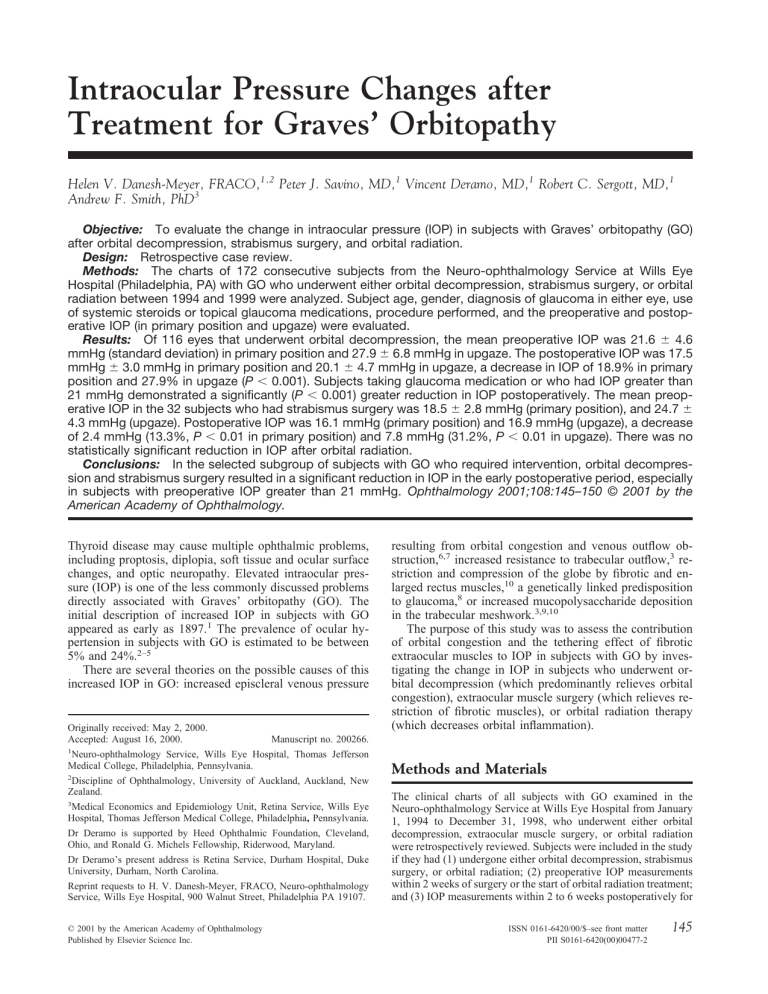
Intraocular Pressure Changes after Treatment for Graves’ Orbitopathy Helen V. Danesh-Meyer, FRACO,1,2 Peter J. Savino, MD,1 Vincent Deramo, MD,1 Robert C. Sergott, MD,1 Andrew F. Smith, PhD3 Objective: To evaluate the change in intraocular pressure (IOP) in subjects with Graves’ orbitopathy (GO) after orbital decompression, strabismus surgery, and orbital radiation. Design: Retrospective case review. Methods: The charts of 172 consecutive subjects from the Neuro-ophthalmology Service at Wills Eye Hospital (Philadelphia, PA) with GO who underwent either orbital decompression, strabismus surgery, or orbital radiation between 1994 and 1999 were analyzed. Subject age, gender, diagnosis of glaucoma in either eye, use of systemic steroids or topical glaucoma medications, procedure performed, and the preoperative and postoperative IOP (in primary position and upgaze) were evaluated. Results: Of 116 eyes that underwent orbital decompression, the mean preoperative IOP was 21.6 ⫾ 4.6 mmHg (standard deviation) in primary position and 27.9 ⫾ 6.8 mmHg in upgaze. The postoperative IOP was 17.5 mmHg ⫾ 3.0 mmHg in primary position and 20.1 ⫾ 4.7 mmHg in upgaze, a decrease in IOP of 18.9% in primary position and 27.9% in upgaze (P ⬍ 0.001). Subjects taking glaucoma medication or who had IOP greater than 21 mmHg demonstrated a significantly (P ⬍ 0.001) greater reduction in IOP postoperatively. The mean preoperative IOP in the 32 subjects who had strabismus surgery was 18.5 ⫾ 2.8 mmHg (primary position), and 24.7 ⫾ 4.3 mmHg (upgaze). Postoperative IOP was 16.1 mmHg (primary position) and 16.9 mmHg (upgaze), a decrease of 2.4 mmHg (13.3%, P ⬍ 0.01 in primary position) and 7.8 mmHg (31.2%, P ⬍ 0.01 in upgaze). There was no statistically significant reduction in IOP after orbital radiation. Conclusions: In the selected subgroup of subjects with GO who required intervention, orbital decompression and strabismus surgery resulted in a significant reduction in IOP in the early postoperative period, especially in subjects with preoperative IOP greater than 21 mmHg. Ophthalmology 2001;108:145–150 © 2001 by the American Academy of Ophthalmology. Thyroid disease may cause multiple ophthalmic problems, including proptosis, diplopia, soft tissue and ocular surface changes, and optic neuropathy. Elevated intraocular pressure (IOP) is one of the less commonly discussed problems directly associated with Graves’ orbitopathy (GO). The initial description of increased IOP in subjects with GO appeared as early as 1897.1 The prevalence of ocular hypertension in subjects with GO is estimated to be between 5% and 24%.2–5 There are several theories on the possible causes of this increased IOP in GO: increased episcleral venous pressure Originally received: May 2, 2000. Accepted: August 16, 2000. Manuscript no. 200266. 1 Neuro-ophthalmology Service, Wills Eye Hospital, Thomas Jefferson Medical College, Philadelphia, Pennsylvania. 2 Discipline of Ophthalmology, University of Auckland, Auckland, New Zealand. 3 Medical Economics and Epidemiology Unit, Retina Service, Wills Eye Hospital, Thomas Jefferson Medical College, Philadelphia, Pennsylvania. Dr Deramo is supported by Heed Ophthalmic Foundation, Cleveland, Ohio, and Ronald G. Michels Fellowship, Riderwood, Maryland. Dr Deramo’s present address is Retina Service, Durham Hospital, Duke University, Durham, North Carolina. Reprint requests to H. V. Danesh-Meyer, FRACO, Neuro-ophthalmology Service, Wills Eye Hospital, 900 Walnut Street, Philadelphia PA 19107. © 2001 by the American Academy of Ophthalmology Published by Elsevier Science Inc. resulting from orbital congestion and venous outflow obstruction,6,7 increased resistance to trabecular outflow,3 restriction and compression of the globe by fibrotic and enlarged rectus muscles,10 a genetically linked predisposition to glaucoma,8 or increased mucopolysaccharide deposition in the trabecular meshwork.3,9,10 The purpose of this study was to assess the contribution of orbital congestion and the tethering effect of fibrotic extraocular muscles to IOP in subjects with GO by investigating the change in IOP in subjects who underwent orbital decompression (which predominantly relieves orbital congestion), extraocular muscle surgery (which relieves restriction of fibrotic muscles), or orbital radiation therapy (which decreases orbital inflammation). Methods and Materials The clinical charts of all subjects with GO examined in the Neuro-ophthalmology Service at Wills Eye Hospital from January 1, 1994 to December 31, 1998, who underwent either orbital decompression, extraocular muscle surgery, or orbital radiation were retrospectively reviewed. Subjects were included in the study if they had (1) undergone either orbital decompression, strabismus surgery, or orbital radiation; (2) preoperative IOP measurements within 2 weeks of surgery or the start of orbital radiation treatment; and (3) IOP measurements within 2 to 6 weeks postoperatively for ISSN 0161-6420/00/$–see front matter PII S0161-6420(00)00477-2 145 Ophthalmology Volume 108, Number 1, January 2001 those who had orbital decompression or strabismus surgery or between 6 and 12 weeks from the end of radiation treatment. Subjects were excluded if there were changes to their medications that could influence IOP (glaucoma medication and oral steroids) or if there were incomplete preoperative or postoperative data in the medical records. Information that was collected from the medical record included subject age, gender, diagnosis of glaucoma in either eye, use of systemic steroids or topical glaucoma medications, procedure performed, and the preoperative and postoperative IOP. In all subjects, the IOP was recorded in the primary position and in upgaze. All subjects who underwent orbital decompression had two wall (medial and inferior) orbital decompression with an endonasal approach to the medial wall. Extraocular muscle surgery consisted of unilateral or bilateral inferior rectus muscle recession at times combined with medial rectus muscle recessions. Strabismus surgery used adjustable suture technique in all inferior rectus muscle surgery. Subjects who had orbital radiation had received a dose of 2000 cGy delivered in 10 200-cGy daily fractions. Statistical Methods Data were collected and entered into a computerized statistical software package (SPSS Version 6.1) (SPSS Inc, Chicago, IL) in a standard fashion. Analysis of the data consisted of deriving the descriptive statistics, calculating the means, and tests for statistical significance, including two-tailed Student’s t tests and the analysis of variance, which measure differences in IOP readings between the three intervention groups and between preoperative and postoperative IOP levels. Throughout, P value for significance was set at 0.05. Results The charts of 172 subjects with GO treated with orbital decompression, strabismus surgery, or orbital radiation were reviewed; 132 subjects met the inclusion criteria, leaving 204 eyes for analysis. One hundred sixteen eyes (80 subjects) underwent orbital decompression, 32 eyes (24 subjects) underwent strabismus surgery, and 56 eyes (28 subjects) underwent orbital radiation. Forty subjects were excluded. Thirty subjects had inadequate follow-up information, and 10 were excluded because oral steroids were begun between the preoperative and postoperative visits. The average age for the entire group was 50.5 years (range, 27–76 years). Most subjects (60%) were women. Fifty-six subjects had a diagnosis of glaucoma and were taking topical glaucoma medications at the time of referral to the Neuroophthalmology Service. Table 1 summarizes the demographic data for each of the three groups. Orbital Decompression For all subjects who underwent orbital decompression, the mean preoperative IOP was 21.6 ⫾ 4.6 mmHg (standard deviation) in primary position and 27.9 ⫾ 6.8 mmHg in upgaze (Table 2). The mean postoperative IOP was 17.5 mmHg ⫾ 3.0 mmHg in primary position and 20.1 ⫾ 4.7 mmHg in upgaze. This was a mean decrease in IOP postoperatively of 18.9% in primary position and 27.9% in upgaze. (P ⬍ 0.001) The change in IOP after orbital decompression surgery was further analyzed according to indication for surgery (Table 3) and whether subjects were taking glaucoma medications (Table 4). The indication for decompressive surgery was optic neuropathy in 80 eyes and proptosis in 36 eyes. Subjects with optic neuropathy 146 Table 1. Demographic Data (Number of Eyes ⫽ 204) Characteristic Decompression Strabismus Radiation n Age, mean (SD) Female, n (%) Indications for surgery, n (%) Diplopia Proptosis Optic neuropathy Inflammatory disease On glaucoma medications, n (%) 116 49.0 (10.6) 84 (72) NA 36 (31) 80 (69) NA 35 (30) 32 56 51.3 (9.4) 53.5 (11.2) 22 (69) 41 (74) 100 NA NA NA 13 (41) NA NA 38 (67) 18 (32.2) 8 (14) SD ⫽ standard deviation. showed a 21.6% (5.0 mmHg, P ⬍ 0.01) decrease in their IOP postoperatively in primary position and 30.7% (9.2 mmHg, P ⬍ 0.01) in upgaze. The decrease in IOP in the proptosis group was 9.5% (1.7 mmHg, P ⬍ 0.01). Thirty-five eyes were receiving glaucoma medication; 19 were taking one topical antiglaucoma agent, and 16 were taking two agents. Subjects who were taking glaucoma medication had a significant decrease of 27.4% (7.1 mmHg, P ⬍ 0.001) in IOP postoperatively in primary position and 30% (9.1 mmHg, P ⬍ 0.001) in upgaze. Those who underwent orbital decompression who were not on glaucoma medications had a smaller decrease in IOP postoperatively of 13.9% (2.8 mmHg, P ⬍ 0.001) in primary position and 27.2% (7.3 mmHg, P ⬍ 0.001) in upgaze. Subjects (n ⫽ 51) who had preoperative IOP values of less than 21 mmHg (mean, 17.3 mmHg) had a decrease in IOP of 6.9% (1.2 mmHg, P ⬍ 0.01) postoperatively. Subjects with a preoperative IOP greater than 21 mmHg (mean, 24.9 mmHg) experienced a 24.9% (6.2 mmHg, P ⬍ 0.01) decrease in their IOP postoperatively (Table 5). Strabismus Surgery Thirty-two eyes underwent strabismus surgery: 21 had inferior rectus recessions alone and 11 had inferior and medial rectus recessions simultaneously. The mean preoperative IOP in primary position was 18.5 ⫾ 2.8 mmHg, and 24.7 ⫾ 4.3 mmHg in upgaze (Table 2). Postoperative IOP in primary position was 16.1 mmHg and 16.9 mmHg in upgaze. This is a decrease of 2.4 mmHg (13.3%, P ⬍ 0.01) in primary position and 7.8 mmHg (31.2%, P ⬍ Table 2. Mean Intraocular Pressure Readings (mmHg) Characteristic Preop IOP, mean (SD) Primary position Upgaze Postop IOP, mean (SD) Primary position Upgaze Mean difference, (SD) Primary position Upgaze % Decrease Primary position (P value) Upgaze (P value) Decompression Strabismus Radiation 21.6 (4.6) 27.9 (6.8) 18.5 (2.8) 24.7 (4.3) 19.4 (4.5) 26.6 (9.3) 17.5 (3.0) 20.1 (4.7) 16.1 (2.8) 16.9 (3.7) 18.4 (5.2) 24.2 (7.1) ⫺4.1 (3.9) ⫺7.8 (5.8) ⫺2.4 (2.9) ⫺7.8 (4.5) ⫺1.0 (5.0) ⫺2.4 (5.8) 18.9% (P ⬍ 0.001) 27.9% (P ⬍ 0.001) 13.3% (P ⬍ 0.01) 31.2% (P ⬍ 0.01) 5.1% (P ⫽ 0.35) 9.0% (P ⫽ 0.17) IOP ⫽ intraocular pressure; SD ⫽ standard deviation. Danesh-Meyer et al. 䡠 IOP Changes after Graves’ Orbitopathy Table 3. Change in Intraocular Pressure After Orbital Decompression Based on Indication for Intervention Indication for Intervention Optic neuropathy (n ⫽ 80) Primary position (SD) Upgaze position (SD) Proptosis (n ⫽ 36) Primary position (SD) Upgaze position (SD) Intraocular Pressure Before Intraocular Pressure After Drop in Intraocular Pressure % Decrease in Intraocular Pressure P Value 22.9 (4.1) 30.1 (5.9) 17.9 (3.0) 20.9 (4.8) 5.0 (3.8) 9.2 (5.8) 21.6% 30.7% ⬍0.01 ⬍0.01 18.8 (4.7) 23.3 (6.5) 17.1 (2.9) 18.6 (4.5) 1.7 (3.7) 4.7 (4.6) 9.5% 20.1% ⬍0.01 ⬍0.01 SD ⫽ standard deviation. 0.01) in upgaze (P ⬍ 0.0001). There was no statistical difference in IOP in subjects who underwent inferior rectus recession alone compared with combined inferior and medial rectus recession. Orbital Radiation Twenty-eight subjects who underwent orbital radiation had treatment to both eyes. Sixty-eight percent had orbital radiation for optic neuropathy and 32% for acute orbital inflammation (Table 1). The mean pretreatment IOP was 19.4 ⫾ 4.5 mmHg in primary position and 26.6 ⫾ 9.3 mmHg in upgaze. The mean posttreatment value at 6- to 12-week follow-up was 18.4 ⫾ 5.2 mmHg, in primary position and 24.2 ⫾ 7.1 mmHg in upgaze, the mean decrease in IOP being 1 mmHg (5%, P ⫽ 0.35), in primary position and 2.4 mmHg (9%, P ⫽ 0.17) in upgaze. This difference was not statistically significant (Table 2). Subjects with pretreatment IOP measurement of less than 21 mmHg had a mean IOP value of 16.5 mmHg with a posttreatment IOP of 15.8 mmHg, a decrease of 0.5 mmHg (P ⫽ 0.20). Those subjects in the radiation group who had a pretreatment value of greater than 21 mmHg (mean, 23.9 mmHg) had a posttreatment IOP of 22.0 mmHg, a decrease of 1.9 mmHg (P ⫽ 0.76). Discussion This study demonstrates that IOP decreases significantly after orbital decompression and strabismus surgery in subjects with GO but does not decrease in subjects treated with orbital radiation. Orbital Decompression Orbital decompression resulted in a decrease in IOP postoperatively irrespective of the preoperative IOP. However, subjects with preoperative IOP values of 21 mmHg or higher had more than a threefold greater reduction in their postoperative IOP compared with subjects who started with an IOP less than 21 mmHg. These findings are supported by the results of other smaller studies. In a series of 22 eyes (12 subjects) that underwent orbital decompression, Dev et al.11 found a mean postoperative decrease in IOP of 3.0 mmHg. Seven of eight eyes that had preoperative IOP values greater than 21 mmHg showed a greater decrease in IOP postoperatively (mean of 5.6 mmHg). Ohtuska12 measured IOP in six subjects before and after orbital decompression. The mean IOP decreased from 23.3 to 18.8 mmHg after orbital surgery. Kalmann and Mourits13 also reported five subjects who had orbital decompression for GO who had a significant decrease in their postoperative IOP. Another study,14 which used the technique of fat removal orbital decompression, described a mean decrease in IOP of 8.5 mmHg in nine subjects with preoperative IOP greater than 21 mmHg. Algevere et al.4 reported three of five subjects in whom glaucoma was “cured” with pterional orbital decompression. However, the postoperative IOP values were not reported in the study. Several theories have been invoked in an attempt to explain the decrease in IOP after orbital decompression. Increased orbital contents in a confined orbital volume, as seen in GO, may contribute to elevated IOP by increasing intraorbital pressure and venous congestion,7,15 subsequently increasing episcleral venous pressure (EVP).16 The increase in orbital contents is secondary to enlargement of the extraocular muscles, deposition of glycosaminoglycans, and lymphocytic infiltration of orbital fat.17 Direct orbital manometry demonstrated higher orbital tissue tension and lower orbital compartment compliance (both factors are thought to be components determining retrobulbar pressure) Table 4. Change in Intraocular Pressure in Orbital Decompression Group: On and Off Glaucoma Medications Use of Glaucoma Medications Using glaucoma medications (n ⫽ 35) Primary position (SD) Upgaze position (SD) Not using glaucoma medications (n ⫽ 81) Primary position (SD) Upgaze position (SD) Intraocular Pressure Before Intraocular Pressure After Drop in Intraocular Pressure % Decrease in Intraocular Pressure 25.9 (2.9) 30.5 (3.7) 18.8 (2.7) 21.4 (4.2) 7.1 (3.0) 9.1 (5.1) 27.4% 30.0% ⬍0.001 19.8 (4.0) 26.9 (7.6) 17.0 (3.0) 19.6 (4.9) 2.8 (3.7) 7.3 (6.1) 13.9% 27.2% ⬍0.001 P Value SD ⫽ standard deviation. 147 Ophthalmology Volume 108, Number 1, January 2001 Table 5. Change in Intraocular Pressure after Treatment According to Preoperative Intraocular Pressure Range Preoperative Intraocular Pressure Categories Decompression (n ⴝ 116) Strabismus (n ⴝ 32) Radiation (n ⴝ 56) ⬍21 mm Hg Mean preoperative IOP (SD) Mean postoperative IOP (SD) Mean drop in IOP (SD) % Decrease P Value ⱖ21 mm Hg Mean preoperative IOP (SD) Mean postoperative IOP (SD) Mean drop in IOP (SD) % Decrease P value (n ⫽ 51) 17.3 (2.3) (n ⫽ 27) 17.8 (2.2) (n ⫽ 34) 16.5 (2.9) 16.1 (2.8) 15.5 (2.7) 15.8 (2.7) ⫺1.2 (2.8) 6.9 (P ⬍ 0.01) (n ⫽ 65) 24.9 (3.0) ⫺2.3 (0.71) 12.9 (P ⬍ 0.01) (n ⫽ 5) 23.0 (0.5) ⫺0.7 (1.4) 4.3 (P ⫽ 0.20) (n ⫽ 22) 23.9 (2.5) 18.7 (2.5) 19.4 (1.1) 22.0 (4.9) ⫺6.2 (3.5) ⫺3.6 (1.4) ⫺1.9 (4.5) 24.9 (P ⬍ 0.01) 15.7 (P ⫽ 0.11) 7.6 (P ⫽ 0.76) IOP ⫽ intraocular pressure; SD ⫽ standard deviation. in the orbits of subjects with GO.18 Other studies have shown that there is an increased retro-orbital pressure in GO that is relieved with orbital decompression.15,18,19 An increase in EVP causes a proportional increase in IOP, according to the Goldmann equation: IOP ⫽ aqueous inflow/outflow facility ⫹ EVP. Because decompression surgery decreases orbital pressure and venous congestion, it would be expected to reduce EVP.4 In fact, orbital decompression has been shown to allow filling of the ophthalmic vein in subjects who previously had no filling during orbital venography, suggesting a lowering of EVP.9,20 Thirty-five eyes that underwent orbital decompression were being treated with at least one topical glaucoma medication. These subjects were referred to the Neuro-ophthalmology Service already on glaucoma medications. The IOP significantly decreased in this subgroup from 25.9 mmHg preoperatively to 18.8 mmHg postoperatively, a mean decrease in IOP of 7.1 mmHg or 27%. Hence, most subjects had their IOP “normalized” to a value less than 21 mmHg as a result of orbital decompression. This suggests that there was a significant contribution to the elevated preoperative IOP from factors that were not being effectively treated by the glaucoma medication. Those subjects who underwent orbital decompression who had optic nerve compression as their indication for decompression had a greater decrease in their IOP postoperatively than did subjects with proptosis as their indication for surgery. Optic nerve compression is commonly seen in subjects with little or no proptosis and with a crowded orbital apex seen on imaging. It would follow that the smaller decrease in IOP among the subjects who had proptosis as their indication for surgery is because the proptosis itself has a decompressive effect. By displacing the orbital contents outside the bony orbit, there is a decrease in the effective volume of the contents that occupy the bony orbit. This limited additional space that proptosis offers may 148 allow more room for the congested orbital contents and subsequently less compression on the globe and subsequent elevation in IOP. Strabismus Surgery To our knowledge (after a literature search of MEDLINE), our study is the first to statistically evaluate changes in IOP before and after inferior rectus surgery in GO. Extraocular muscle surgery decreased IOP in subjects by an average of 2.4 mmHg (12.9%) in primary position and 4.9 mmHg (22.8%) in upgaze. The mechanism of the increased IOP on upgaze is thought to be related to inelasticity of the inferior rectus muscle. The inability to relax when the elevator pulls the eye upward results in compression of the globe and subsequent elevation in IOP.21,23 An average rise in IOP of approximately 2 mmHg in upgaze has been reported to occur in healthy volunteers.24 In many subjects with GO, the average increase of IOP in upgaze is significantly higher.22,25,32 Fishman and Benes29 demonstrated that there is a direct linear correlation between the amount of hypotropia as measured in prism diopters and the increase in IOP in upgaze. High-resolution computed tomography has demonstrated that an increased IOP in upgaze may be caused by attempts to rotate the globe against fibrosed and shortened extraocular muscle.30 This is usually attributed to restriction specifically of the inferior rectus muscle. In some subjects the inferior rectus also will be exerting a tethering effect in primary position. As the inferior rectus becomes more contracted, it tends to pull the eye downward. In these subjects, an effort has to be exerted against the inferior rectus even to bring the eyes into the primary position. This may increase IOP in the primary position by the same mechanism. Orbital Radiation Orbital radiation is a treatment modality used in the acute, active phase of GO. Soft tissue signs and optic neuropathy of GO have been reported to improve after radiation treatment. The effect of orbital radiation on proptosis and extraocular muscle function is less consistent.33,34 Extraocular muscle size does not change significantly after radiation therapy.35 In our study, orbital radiation did not result in any significant change in IOP. In some ways this is surprising because radiotherapy is known to decrease the inflammatory component of GO, which should decrease orbital volume. One possible explanation is that although radiation decreases the inflammatory reaction, the effect on orbital volume is less significant and therefore does not translate into a significant reduction in IOP. Longer follow-up time may have detected a reduction in IOP. Alternatively, it may be that the number of subjects in our study was too small to detect a smaller, but potentially significant, reduction in IOP after radiation. Our study suggests that in a significant number of subjects with GO, the elevated IOP is related to the underlying pathophysiology of GO. By relieving these factors the IOP can be lowered. Our study also highlights the difficulty of Danesh-Meyer et al. 䡠 IOP Changes after Graves’ Orbitopathy diagnosing glaucoma in subjects with concomitant GO. It has been suggested1 that ocular hypertension may be more common in subjects with GO (24%) compared with the age-matched general population (5%),36 but a smaller proportion of subjects with GO progress to have glaucomatous field defects develop. A number of different theories may explain this presumed lower incidence of glaucoma among ocular hypertensives, with GO, including less susceptible optic nerves or elevated IOP for shorter periods of the day (e.g., on attempted upgaze). Subjects with GO may adopt a chin-up position that places the globe slightly in downgaze, relieving the elevated IOP associated with upgaze, attempted upgaze, or even gaze in primary position (the IOP measured in this position may not reflect the average daily IOP). The limitations of this study include that it is a retrospective review of subjects who required intervention for GO. This represents a small portion of subjects with GO. Because there was no control group, a comparison could not be made between change in IOP in subjects undergoing intervention and those who had no intervention. Subjects in the orbital decompression group had their IOP measured at 1 to 2 weeks postoperatively. There is no long-term follow-up to determine whether the decline in IOP seen postoperatively is sustained. Subjects who underwent strabismus surgery had significant limitation of upgaze. For these subjects, it is difficult to assume a standardized technique for measuring IOP in upgaze. Some subjects had their eyes fixed in downgaze and had to exert effort to attempt to bring their globes into the primary position. Finally, this study did not include the evaluation of optic nerve appearance, visual acuity, and visual fields in subjects with elevated IOP. Therefore, a comment cannot be made on whether there was any change in optic nerve function after intervention. Despite these limitations, we believe that the large number of subjects studied that allow statistical evaluation makes our observations useful. First, our study increases the body of evidence that suggests that increased intraorbital pressure and orbital congestion with subsequent venous obstruction and increased EVP contribute significantly to elevating IOP in subjects with GO. This is the largest study of change in IOP in subjects with GO who underwent orbital or strabismus surgery or radiation. Second, this study is the first to demonstrate that strabismus surgery results in an appreciable decrease in IOP in subjects with GO. Third, our findings suggest that the approach to the patient with GO and elevated IOP should be modified from ocular hypertension in other settings. Although ocular hypertension seen in GO subjects may be caused by the coexistence of two relatively common conditions, the elevated IOP could be secondary to the underlying pathologic processes that occur in GO. Finally, subjects diagnosed with glaucoma who are undergoing orbital decompression or inferior rectus surgery may have decreased IOP postoperatively. Hence, GO subjects with a diagnosis of glaucoma should have their glaucoma status reevaluated after these two surgical procedures. References 1. Brailey WA, Eyre JWH: Guy’s Hospital Rep (Abstr Ophthalmol Rev) 1901;20:147– 8. 2. Cockerham KP, Pal C, Jani B, et al. The prevalence and implications of ocular hypertension and glaucoma in thyroidassociated orbitopathy. Ophthalmology 1997;104:914 –7. 3. Manor RS, Kurz O, Lewitus Z. Intraocular pressure in endocrinological patients with exophthalmos. Ophthalmologica 1974;168:241–52. 4. Algvere P, Almqvist S, Backlund EO. Pterional orbital decompression in progressive ophthalmopathy of Graves’ disease. Short-term effects. Acta Ophthalmol (Copenh) 1973;51: 461–74. 5. Haddad HM. Tonography and visual fields in endocrine exophthalmos. Report on 29 patients. Am J Ophthalmol 1967;64:63–7. 6. Vanni VF, Vozza R. Comportamento del tono oculare in vari tipidi esoftalmo. Boll Oculist 1960;39:189 –97. 7. Nordmann J. Lobstein A, Gherarrd JP, Levy JP. Presentation of 14 cases of glaucoma due to elevated ocular venous pressure. Ophthalmologica 1961;142:501–5. 8. Cheng H, Perkins, ES. Thyroid disease and glaucoma. Br J Ophthalmol 1967;51:547–53. 9. Cant JS, Wilson TM. The ocular and orbital circulations in dysthyroid ophthalmopathy. Trans Ophthalmol Soc U K 1974; 94:416 –29. 10. Dyer JA. The oculorotatory muscles in Graves’ disease. Trans Am Ophthalmol Soc 1977;74:425–56. 11. Dev S, Damji KF, DeBacker CM, et al. Decrease in intraocular pressure after orbital decompression for thyroid orbitopathy. Can J Ophthalmol 1998;33:314 –9. 12. Ohtsuka K. Intraocular pressure and proptosis in 95 patients with Graves’ ophthalmopathy. Am J Ophthalmol 1997;124: 570 –2. 13. Kalmann R, Mourits MP. Prevalence and management of elevated intraocular pressure in patients with Graves’ orbitopathy. Br J Ophthalmol 1998;82:754 –7. 14. Adenis JP, Robert PY, Lasudry JGH, Dalloul Z. Treatment of proptosis with fat removal orbital decompression in Graves’ ophthalmopathy. Eur J Ophthalmol 1998;8:246 –52. 15. Otto AJ, Koornneef L, Mourits MP, Deen-van Leeuen L. Retrobulbar pressure measured during surgical decompression of the orbit [published erratum appears in Br J Ophthalmol 1997;81:175]. Br J Ophthalmol 1996;80:1042–5. 16. Dallow RL, Netland PA. Management of thyroid ophthalmopathy (Graves’ disease). In: Albert DM, Jakobiec FA, editors. Principles and Practice of Ophthalmology. Philadelphia: WB Saunders; 1994; vol. 3, 1905–22. 17. Netland PA, Dallow RL. Thyroid ophthalmopathy. In : Albert, DM, Jackobiec FA, eds. Principles and Practice of Ophthalmology: Clinical Practice. Philadelphia: W.B. Saunders, 1994; vol. 5, 2937–55. 18. Riemann CD, Foster JA, Kosmorsky GS. Direct orbital manometry in patients with thyroid-associated orbitopathy. Ophthalmology 1999;106:1296 –302. 19. Otto AJ, Spekreije J. Intraorbital volume discrepancies and intraorbital pressure. Int Ophthalmol 1987;11:113– 4. 20. Aron-Rosa D, Morax PV, Aron JJ, Metzger J. Exophtalmies oedémateuses endocriniennes et blocage circulatoire veineux orbitaire. Intérêt des phlébographies. Ann Ocul (Paris) 1970; 203:1–24. 21. Metz HS. Restrictive factors in strabismus [review]. Surv Ophthalmol 1983;28:71– 83. 22. Zappia RJ, Winkelman JZ, Gay AJ. Intraocular pressure 149 Ophthalmology Volume 108, Number 1, January 2001 23. 24. 25. 26. 27. 28. 29. changes in normal subjects and the adhesive muscle syndrome. Am J Ophthalmol 1971;71:880 –3. Braley AE. Malignant exophthalmos. Am J Ophthalmol 1953; 36:1286 –90. Reader AL III. Normal variations of intraocular pressure on vertical gaze. Ophthalmology 1982;89:1084 –7. Gamblin GT, Harper DG, Galentine P, et al. Prevalence of increased intraocular pressure in Graves’ disease— evidence of frequent subclinical ophthalmopathy. N Engl J Med 1983; 308:420 – 4. Spierer A, Eisenstein Z. The role of increased intraocular pressure on upgaze in the assessment of Graves’ ophthalmopathy. Ophthalmology 1991;98:1491– 4. Allen C, Stetz D, Roman SH, et al. Prevalence and clinical associations of intraocular pressure changes in Graves’ disease. J Clin Endocrinol Metab 1985;61:183–7. Kazim M, Kennerdell JS. Elevated intraocular pressure and dysthyroid orbitopathy. Orbit 1991;10:211–5. Fishman DR, Benes SC. Upgaze intraocular pressure changes and strabismus in Graves’ ophthalmopathy. J Clin Neuroophthalmol 1991;11:162–5. 150 30. Lyons DE. Postural changes in IOP in dysthyroid exophthalmos. Trans Ophthalmol Soc U K 1971;91:799 – 803. 31. Nardi M, Barolomei MP, Romani A, Barca L. Intraocular pressure changes in secondary positions of gaze in normal subjects and in restrictive ocular motility disorders. Graefes Arch Clin Exp Ophthalmol 1988;226:8 –10. 32. Saunders RA, Helveston EM, Ellis FD. Differential intraocular pressure in strabismus diagnosis. Ophthalmology 1981;88: 59 –70. 33. Donaldson SS, Bagshaw MA, Kriss JP. Supervoltage orbital radiotherapy for Graves’ ophthalmopathy. J Clin Endocrinol Metab 1973;37:276 – 85. 34. Wiersinga WM, Smit T, Schuster-Uittenhoeve AL, et al. Therapeutic outcome of prednisone medication and of orbital irradiation in patients with Graves’ ophthalmopathy. Ophthalmologica 1988;197:75– 84. 35. Kao SC, Kendler DL, Nugent RA, et al. Radiotherapy in the management of thyroid orbitopathy. Computed tomography and clinical outcomes. Arch Ophthalmol 1993;111:819 –23. 36. Sommer A. Intraocular pressure and glaucoma. Am J Ophthalmol 1989;107:186 – 8.