 2015;50:123e–128. 15. Delevatti RS, Kanitz AC, Alberton CL, et al. Glucose control can be similarly improved after aquatic or dry-land aerobic training in patients with type 2 diabetes: A randomized clinical Trial. J Sci Med Sport 2016;19:688–93. 16. Borg G. Borg´s perceived exertion and pain scales. Champaign, IL, Human Kinetics, 1998; 1–103. 17. Terada T, Friesen A, Chahal BS, et al. Exploring the variability in acute glycemic responses to exercise in type 2 diabetes. J Diabetes Res 2013;2013:1–6. 18. Guimarães GV, Ciolac EG, Carvalho VO. Effects of continuous vs. interval exercise training on blood pressure and arterial stiffness in treated hypertension. Hypertens Res 2010;33:627–32. 19. Emmanuel GC, Guilherme G, Veridiana D. et al. Acute effects of continuous and interval aerobic exercise on 24-h ambulatory blood pressure in long-term treated hypertensive patients. Int J Cardiol 2009;133:381–87. 20. Cunha GA, Rios ACS, Moreno JR, et al. Hipotensão pós-exercício em hipertensos submetidos ao exercício aeróbio de intensidades variadas e exercício de intensidade constante. Revista Brasileira De Medicina Do Esporte 2006;12:313–17. 21. Sociedade Brasileira de Cardiologia. VI Diretrizes brasileiras de hipertensão. Arq Bras Cardiol 2010;95(1 supl 1):1–51. 22. Krieger EM, Brum PC, Negrão CE. Role of arterial baroreceptor function on cardiovascular adjustments to acute and chronic dynamic exercise. Biol Res 1998;31:273–79. 23. Tomasi T, Simão R, Polito MD. Comparação do comportamento arterial após sessão de exercício aeróbico e de força em indivíduos normotensos. Revista Da Educação Fìsica/UEM 2008;19:361–67. 24. Reis SM, Ferreira VRF, Prado FL, Lopes AMC. Análise da resposta pressórica Mediante exercício físico regular em indivíduos normotensos, hipertensos e hipertensos-diabéticos. Rev Bras Cardiol 2012;25:290–98. Copyright of Clinical & Experimental Hypertension is the property of Taylor & Francis Ltd and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.