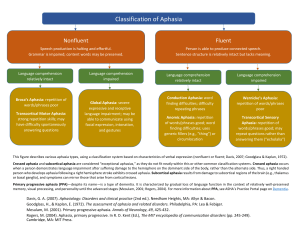
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/6670022 Computerised treatment of anomia in acute aphasia: Treatment intensity and training size Article in Neuropsychological Rehabilitation · January 2007 DOI: 10.1080/09602010543000064 · Source: PubMed CITATIONS READS 57 658 3 authors, including: Marina Laganaro Marie Di Pietro University of Geneva Hôpitaux Universitaires de Genève, Université de Genève 110 PUBLICATIONS 1,823 CITATIONS 35 PUBLICATIONS 551 CITATIONS SEE PROFILE SEE PROFILE Some of the authors of this publication are also working on these related projects: Rapid naming and reading skills in school‐aged children: A behavioral and ERP approach to the contribution of the lexical‐phonological processes View project Peripheral components of reading View project All content following this page was uploaded by Marie Di Pietro on 05 June 2014. The user has requested enhancement of the downloaded file. NEUROPSYCHOLOGICAL REHABILITATION 2006, 16 (6), 630– 640 Computerised treatment of anomia in acute aphasia: Treatment intensity and training size Marina Laganaro, Marie Di Pietro, and Armin Schnider Service de Rééducation, University Hospital, Geneva, Switzerland In this study we analysed the outcome of computer-assisted therapy (CAT) for anomia on eight acute aphasic patients. Since therapy for anomia generally leads to an item-specific effect, the aim of the present study was to investigate whether it is possible to enhance recovery from anomia by increasing the number of treated items. Two periods of five daily written-naming CAT sessions were compared: In one period the CAT included one set of 48 words (single list) and in the other period a double list of 96 items was treated. Seven out of eight patients improved in naming performance for treated items. Overall gains were superior after practising the double list, despite fewer item repetitions. These results suggest that the size of the effect of therapy for anomia depends more on the number of treated items than on the number of repetitions per item. The integration of these results within the framework of studies on intensity is discussed. INTRODUCTION The efficacy of aphasia therapy has been studied by comparing language recovery in treated and untreated aphasic patients. Although lack of conclusive proof has been suggested by some authors (Greener, Enderby, & Whurr, 1999; Lincoln et al., 1984; Meikle et al., 1979), a certain number of studies have demonstrated efficacy of therapy for aphasia (Basso, Capitani, & Correspondence should be sent to: Marina Laganaro, Service de Rééducation, Hopitaux Universitaires de Genève, Av. Beau-Séjour 26, CH-1211 Genève 14, Switzerland. E-mail: marina.laganaro@hcuge.ch This research was supported by Swiss National Science Foundation grant no. 105312100741/1. The authors wish to thank Myrna Schwartz, Kathleen Baynes and an anonymous reviewer for their helpful comments on a previous version of this paper. # 2006 Psychology Press, an imprint of the Taylor and Francis Group, an informa business http://www.psypress.com/neurorehab DOI:10.1080/09602010543000064 THERAPY FOR ANOMIA: INTENSITY AND TREATMENT SIZE 631 Vignolo, 1979; Mazzoni et al., 1995; Poeck, Huber, & Willmes, 1989). These group studies analysed the effect of an unspecified therapy for aphasia — based on a language stimulation approach — on standard aphasia assessment batteries. By contrast, single-case studies have focused on a specific language skill, with therapy based on a cognitive analysis of the impairment. In particular, there is convergent agreement that therapy for anomia can be effective, especially when a cognitive model-oriented approach is followed (Best & Nickels, 2000; Nickels, 2002). However, no precise prediction can be made about the size of the effect of a specific therapy for anomia with a specific aphasic patient. Indeed, several biographical and neurological factors, as well as factors linked to treatment type and conditions, may affect recovery (Basso, 1991, 1992). Among these, the treatment intensity seems to be an important predictor of the therapy outcome. Treatment intensity was manipulated in most studies in terms of number of sessions, and a higher number of therapy sessions was shown to have better outcome than regular intensity therapy (Basso & Caporali, 2001; Bhogal, Teasell, & Speechley, 2003; Denes, Perazzolo, Piani, & Piccione, 1996). Alternatively, therapy intensity has been analysed in terms of massed practice, showing better outcome when therapy sessions were grouped over a short period of time rather than distributed over a longer time period (Pulvermuller et al., 2001). Finally, intensity of treatment can be conceived in terms of drill or repetition, i.e., number of times the task, or particular items, are presented for practice during therapy. Indeed, cognitive therapy studies suggest that a single item presentation has no long-term effect on naming and that several task and item repetitions are necessary for long lasting effects (Howard et al., 1985a, b). Although the issue of the number of item presentations has not been addressed directly, most studies on efficacy of anomia treatment involved many repetitions of a few items (for example, 30 items presented 50 times in Miceli, Amitrano, Capasso, & Caramazza, 1996; 60 items practised up to 18 hours of therapy in the studies presented by Nickels & Best, 1996; 9 repetitions for each set of 30 items in Renvall, Laine, Laakso, & Martin, 2003). Here we address the study of intensity in terms of drill by varying the number of exposures to items during therapy as a function of the number of treated words. One way of increasing item drill during therapy is the introduction of computer-assisted treatment (CAT). CAT programs, designed to treat anomia, have shown encouraging results with chronic aphasic speakers (Bruce & Howard, 1987; Fink, Brecher, Schwartz, & Robey, 2002; Pedersen & Olsen, 2001). An item-specific improvement in naming was described by Bruce and Howard (1987) after five sessions with a computer program providing oral cue. Fink et al. (2002) also reported mostly item-specific benefits of a computer-assisted phonological cueing therapy in six chronic aphasic subjects. A written-naming task was used in the 632 LAGANARO, DI PIETRO, SCHNIDER study by Deloche et al. (1992) and an item-specific improvement with generalisation from the written to the oral modality was observed for most patients. Finally, Pedersen et al. (2001) reported efficacy of home-based CAT for anomia in three aphasic subjects. They also used a written-naming task and observed an item-specific improvement in two subjects. Although the issue of therapy intensity has not been explicitly addressed in CAT studies, authors suggested that the benefits of CAT may be linked to increased treatment in terms of item repetitions (Mortley, Enderby, & Petheram, 2001). Since the benefits of therapy for anomia are mostly itemspecific, it would be desirable to increase the number of treated items in order to increase the amount of recovery. But it is unknown whether improvement can be enhanced by increasing the number of items, or whether the amount of drill necessary per item, i.e., the number of times each item is presented as a therapy stimulus, limits the number of treatable items. In a previous study (Laganaro, Di Pietro, & Schnider, 2003), we analysed the outcome of computer-assisted therapy for anomia with chronic outpatients and with acute patients. In the group of acute aphasic patients, daily CAT sessions were added to individual aphasia therapy sessions, while CAT sessions were alternated with an equal number of clinical treatment sessions in the group of chronic patients. An item-specific effect of CAT for anomia was observed in all chronic patients and in three out of the seven acute patients. Our results with acute patients and the observation that the effect of therapy for anomia is mostly item-specific raised the question as to whether doubling the number of items practised during a limited number of sessions would increase recovery, or whether the number of items should be limited in order to increase repetition of treated items. This question is addressed by comparing gains in naming after CAT on one set of stimuli versus the double amount of stimuli for an equal number of sessions. METHOD Subjects Eight patients suffering from aphasia after stroke or traumatic brain injury (TBI) participated in the study. The inclusion criteria were based on the outcome of our previous study (Laganaro et al., 2003): Patients had mild to severe anomia among other aphasic symptoms; correct naming of at least 5% of the items on a screening picture-naming task; no stereotyped answers; no evident signs of apraxia of speech; mild or no comprehension impairment; and insight into their language difficulties. The patients were required to be motivated for therapy and for adding a therapy session to THERAPY FOR ANOMIA: INTENSITY AND TREATMENT SIZE 633 their daily planning. Concerning computer skills, patients had to be able to use the keyboard for writing or copying and the mouse for selecting a button on the screen. These abilities were assessed in a training session with the same computer program as was used in the study, but with different word stimuli. Patients were expected to be independent with the computer program after one or two training sessions. Only one patient, presenting with limb apraxia and executive dysfunction, was unable to work alone on the computer program after several training sessions and could not be included in the study. All the participants were in-patients and were between one and two months post-onset. They agreed to participate in the study by accepting a consent form specifically designed for this study according to institutional guidelines. The Montréal-Toulouse aphasia examination (Nespoulous et al., 1992) was used for assessing aphasia. Subjects’ demographic data and aphasia subtype are given in Table 1. All but two subjects were French native speakers; P2 and P3 were not native speakers, but French was their main language for over 20 years and the language they recovered best after their stroke. Therapy design A spoken picture-naming task of 144 items was used for assessment at baseline and after each therapy period. The naming material was made up of three sets of 48 words each and the corresponding line drawings selected from Alario et al. (2004) and Bonin, Chalard, Méot, and Fayol (2002). The items in the three lists were matched for name agreement, lexical frequency, words’ age of acquisition, length and syllabic structure. For therapy, two sets of items were grouped in order to form a double list of 96 items. These lists (the single list and the double list) were treated following a crossover design. After baseline testing, the double and the single list TABLE 1 Subjects’ demographic data Subjects Age Months post-onset P1 30 P2 P3 P4 P5 P6 P7 P8 48 56 38 48 39 76 62 Gender Aphasia type Aetiology Lesion 1 M TBI Left frontoparietal 1 1 1 1 2 1 2 M F F F F M M Transcortical sensory Conduction Mixed Broca Anomic Anomic Wernicke Anomic CVA TBI CVA TBI CVA CVA CVA Left temporoparietal Left frontotemporoparietal Left capsulo-lenticular Left temporal Left temporoparietal Left temporal Extended left perisylvian 634 LAGANARO, DI PIETRO, SCHNIDER were treated separately by CAT for one week each (5 sessions for each list) with a post-test assessment in between (Post-test 1) and at the end of the therapy period (Post-test 2). A third assessment (Post-test 3) was carried out 2 weeks after the end of the therapy period. Four patients worked on the single list in the first CAT period and on the double list in the second CAT period (group A) and four patients started with the double list and finished with the single list (group B). During the study period, all patients received one daily CAT session and one daily session of clinical therapy for aphasia. A written naming CAT program was used with all patients. The patients had to write the word corresponding to a coloured picture, which appeared on the screen with empty boxes corresponding to the number of letters of the target word. Two help buttons were available: One provided the pronounced word, and the second provided help on each letter of the word. The graphemes were provided incrementally, that is, the subject could press the button for help with the next letter only once he had written down the previous one (or copied it from an earlier cue). Only correct letters were displayed on screen. This CAT program was chosen because it involves several cognitive components (orthography, phonology, and semantics), since it has been suggested that a multicomponent treatment may work in different ways for different anomia types (Best, Howard, Bruce, & Gatehouse, 1997; Deloche et al., 1992; Nickels, 2002). Moreover, this same computer program led to significant benefit in three out of four patients presenting with mixed anomia in our previous study (Laganaro et al., 2003). During CAT sessions, patients worked alone, but could call a therapist for technical help. Each CAT session lasted from 30 to 60 minutes, depending on the patient’s speed, motivation or fatigue. For each therapy session the computer program recorded the time spent on it, the number of trials, and any help the subjects had used. Thus, the number of sessions was controlled during each CAT period, but the time spent on it and the number of item repetitions varied across patients. RESULTS Naming accuracy at baseline and post-tests was transcribed and scored online by trained speech and language therapists. Only first attempt correct responses within a delay of 5 seconds were scored as correct. Naming scores at baseline varied across patients from 8% to 58% correct, with similar proportional scores on the double and the single list for each patient (see Table 2). Pearson’s Chi square calculated on each patient’s naming accuracy on the single and the double list showed no significant difference between the two lists (all x2 , 1). THERAPY FOR ANOMIA: INTENSITY AND TREATMENT SIZE 635 TABLE 2 Correct naming (percent) at baseline, mean item repetitions during each CAT period (columns 4 and 6) and number of recovered items after each period (columns 5 and 7) on the single list and on the double list for the eight patients % correct at baseline 5 CAT sessions on 48 (single list) 5 CAT sessions on 96 (double list) Item repetitions per treatment period Recovered treated words (post–pre) n% Single list (48) % Double list (96) % Item repetitions per treatment period Recovered treated words (post–pre) n (%) Group A P1 P2 P3 P4 7 44 15 8 7 47 13 7 6 9 5 5 7 (15) 11 (23) 25 (52) 3 (6) 4.5 3 2.5 2.5 14 (15) 29 (30) 65 (68) 11 (11) Group B P5 P6 P7 P8 58 10 40 17 65 7 49 13 5 5 15 21 12 (25) 18 (37) 22 (46) 20 (42) 5 2.5 4.3 7.2 37 (39) 27 (28) 18 (19) 47 (49) Subject Table 2 also shows the amount of gains in naming the treated items for each patient after each CAT period and the number of item repetitions during each therapy period (i.e., the number of times each item was practised as a therapy stimulus during the CAT sessions). Gains are the increase in the number of correct naming responses in two consecutive testing periods. All but one patient (P4) improved significantly in picture naming after CAT (McNemar’s Chi square calculated on the correct naming score on the 144 items at post-test 3 versus baseline: for P4, x2 ¼ 3,7, p ¼ .06; for all other participants, x2 . 14.3, all ps , .01). It can be noticed that some patients practised each set of 48 items only once at each CAT session (thus, only half of the 96 items were treated during each session when practising the double list), while other patients repeated each set up to five times (see P8). Despite these differences, the number of item repetitions was always much higher for CAT on a single list than for CAT on the double list. Figure 1 shows percent correct naming on each list (48 items and 96 items) at baseline and at each post-therapy assessment period. A repeated measure ANOVA was carried out on correct naming scores before and after each therapy period with lists (single, double) and assessment period as within subject factors. A significant improvement in naming is observed after each 636 LAGANARO, DI PIETRO, SCHNIDER Figure 1. Correct naming (mean percent) on the single list and the double list for group A (single list treated first) and group B (double list treated first) at baseline and at each post-test CAT period, F(1, 7) ¼ 6.9, p , .05 after CAT on the single list, and F(1, 7) ¼ 40.2, p , .001 after CAT on the double list with a significant interaction with lists, respectively, F(1, 7) ¼ 7, p , .05 and F(1, 7) ¼ 35.7, p , .001, showing that improvement is limited to the single list after CAT on the single list and to the double list after CAT on the double list. Thus, improvement in naming is linked to CAT and is item-specific. THERAPY FOR ANOMIA: INTENSITY AND TREATMENT SIZE 637 Results at post-test 3 compared to post-test 2 were unchanged, F(1, 7) , 1, with no further improvement during the 2 weeks without therapy despite the ongoing clinical therapy. Proportional naming scores were similar on the single and the double list at the end of the study (see Figure l), which means that the absolute gain was double on the double list. A paired t-test calculated on total gains on the single and the double lists per subject shows significantly higher improvement on the double list, t(7) ¼ 23.28, p , .05. Thus, total gains were superior on the 96-items list than on the 48-items list despite less exposure to items (fewer item repetitions). This is further confirmed by an absence of correlation between the number of item repetitions for each patient during each treatment period and the related number of recovered items, r ¼ 2.131, N ¼ 16, p ¼ .63. DISCUSSION We described the effect of computer assisted therapy (CAT) for anomia on eight acute aphasic patients who underwent daily CAT sessions with a written-naming program, first on a single list (48 items) and then on a double list (96 items) and vice-versa. A significant improvement in naming after both CAT periods was observed, which was restricted to the treated items in both periods. These results are consistent with previous studies showing item-specific effect of therapy for anomia (Hillis & Caramazza, 1994; Laganaro et al., 2003; Miceli et al., 1996) and cannot be explained by generalisation, which would have led to improvement in both the treated and the untreated list. For the same reasons, spontaneous recovery and/or clinical aphasia therapy do not account for the observed improvement in naming pictures, which patients were unable to name at baseline. The main question addressed in this study was whether doubling the number of stimuli enhances treatment gains from anomia. Results showed similar proportional improvement on both lists, with numerically higher gains on the double list than on the single list. Improvement in naming was not directly linked to the number of times an item was practised, since the number of recovered words was higher when the double list was treated despite less item practice, and no correlation between drill and improvement was found. This result appears to contradict studies suggesting an effect of treatment intensity on recovery. However, in these studies intensity was manipulated in terms of number of sessions rather than in terms of drill, i.e., daily sessions compared to 2 – 3 weekly sessions (Denes et al., 1996) and 2 –3 hours per day compared to 1 hour (Basso & Caporali, 2001), or in terms of distribution of sessions over time (3 hours per day as compared to the same number of sessions over a longer period in Pulvermuller et al., 2001). In the present study the number of exposures to items during CAT 638 LAGANARO, DI PIETRO, SCHNIDER varied depending on the number of treated words. Our results suggest that 2– 3 item repetitions in daily therapy may be sufficient for some aphasic speakers to enable improvement in naming on a one-week period (at least in the acute stage). Indeed, the number of item repetitions in relation to the training-set size is very low by comparison with other CAT studies on anomia, which provided a high number of therapy sessions and of exposure to target items (20 items repeated up to 12 times in Fink et al., 2002; from 20 to 66 hours therapy for a maximum of 60 items in Pedersen et al., 2001; and up to 25 session in Deloche et al., 1992). However, we do not argue that therapy intensity does not play a role in recovery from anomia. First of all, the conditions of our study are in the form of an intensive therapy with a daily CAT session added to a daily clinical therapy session. Moreover, some patients spontaneously practised, twice or more, the CAT program during each session, in order to increase exposure to items (up to 20 times for P8). Taken together, our results suggest that, within the framework of intensive therapy for anomia, improvement is enhanced when the training size is increased, even in patients practising items at a high repetition rate. These individual variations of practice with a CAT program may probably reflect self-evaluation of needs in therapy and item repetitions. Although doubling the number of treated items increased improvement also in patients who spontaneously practised each list more than requested, neither list of items ever was completely recovered after therapy. This suggests that some items can be recovered under a certain amount of intensity, while others probably need more drill in order to be recovered. Thus, the numerically higher gains on the double list than on the single list despite a minor drill per item may reflect that doubling the number of treated items increased the number of items presenting characteristics that correlate with easier recovery. Further studies should be oriented to the analysis of the conditions predicting amount and speed of recovery as a function of training-set size and intensity, in order to guide item selection and duration in therapy for anomia. REFERENCES Alario, X., Ferrand, L., Laganaro, M., New, B., Frauenfelder, U. H., & Segui, J. (2004). Predictors of picture naming speed. Behavior Research Methods, Instruments, and Computers, 36, 140 – 155. Basso, A. (1991). Therapy of aphasia. In F. Boller & J. Grafman (Eds.), Handbook of clinical neuropsychology. Amsterdan: Elsevier. Basso, A. (1992). Prognostic factors in aphasia. Aphasiology, 6, 337– 348. Basso, A., Capitani, E., & Vignolo, L. A. (1979). Influence of rehabilitation on language skills in aphasia patients: A controlled study. Archives of Neurology, 36, 190– 196. Basso, A., & Caporali, A. (2001). Aphasia therapy or the importance of being earnest. Aphasiology, 15(4), 307– 332. THERAPY FOR ANOMIA: INTENSITY AND TREATMENT SIZE 639 Best, W., Howard, D., Bruce, C., & Gatehouse, C. (1997). A treatment for anomia: Combining semantics, phonology and orthography. In S. Chiat, J. Marshall, & J. Law (Eds.), Language disorders in children and adults, psycholinguistic approaches to therapy. London: Whurr. Best, W., & Nickels, L. (2000). From theory to therapy in aphasia: Where are we now and where to next? Neuropsychological Rehabilitation, 10, 231 – 247. Bhogal, S.K., Teasell, R., & Speechley, M. (2003). Intensity of aphasia therapy, impact on recovery. Stroke, 34(4), 987 –992. Bonin, P., Chalard, M., Méot, A., & Fayol, M. (2002). The determinants of spoken and written picture naming latencies. British Journal of Psychology, 93, 89– 114. Bruce, C., & Howard, D. (1987). Computer-generated phonemic cues: An effective aid for naming in aphasia. British Journal of Disorders of Communication, 22, 191– 201. Deloche, G., Ferrand, I., Metz-Lutz, M. N., Dordain, M., Kremin, H., Hannequin, D., Perrier, D., Pichard, B., Quint, S., Larroque, C., Cardebat, D., Naud, E., Bargego, C., Pradat, P., & Tessier, C. (1992). Confrontation naming rehabilitation in aphasics: A computerised written technique. Neuropsychological Rehabilitation, 2, 117– 124. Denes, G., Perazzolo, C., Piani, A., & Piccione, F. (1996). Intensive versus regular speech therapy in global aphasia: A controlled study. Aphasiology, 10(4), 385–394. Fink, R. B., Brecher, A., Schwartz, M. F., & Robey, R. R. (2002). A computer-implemented protocol for treatment of naming disorders: Evaluation of clinician-guided and partially self-guided instructions. Aphasiology, 16, 1061 –1086. Greener, J., Enderby, P., & Whurr, R. (1999). Speech and language therapy for aphasia following stroke. The Cochrane Database of Systematic Reviews (Issue 4). Oxford, UK: Update Software. Hillis, A., & Caramazza, A. (1994). Theories of lexical processing and rehabilitation of lexical deficits. In M. J. Riddoch & G. W. Humphreys (Eds.), Cognitive neuropsychology and cognitive rehabilitation. Hove, UK: Lawrence Erlbaum Associates Ltd. Howard, D., Patterson, K. E., Franklin, S., Orchard-Lisle, V., & Morton, J. (1985a). The facilitation of picture naming in aphasia. Cognitive Neuropsychology, 2, 49– 80. Howard, D., Patterson, K. E., Franklin, S., Orchard-Lisle, V., & Morton, J. (1985b). The treatment of word retrieval in aphasia: A comparison of two therapy methods. Brain, 108, 818– 829. Laganaro, M., Di Pietro, M., & Schnider, A. (2003). Computerised treatment of anomia in chronic and acute aphasia: An exploratory study. Aphasiology, 17(8), 709– 721. Lincoln, N. B., McGuirk, E., Mulley, G. P., Lendrem, W., Jones, A. C., & Mitchell, J. R. (1984). Effectiveness of speech therapy for aphasic stroke patients: A randomized controlled trial. Lancet, 8388, 1197 –1200. Mazzoni, M., Vista, M., Geri, E., Avila, L., Bianchi, F., & Moretti, P. (1995). Comparison of language recovery in rehabilitated and matched, non-rehabilitated aphasic patients. Aphasiology, 9, 553 –563. Meikle, M., Wechsler, E., Tupper, A., Benenson, M., Butler, J., Mulhall, D., & Stern, G. (1979). Comparative trail of volunteer and professional treatments of dysphasia after stroke. British Medical Journal, 14(2), 87– 89. Miceli, G., Amitrano, A., Capasso, R., & Caramazza, A. (1996). The treatment of anomia resulting from output lexical damage: Analysis of two cases. Brain and Language, 52, 150– 174. Mortley, J., Enderby, P., & Petheram, B. (2001). Using a computer to improve functional writing in a patient with severe dysgraphia. Aphasiology, 15(5), 443– 461. Nespoulous, J. L., Lecours, A. R., Lafond, D., Lemay, A., Puel, M., Joannette, Y., Cot, F., & Rascol, A. (1992). Protocole Montréal-Toulouse d’examen linguistique de l’aphasie (MT86). Isbergues, France: L’Ortho-Edition. 640 LAGANARO, DI PIETRO, SCHNIDER Nickels, L. (2002). Therapy for naming disorders: Revisiting, revising, and reviewing. Aphasiology, 16, 935 –979. Nickels, L., & Best, W. (1996). Therapy for naming disorders (Part II): Specifics, surprises and suggestions. Aphasiology, 10, 109 – 136. Pedersen, P. M. V. K., & Olsen, T. S. (2001). Improvement of oral naming by unsupervised computerised rehabilitation. Aphasiology, 15, 151 – 169. Poeck, K., Huber, W., & Willmes, K. (1989). Outcome of intensive language treatment in aphasia. Journal of Speech and Hearing Disorder, 54, 471–479. Pulvermuller, F., Neininger, B., Elbert, T., Mohr, B., Rockstroh, B., Koebbel, P., & Taub, E. (2001). Constraint-induced therapy of chronic aphasia after stroke. Stroke, 32(7), 1621– 1626. Renvall, K., Laine, M., Laakso, M. & Martin, N. (2003). Anomia treatment with contextual priming: A case study. Aphasiology, 17, 305 – 328. Manuscript received April 2004 Revised manuscript received January 2005 View publication stats