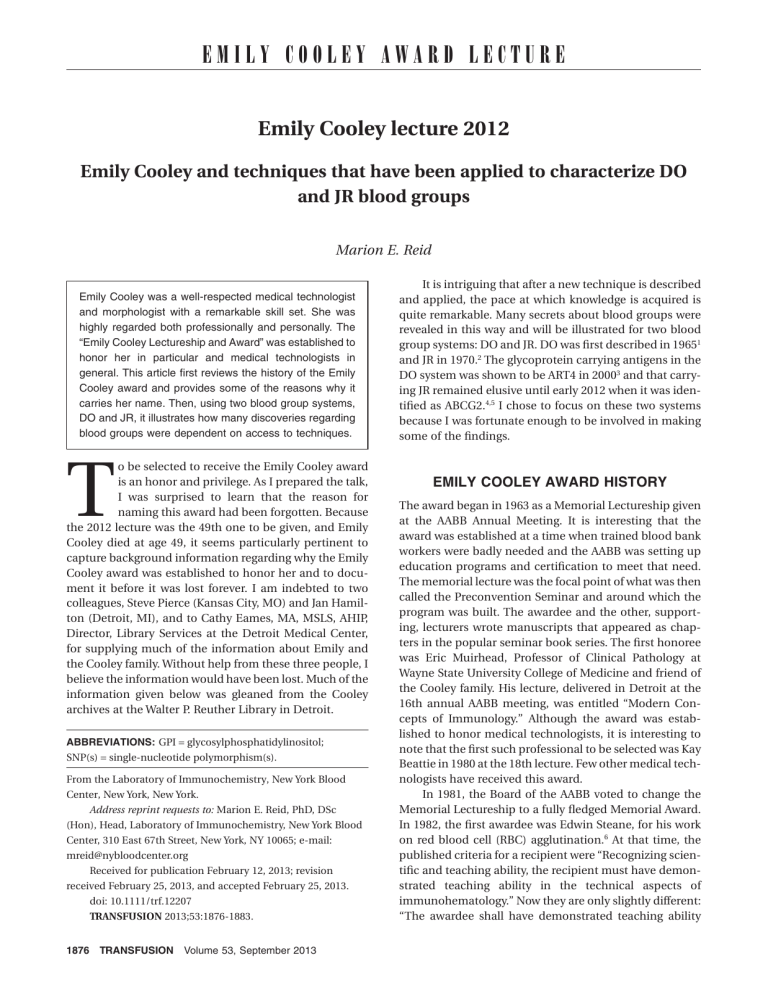
EMILY COOLEY AWARD LECTURE Emily Cooley lecture 2012 Emily Cooley and techniques that have been applied to characterize DO and JR blood groups Marion E. Reid Emily Cooley was a well-respected medical technologist and morphologist with a remarkable skill set. She was highly regarded both professionally and personally. The “Emily Cooley Lectureship and Award” was established to honor her in particular and medical technologists in general. This article first reviews the history of the Emily Cooley award and provides some of the reasons why it carries her name. Then, using two blood group systems, DO and JR, it illustrates how many discoveries regarding blood groups were dependent on access to techniques. T o be selected to receive the Emily Cooley award is an honor and privilege. As I prepared the talk, I was surprised to learn that the reason for naming this award had been forgotten. Because the 2012 lecture was the 49th one to be given, and Emily Cooley died at age 49, it seems particularly pertinent to capture background information regarding why the Emily Cooley award was established to honor her and to document it before it was lost forever. I am indebted to two colleagues, Steve Pierce (Kansas City, MO) and Jan Hamilton (Detroit, MI), and to Cathy Eames, MA, MSLS, AHIP, Director, Library Services at the Detroit Medical Center, for supplying much of the information about Emily and the Cooley family. Without help from these three people, I believe the information would have been lost. Much of the information given below was gleaned from the Cooley archives at the Walter P. Reuther Library in Detroit. ABBREVIATIONS: GPI = glycosylphosphatidylinositol; SNP(s) = single-nucleotide polymorphism(s). From the Laboratory of Immunochemistry, New York Blood Center, New York, New York. Address reprint requests to: Marion E. Reid, PhD, DSc (Hon), Head, Laboratory of Immunochemistry, New York Blood Center, 310 East 67th Street, New York, NY 10065; e-mail: mreid@nybloodcenter.org Received for publication February 12, 2013; revision received February 25, 2013, and accepted February 25, 2013. doi: 10.1111/trf.12207 TRANSFUSION 2013;53:1876-1883. 1876 TRANSFUSION Volume 53, September 2013 It is intriguing that after a new technique is described and applied, the pace at which knowledge is acquired is quite remarkable. Many secrets about blood groups were revealed in this way and will be illustrated for two blood group systems: DO and JR. DO was first described in 19651 and JR in 1970.2 The glycoprotein carrying antigens in the DO system was shown to be ART4 in 20003 and that carrying JR remained elusive until early 2012 when it was identified as ABCG2.4,5 I chose to focus on these two systems because I was fortunate enough to be involved in making some of the findings. EMILY COOLEY AWARD HISTORY The award began in 1963 as a Memorial Lectureship given at the AABB Annual Meeting. It is interesting that the award was established at a time when trained blood bank workers were badly needed and the AABB was setting up education programs and certification to meet that need. The memorial lecture was the focal point of what was then called the Preconvention Seminar and around which the program was built. The awardee and the other, supporting, lecturers wrote manuscripts that appeared as chapters in the popular seminar book series. The first honoree was Eric Muirhead, Professor of Clinical Pathology at Wayne State University College of Medicine and friend of the Cooley family. His lecture, delivered in Detroit at the 16th annual AABB meeting, was entitled “Modern Concepts of Immunology.” Although the award was established to honor medical technologists, it is interesting to note that the first such professional to be selected was Kay Beattie in 1980 at the 18th lecture. Few other medical technologists have received this award. In 1981, the Board of the AABB voted to change the Memorial Lectureship to a fully fledged Memorial Award. In 1982, the first awardee was Edwin Steane, for his work on red blood cell (RBC) agglutination.6 At that time, the published criteria for a recipient were “Recognizing scientific and teaching ability, the recipient must have demonstrated teaching ability in the technical aspects of immunohematology.” Now they are only slightly different: “The awardee shall have demonstrated teaching ability EMILY COOLEY AND BLOOD GROUPS and have made a major contribution to the field of immunohematology and transfusion medicine or cellular therapies.” The list of all awardees used to be published in each AABB Annual Meeting Program and is now on the AABB website (aabb.org). WHY THE AWARD USES EMILY COOLEY’S NAME Emily Cooley’s family Many of the males in Emily’s family had been lawyers. For example, her grandfather, Thomas McIntyre Cooley, was Dean of the University of Michigan Law School and Chief Justice of the Michigan Supreme Court. The Thomas M. Cooley Law School in Lansing is named in his honor. Emily Cooley’s father, Thomas Benton Cooley, broke with family tradition to become a physician, specializing in pediatric medicine. When he began his career, pediatrics was not a recognized specialty and some credit him as being the first modern pediatrician in Detroit, if not all of Michigan. He was a key agent in the development of the Children’s Hospital of Detroit and was Professor of Pediatrics at Wayne State University. Although not formally trained in hematology, it became his special area of interest and his most lasting contribution was the recognition of “erythroblastic anemia,” now better known as b-thalassemia major. Thomas Cooley was famous for his work on this anemia, which is often referred to as “Cooley’s anemia.” His detailed observations showed that this condition was inherited.7 Thomas Cooley became a leading advocate of the role of genetics in medicine, which was then largely ignored.8 Thomas Cooley had widely varied interests and believed strongly in the value of culture and a broad education in the humanities, especially for physicians. This attitude was reflected in the life of Emily Cooley, who, like her father, was a lively conversationalist on a wide range of topics. Emily Holland Cooley Emily was born in 1905 to Thomas Benton and Abigail Hubbard Cooley. She attended private girls’ schools and later graduated from Vassar College with a degree in landscaping. The gardens at her family’s home drew wide praise, but any thoughts of a career ended when she took over running the family household. This she did mainly because her father was ailing and her mother, a kindly, gracious woman, was often incapacitated with severe depression (then called melancholia). In this role, Emily assisted her father, handling his correspondence, driving him about town, and attending meetings with him. She did much of his library research. Having trained under Beaux Arts teachers in Paris, Emily was an accomplished artist. Her drawings were works of art and she pioneered this technical field for women. She used her talents to illustrate her father’s publications and lectures with detailed drawings of blood slides. Examples of her illustrations and exquisite depiction of blood cells are shown in Fig. 1. During the later years of Dr Cooley’s life, the family was in a poor financial state, so after her parents died (in 1945), Emily had to find a means of support. Given the medical education she had received by helping her father, she turned to medical technology, then a growing field, especially for women. She trained as a medical technologist at Henry Ford Hospital in Detroit and then earned an MSc degree at Wayne State University. Emily returned to Children’s Hospital in Detroit and soon became chief hematology technician and a mainstay of her department. She was highly regarded professionally as an excellent medical technologist and morphologist and personally as a warm, sensitive, intelligent, and generous human being and was looked up to and beloved by her colleagues (Fig. 2). In 1954, at age 49 years, she died suddenly of a ruptured cerebral aneurysm. She worked until a few hours before she died. In her honor, a technicians’ lounge was created by memorial contributions at Children’s Hospital and the AABB established a lectureship. Dedication at first lecture Wolf Zuelzer, noted pediatric hematologist who was then Director of Laboratories at Children’s Hospital in Detroit, introduced the first lectureship as follows: “In honoring the memory of Emily Cooley we are honoring the profession of which she was a dedicated and beloved member. This lecture is the first of a series of annual lectures, to be given by distinguished speakers at the meetings of the American Association of Blood Banks, in honor of an outstanding medical technologist. It is the beginning of a tradition intended to give recognition to a group of men and women whose contribution to modern medicine has not always been as highly appreciated as it deserves to be . . . I can think of no one worthier of the honor connected with this occasion than Emily Cooley.”9 BLOOD GROUP SYSTEMS AND THEIR ADVANCEMENT THROUGH TECHNIQUES In 1905, when Emily Cooley was born, ABO was the only known blood group system. By the time she died in 1954, there were 10 more. Today, there are 33 systems. Advances in knowledge about a blood group system are often only made after a new technique reveals certain secrets. Emily would be amazed at techniques now available to study blood cells. The rest of this article summarizes discoveries made in DO and JR blood group systems that were revealed when specific techniques became available. Volume 53, September 2013 TRANSFUSION 1877 REID Fig. 1. Illustrations hand drawn by Emily Cooley, scanned from “The Anemias” by Thomas Benton Cooley. Chapter 16 in Practice in Pediatrics, Vol. III, 1937. 1878 TRANSFUSION Volume 53, September 2013 EMILY COOLEY AND BLOOD GROUPS Amino acids 1 to 44 (or 22-44) are cleaved 45 Hy+/– Gly/Val 108 Jo(a+)/Jo(a–) Thr/Ile 117 DOMR+/– Arg/Glu 144 DOYA+/– Tyr/Asp 183 DOLG+/– Leu/Gln 225 Doa/Dob Asn/Asp 265 240 or 253 COOH Fig. 2. Picture of Emily Cooley. The Dombrock blood group system: nearly half a century of study RBC lipid bilayer Characteristics of Dombrock as revealed by hemagglutination Fig. 3. Dombrock glycoprotein showing the location of amino acids associated with antigens in the Dombrock blood group Classical hemagglutination, in the 1960s and 1970s, identified the first example of anti-Doa and anti-Dob,1,10 which define three phenotypes: Do(a+b-), Do(a+b+), and Do(a-b+). In 1985, Doa and Dob were placed in the Dombrock blood group system (DO; 014) by the International Society of Blood Transfusion (ISBT) Working Party on Terminology for Red Cell Surface Antigens.11 The high-prevalence antigens Gregory (Gya) and Holley (Hy) were individually reported in 196712,13 and 8 years later were shown to be phenotypically related: RBCs from Caucasians with the Gy(a-) phenotype are Hy-, and RBCs from black people of African descent with the Hyphenotype are Gy(a+w).14 Based on this observation, Gya and Hy were upgraded from the ISBT Series of High Incidence Antigens to the Gregory Collection.15 Later, the high-prevalence antigen Joa16 was shown to have a phenotypic association with Gya and Hy because RBCs with either the Gy(a-) phenotype or the Hy- phenotype are also Jo(a-).17,18 It was not until 199219 that a remarkable discovery was reported—still using hemagglutination! In addition to being Hy- and Jo(a-), Gy(a-) RBCs were shown to be Do(a-b-).20 Thus, RBCs with the Gy(a-) phenotype are the null phenotype of the DO blood group system. Upon this discovery, Gya, Hy, and Joa antigens were all assigned ISBT numbers in the DO blood group system.21,22 More recently, three new antigens have been added to the DO blood group system: DOYA, DOMR, and DOLG, bringing the system. Signal peptides and GPI-anchor motifs are cleaved from the membrane-bound glycoprotein. total to eight.23-25 Figure 3 is a stick figure showing the location of the critical amino acid associated with expression of each antigen. Properties of the Dombrock glycoprotein revealed by immunoblotting Immunoblotting confirmed that Gya, Hy, and Joa antigens are located on the same glycoprotein and revealed that the glycoprotein is attached to the RBC membrane by a glycosylphosphatidylinositol (GPI) linkage.26,27 On an immunoblot, the DO glycoprotein runs with a broad band with an apparent Mr of approximately 47,000 to 58,000 in sodium dodecyl sulfate–polyacrylamide gel electrophoresis under nonreducing conditions. The GPI nature of the DO glycoprotein was also revealed by Telen and colleagues,28 who passed RBC from a patient with paroxysmal nocturnal hemoglobinuria very slowly through a column coated with anti-AcHE. AcHE is also bound to the RBC membrane via a GPI linkage. The RBCs that did not attach to the column were tested for various antigens. Any antigen on a protein attached to the RBC membrane by a GPI linkage (namely, antigens in YT, DO, CROM, and JMH systems) is absent from paroxysmal nocturnal hemoglobinuria III RBCs. Volume 53, September 2013 TRANSFUSION 1879 REID In silico analysis and cloning the gene encoding the Dombrock glycoprotein Based on the knowledge that the DO glycoprotein is attached to the RBC membrane via a GPI linkage, and on the assignment of the DO to the short arm of chromosome 12,29 expressed sequence tags from terminally differentiating human erythroid cells were analyzed in silico. A candidate gene was detected within a BAC clone (GenBank Accession Number AC007655) and, by a series of experiments, was proven to be the gene that encodes the DO glycoprotein.3 This gene, ART4 was been renamed DO (GenBank Accession Number XM_017877). The DO glycoprotein (ART4) is a member of the mono-ADPribosyltransferase family, but has no demonstrable enzyme activity on the RBC.30,31 The DO gene consists of three exons distributed over 14 kb of DNA. The messenger RNA is predicted to encode a protein of 314 amino acids that has both a signal peptide sequence and a GPI-anchor motif.3 The signal peptide and GPI-anchor peptide are cleaved from the membranebound Do glycoprotein. Manual polymerase chain reaction–based assays reveal single nucleotide polymorphisms and provide a means to find antigen-negative blood Having identified the DO gene, it was a simple task to sequence DNA from people of known Do phenotype. The DO*A and DO*B alleles were shown to differ at three nucleotide positions. Two are silent nucleotide changes (c.378C>T; Tyr126Tyr and c.624T>C; Leu208Leu) and one is a missense change (c.793A>G; Asn265Asp), which encodes, respectively, Doa and Dob.3 As the two silent nucleotide changes are present in different combinations in various DO alleles,32 typically only the missense change is used to distinguish DO*A from DO*B. The ability to distinguish DO*A from DO*B makes it feasible to type patients and blood donors using polymerase chain reaction (PCR)-based techniques. This is a tremendous advantage, because due to the paucity of reliable antibodies, screening a large number of samples to find Do(a-) or Do(b-) blood donors by hemagglutination has been impossible. PCR-restriction fragment length polymorphism RFLP analysis has shown that Do(a+b-) donors previously typed by hemagglutination have both DO*A and DO*B alleles and so are, in fact, Do(a+b+). The nucleotide change associated with Hy+/Hy- is c.323G>T, which is predicted to encode Gly108Val. This change is associated with the absence of the Hy antigen and in most populations, is on an allele carrying c.793G (DO*B) and explains why RBCs with the Hy-negative phenotype are Do(a-b+). A nucleotide change of c.350C>T, predicted to encode isoleucine instead of threonine at Amino Acid Residue 117, is associated with the absence of the Joa antigen and is on an allele carrying c.793A (DO*A). 1880 TRANSFUSION Volume 53, September 2013 The genotype of people whose RBCs have the Jo(a-) phenotype can be DO*JO/DO*JO or DO*HY/DO*JO.33 Silenced DO alleles encode the Do(a-b-), Gy(a-), or DOnull phenotype. Several molecular bases have been described to encode this phenotype.32 No pathology has been observed with an absence of the entire DO glycoprotein [Gy(a-)]. People with the DOnull phenotype are apparently healthy. DNA array technology The ability to detect single nucleotide changes on DNA arrays is revolutionizing the way we provide antigennegative blood in transfusion medicine. Use of DNA arrays not only provides high-throughput analyses of multiple single-nucleotide polymorphisms (SNPs) on one chip but also electronically interprets and downloads the massive amount of data directly to a database.34-37 Because antibodies to antigens in the DO blood group system (especially anti-Dob) are rarely available as a single specificity with strength and volume to make accurate typing possible, this is the first instance where DNA-based analyses are more reliable than hemagglutination. Transfection and hybridoma technology The ability to transfect cells with DO cDNA provided a tool to not only study protein expression but also to immunize mice as the first step in the production of monoclonal antibodies (MoAbs) to Dombrock antigens.3 The availability of MoAb anti-Do has made it possible for the DO glycoprotein to be assigned the cluster of differentiation number CD297,38 and pepscan analyses using overlapping peptides (also known as pin technology) allow precise epitope mapping of MoAbs.39 The JR blood group system: more than 40 years of study Characteristics of Jr a as revealed by hemagglutination The high-prevalence blood group antigen Jra was first described in 1970 when previously unidentified antibodies in plasma and RBCs from Fujikawa, Tamura, Tad, Sorza, Powell, and Jacobs were shown to be mutually compatible.2 The antigen was named Jr after Rose Jacobs and in 1990 was placed in the ISBT 901 Series of HighIncidence Antigens and assigned the number 901005 by the ISBT Working Party on Terminology for Red Cell Surface Antigens.15 The Jr(a-) phenotype has been found in people of many ethnicities, including northern Europeans, Bedouin Arabs, a Mexican, and most commonly in Asians and notably in Japanese persons where in the Niigata region the prevalence is 1 in 58.40 Family studies showed the Jr(a-) phenotype was inherited as an autosomal recessive trait. EMILY COOLEY AND BLOOD GROUPS Secrets revealed by immunoprecipitation and transfection Attempts to immunoblot and immunoprecipitate the antigen using human anti-Jra were unsuccessful and indeed for many years, numerous laboratories, using various techniques, failed to define the membrane component carrying the Jra antigen. A MoAb anti-Jra (HMR0921)41 agglutinated human RBCs, reacted weakly by flow cytometry, and did not react by immunoblotting or immune precipitation. However, using cat RBCs this MoAb reacted strongly by flow cytometry and immuneprecipitated a protein of approximately 70 kDa. By mass spectrometry, this protein was identified as Abcg2, encoded by the cat ortholog of human transporter gene ABCG2.5 Saison and colleagues5 transfected an ABCG2 expression construct into K562 erythroleukemia cells (which do not express ABCG2) and by flow cytometry observed strong expression of ABCG2 and of Jra. They then used the transfected K562 cells and HMR0921 to immunoprecipitate ABCG2, showing that human Jra is carried on ABCG2. Secrets revealed by homozygosity by descent gene mapping Zelinski and coworkers4 used a novel approach to identify the gene encoding the protein carrying the Jra antigen— homozygosity by descent gene mapping. Genomic DNA, extracted from six Jr(a-) subjects (four probands) who had been identified by hemagglutination, was subjected to analysis on Affymetrix GeneChip Human Mapping 250K NspI array for SNPs. A homozygous region of 397,000 bp on the long arm of Chromosome 4 was identified. This region contained four validated genes: MEPE, SPPI, PKD2, and ABCG2. Only the product of ABCG2 was known to be expressed on RBCs. Therefore, PCR primers were designed and used to amplify the coding exons (2-16) of ABCG2 from the six Jr(a-) study subjects. Purified products were subjected to Sanger sequencing and silencing changes were observed in all. Concordant serologic and genetic results established that the Jr(a-) blood group phenotype is defined by ABCG2-null alleles. PCR-based assays reveal multiple SNPs in ABCG2 ABCG2 is located on Chromosome 4q22.1 and is composed of 16 exons spanning approximately 68.6 kb of gDNA coding for a 655 amino acid, 72.6-kDa glycoprotein, ABCG2 (also known as breast cancer resistance protein [BCRP]; mitoxantrone resistant protein [MXR]; CD338).42 ABCG2 is a multipass membrane glycoprotein and is an ATP-binding cassette (ABC) efflux transporter. The intracellular amino terminal domain, which harbors a nucleotide-binding domain (Residues 1 to ~396) with Walker A, Walker B, and ABC signature motifs, is joined to six putative transmembrane domains (Residues ~397 to 655) at its carboxyl terminus (reviewed in Woodward S (homodimer) 592 S–S 608 S572R novel D620N rs34783571 624 RBC lipid R575X bilayer E334X 394 645 Q531X G262X Walker B R236X R246X 288 Q244X Walker A Q126X 44 COOH 655 Q141K rs2231142 R113X ABC signature motif NH2 ABC = ATP-binding cassette = nucleotide binding domain (NBD) = Jr(a–) Fig. 4. ABCG2 showing the location of nonsense and missense changes involved in altered expression of Jra. et al.43). This structure is characteristic of ABC halftransporters, and to be functionally active, ABCG2 forms homodimers44 or homotetramers45 in the membrane. ABCG2 has wide tissue distribution and broad substrate specificity and is highly conserved across species. With the elucidation of the gene that encodes Jra,4,5 the ISBT Working Party on Red Cell Immunogenetics and Terminology ratified the establishment of a new blood group system, JR (ISBT 032; http://www.isbt-web.org). The JR blood group system contains the single antigen, Jra (032001). Numerous unique ABCG2 variant alleles defining Jr(a-), Jr(a+W/-), or Jr(a+W) phenotype have been described.4,5,46,47 Figure 4 shows the location of nonsense and missense changes on ABCG2. A list of alleles that have been reported to alter expression of Jra are tabulated on the ISBT website (http://www.isbt-web.org). In dbSNP, nearly 1300 synonymous and nonsynonymous SNPs are listed, and ABCG2 and ABCG2 are the subject of more than 2000 reports in the literature (June 2012). Revealing the connection between the Jr(a-) phenotype and ABCG2 has immediately provided a wealth of information about the JR blood group system. The large number of known JRnull blood donors are apparently healthy but they have not been studied in depth. Jr(a-) individuals (natural knockout) provide a large cohort in which to study the exact role and function of ABCG2 in normal physiology and pathologic conditions such as cancer. CONCLUDING REMARKS Techniques of a different nature allowed myself and colleagues to develop a homemade educational program, known as Bloodology. This program was presented at the Kids Museum Brooklyn, the American Museum of Natural Volume 53, September 2013 TRANSFUSION 1881 REID History in New York, and the Franklin Institute in Philadelphia. The various activities were popular among children and adults alike. Throughout my career, I indeed have been fortunate to be mentored by people who believed in my abilities more than did I. They challenged me to perform tasks I did not dream I could accomplish but I did my best, not wanting to disappoint them. I am indebted to them all and without them I would not have received this award. Thank you. ACKNOWLEDGMENTS 7. Cooley TB. The anemias. Practice in pediatrics, 1937. 8. Zuelzer W. Thomas B. Cooley (1871-1945), pediatric profiles. St Louis (MO): CV Mosby Company; 1957. 9. Zuelzer W. Emily Cooley: a seminar on advanced techniques in blood banking. Arlington (VA): American Association of Blood Banks; 1963. 10. Molthan L, Crawford MN, Tippett P. Enlargement of the Dombrock blood group system: the finding of anti-Dob. Vox Sang 1973;24:382-4. 11. Lewis M, Allen FH, Jr, Anstee DJ, Bird GW, Brodheim E, Contreras M, Crookston M, Dahr W, Engelfriet CP, Giles CM, Issitt PD, Jorgensen J, Kornstad L, Leikola J, Lubenko For information about Emily Cooley, I am particularly indebted to two colleagues: Steve Pierce from Kansas City for tenaciously pur- A, Marsh WL, Moore BPL, Morel P, Moulds JJ, Nevanlinna H, Nordhagen R, Rosenfield RE, Sabo B, Salmon Ch., suing leads and for supplying much of the information and Jan Yasuda J et al. ISBT Working Party on Terminology for Red Hamilton from Detroit, Michigan, for contacting the librarian at Detroit Medical Center and digging through the archives. I also Cell Surface Antigens: Munich report. Vox Sang 1985;49: 171-5. thank Cathy Eames, MA, MSLS, AHIP, Director of Library Services at the Detroit Medical Center who accepted our challenge and accessed archives at the Walter P. Reuther Library in Detroit. I wholeheartedly thank the numerous colleagues and collaborators with whom I have had the pleasure to work because without 12. Swanson J, Zweber M, Polesky HF. A new public antigenic determinant Gya (Gregory). Transfusion 1967;7:304-6. 13. Schmidt RP, Frank S, Baugh M. New antibodies to high incidence antigenic determinants (anti-So, anti-E1, anti-Hy and anti-Dp) [abstract]. Transfusion 1967;7:386. them I would not have received the Emily Cooley Award; there are too many to name but you know who you are and I extend my grateful appreciation to you. 14. Moulds JJ, Polesky HF, Reid M, Ellisor SS. Observations on the Gya and Hy antigens and the antibodies that define them. Transfusion 1975;15:270-4. CONFLICT OF INTEREST 15. Lewis M, Anstee DJ, Bird GWG, Brodheim E, Cartron J-P, Contreras M, Crookston MC, Dahr W, Daniels GL, Engel- The author declares that she has no conflicts of interest relevant to this manuscript submitted to TRANSFUSION. friet CP, Giles CM, Issitt PD, Jørgensen J, Kornstad L, Lubenko A, Marsh WL, McCreary J, Moore BPL, Morel P, Moulds JJ, Nevanlinna H, Nordhagen R, Okubo Y, Rosenfield RE, Zelinski T et al. Blood group terminology 1990. REFERENCES 1. Swanson J, Polesky HF, Tippett P, Sanger R. A “new” blood group antigen, Doa [abstract]. Nature 1965;206:313. 2. Stroup M, MacIlroy M Jr. Five examples of an antibody 3. 4. 5. 6. 1882 defining an antigen of high frequency in the Caucasian population [conference abstract], 23rd Annual Meeting of the American Association of Blood Banks, San Francisco, 1970:86. Gubin AN, Njoroge JM, Wojda U, Pack SD, Rios M, Reid ME, Miller JL. Identification of the Dombrock blood group glycoprotein as a polymorphic member of the ADPribosyltransferase gene family. Blood 2000;96:2621-7. Zelinski T, Coghlan G, Xiao-Qing L, Reid ME. ABCG2 null alleles define the Jr(a-) blood group phenotype. Nat Genet 2012;44:131-2. Saison C, Helias V, Ballif BA, Peyrard T, Puy H, Miyazaki T, Perrot S, Vayssier-Taussat M, Waldner M, Le Pennec PY, Cartron JP, Arnaud L. Null alleles of ABCG2 encoding the breast cancer resistance protein define the new blood group system Junior. Nat Genet 2012;44:174-7. Steane EA. Red blood cell agglutination: a current perspective. Seminar on Antigen-Antibody Reactions Revisited. Arlington (VA): American Association of Blood Banks; 1982. TRANSFUSION Volume 53, September 2013 ISBT working party on terminology for red cell surface antigens. Vox Sang 1990;58:152-69. 16. Jensen L, Scott EP, Marsh WL, MacIlroy M, Rosenfield RE, Brancato P, Fay AF. Anti-Joa: an antibody defining a high-frequency erythrocyte antigen. Transfusion 1972;12: 322-4. 17. Weaver T, Kavitsky D, Carty L, Dah LKE, Marchese M, Harris M, Draper E, Ballas SK. An association between the Joa and Hy phenotypes [abstract]. Transfusion 1984;24:426. 18. Brown D. Reactivity of anti-Joa with Hy-red cells [abstract]. Transfusion 1985;25:462. 19. Banks JA, Parker N, Poole J. Evidence to show that Dombrock (Do) antigens reside on the Gya/Hy glycoprotein [abstract]. Transfus Med 1992;2(Suppl 1):68. 20. Banks JA, Hemming N, Poole J. Evidence that the Gya, Hy and Joa antigens belong to the Dombrock blood group system. Vox Sang 1995;68:177-82. 21. Daniels GL, Moulds JJ, Anstee DJ, Bird GW, Brodheim E, Cartron J-P, Dahr W, Engelfriet CP, Issitt PD, Jorgensen J, Kornstad L, Lewis M, Levene C, Lubenko A, Mallory D, Morel P, Nordhagen R, Okubo Y, Reid M, Rouger P, Salmon C, Seidl S, Sistonen P, Wendel S, Zelinski T et al. ISBT Working Party on Terminology for Red Cell Surface Antigens: Sao Paulo report. Vox Sang 1993;65:77-80. EMILY COOLEY AND BLOOD GROUPS 22. Daniels GL, Anstee DJ, Cartron J-P, Dahr W, Issitt PD, Jørgensen J, Kornstad L, Lewis M, Levene C, Lomas-Francis C, Lubenko A, Mallory D, Moulds JJ, Okubo Y, Overbeeke M, 35. Hashmi G, Shariff T, Zhang Y, Cristobal J, Chau C, Seul M, Vissavajjhala P, Baldwin C, Hue-Roye K, Charles-Pierre D, Lomas-Francis C, Reid ME. Determination of 24 minor red Reid ME, Rouger P, Seidl S, Sistonen P, Wendel S, Wood- blood cell antigens for more than 2000 blood donors by field G, Zelinski T. Blood group terminology 1995. ISBT high-throughput DNA analysis. Transfusion 2007;47:736- Working Party on terminology for red cell surface antigens. Vox Sang 1995;69:265-79. 47. 36. Denomme GA, Johnson ST, Pietz BC. Mass-scale red cell 23. Mayer B, Thorton N, Yürek S, Wylie D, Hue-Roye K, Poole J, genotyping of blood donors. Transfus Apher Sci 2011;44: 93-9. Bartolmäs T, Salama A, Lomas-Francis C, Velliquette RW, Yazdanbakhsh K, Reid ME. New antigen in the Dombrock blood group system, DOYA, ablates expression of Doa and weakens expression of Hy, Joa and Gya antigens. Transfu- 37. Reid ME, Halter Hipsky C. Looking beyond HEA: matching SCD patients for RH variants. In: Moulds JM, Ness PM, Sloan SR, editors. Beadchip molecular immunohematology. New York: Springer Science+Business Media; 2010. sion 2010;50:1295-302. 24. Costa F, Hue-Roye K, Sausais L, Velliquette RW, Costa Ferreira E, Lomas-Francis C, Reid ME. Absence of DOMR, a new antigen in the Dombrock blood group system that weakens expression of Dob, Gya, Hy, Joa, and DOYA antigens. Transfusion 2010;50:2026-31. p. 101-20. 38. Parusel I, Kahl S, Braasch F, Glowacki G, Halverson GR, Reid ME, Schawalder A, Ortolan E, Funaro A, Malavasi F, Hardie D, Halder S, Buckley CD, Haag F, Koch-Nolte F. A panel of monoclonal antibodies recognizing GPI-anchored ADP-ribosyltransferase ART4, the carrier of the Dombrock blood group antigen. Cell Immunol 2005;236:59-65. 25. Karamatic Crew V, Poole J, Marais I, Needs M, Wiles D, Daniels G. DOLG, a novel high incidence antigen in the Dombrock blood group system [abstract]. Vox Sang 2011; 101(Suppl 1):263. 26. Spring FA, Reid ME. Evidence that the human blood group antigens Gya and Hy are carried on a novel glycosylphosphatidylinositol-linked erythrocyte membrane glycoprotein. Vox Sang 1991;60:53-9. 27. Spring FA, Reid ME, Nicholson G. Evidence for expression of the Joa blood group antigen on the Gya/Hy-active glycoprotein. Vox Sang 1994;66:72-7. 39. Wasniowska K, Jaskiewicz E, Czerwinski M, Syper D, Lisowska E. Mapping of peptidic epitopes of glycophorins A (GPA) and C (GPC) with peptides synthesized on plastic pins (Pepscan analysis). Transfus Clin Biol 1997;4:73-5. 40. Nakajima H, Ito K. An example of anti-Jra causing hemolytic disease of the newborn and frequency of Jra antigen in the Japanese population. Vox Sang 1978;35: 265-7. 41. Miyazaki T, Kwon KW, Yamamoto K, Tone Y, Ihara H, Kato 28. Telen MJ, Rosse WF, Parker CJ, Moulds MK, Moulds JJ. Evidence that several high-frequency human blood group antigens reside on phosphatidylinositol-linked erythrocyte membrane proteins. Blood 1990;75:1404-7. 29. Eiberg H, Mohr J. Dombrock blood group (DO): assign- T, Ikeda H, Sekiguchi S. A human monoclonal antibody to high-frequency red cell antigen Jra. Vox Sang 1994;66: 51-4. 42. Bailey-Dell KJ, Hassel B, Doyle LA, Ross DD. Promoter characterization and genomic organization of the human ment to chromosome 12p. Hum Genet 1996;98:518-21. 30. Koch-Nolte F, Haag F. Mono (ADP-ribosyl) transferases and related enzymes in animal tissues. In: Haag F, KochNolte F, editors. ADP ribosylation in animal tissues: structure, function, and biology of mono (ADP-ribosyl) transferases and related enzymes. New York: Plenum Press; 1997. p. 1-13. 31. Okazaki IJ, Moss J. Characterization of glycosylphosphatidylinositiol-anchored, secreted, and intracellular vertebrate mono-ADP-ribosyltransferases. Annu Rev Nutr 1999;19:485-509. 32. Reid ME, Lomas-Francis C, Olsson ML. The blood group antigen factsbook. 3rd ed. New York: Elsevier; 2012. 33. Rios M, Hue-Roye K, Øyen R, Miller J, Reid ME. Insights into the Holley-negative and Joseph-negative phenotypes. Transfusion 2002;42:52-8. 34. Hashmi G, Shariff T, Seul M, Vissavajjhala P, Hue-Roye K, Charles-Pierre D, Lomas-Francis C, Chaudhuri A, Reid ME. A flexible array format for large-scale, rapid blood group DNA typing. Transfusion 2005;45:680-8. 43. 44. 45. 46. 47. breast cancer resistance protein (ATP-binding cassette transporter G2) gene. Biochim Biophys Acta 2001;1520: 234-41. Woodward OM, Köttgen A, Köttgen M. ABCG transporters and disease. FEBS J 2011;278:3215-25. Leimanis ML, Georges E. ABCG2 membrane transporter in mature human erythrocytes is exclusively homodimer. Biochem Biophys Res Commun 2007;354:345-50. Xu J, Liu Y, Yang Y, Bates S, Zhang JT. Characterization of oligomeric human half-ABC transporter ATP-binding cassette G2. J Biol Chem 2004;279:19781-9. Hue-Roye K, Lomas-Francis C, Coghlan G, Zelinksi T, Reid ME. The JR blood group system (ISBT 032): molecular characterization of three new null alleles. Transfusion 2013;53:1575-9. Hue-Roye K, Zelinksi T, Cobaugh A, Coghlan G, LomasFrancis C, Miyazaki T, Reid ME. The JR blood group system: identification of alleles that alter expression. Transfusion 2013. doi: 10.1111/trf.12118. Volume 53, September 2013 TRANSFUSION 1883