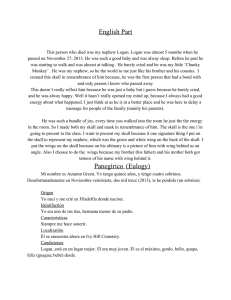
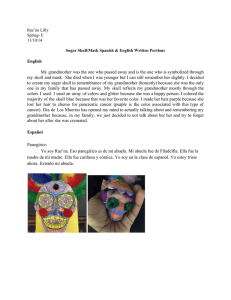
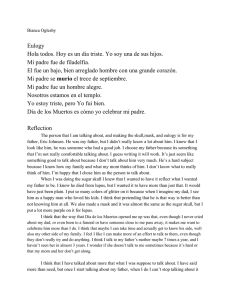
The Laryngoscope Lippincott Williams & Wilkins, Inc. © 2004 The American Laryngological, Rhinological and Otological Society, Inc. Comprehensive Algorithm for Skull Base Dural Lesion and Cerebrospinal Fluid Fistula Diagnosis Cem Meco, MD; Gerhard Oberascher, MD Objectives/Hypothesis: Skull base dural lesions and cerebrospinal fluid (CSF) fistulas are potentially vital conditions whose diagnosis can be challenging. The authors’ aim was to compose a comprehensive algorithm that combines the most modern diagnostic tools in easily applicable patterns to indicate a possible dural lesion or CSF fistula. Study Design: Prospective clinical study. Methods: The authors collected the data of all patients with suspicion of CSF fistula or dural lesion, or both, between January 1999 and December 2002. Beta–trace protein, 2-transferrin, and endoscopic and laboratory sodium fluorescein tests; high-resolution computed tomography; and magnetic resonance cisternography were used according to the symptoms and etiological factors. The results of the diagnostic tools that were used and intraoperative findings (in case of an operative treatment) were reviewed. Results: From 1999 to 2002, 236 patients were evaluated because of suspicion of dural lesion or CSF fistula, mostly after head trauma. Pattern I of the algorithm was applied for head trauma in dural lesion or CSF leak assessment, pattern II for postoperative CSF leaks, pattern III for evaluation of spontaneous CSF rhinorrhea, and pattern IV for the assessment of recurrent pneumococcal meningitis related to dural lesions without CSF fistula. By applying the patterns of this algorithm, a dural lesion or CSF leak that was also confirmed intraoperatively was detected in 48 patients. Conclusion: The four patterns of the new diagnostic algorithm described in the present study enable physicians to reliably clarify suspicions of dural lesions and CSF fistulas and aim to help them choose the best possible management. Each pattern uses the optimal combination of CSF tests and radiological imaging to reach a synergistic effect for precisely detecting dural lesions or CSF fistulas. Accordingly, this improves surgical decision-making when necessary. Key Words: From the Department of Otorhinolaryngology—Head and Neck Surgery, Salzburg University Paracelsus Medical School, Salzburg, Austria. Editor’s Note: This Manuscript was accepted for publication December 12, 2003. Send Correspondence to Cem Meco, MD, Department of Otorhinolaryngology—Head and Neck Surgery, Salzburg University Paracelsus Medical School, Müllner Hauptstrasse 48, A-5020, Salzburg, Austria. E-mail: c.meco@lks.at Laryngoscope 114: June 2004 Skull base, dural lesion, cerebrospinal fluid fistula, diagnosis, algorithm. Laryngoscope, 114:991–999, 2004 INTRODUCTION Diagnosis and management of dural lesions and cerebrospinal fluid (CSF) fistulas can sometimes be challenging, even for the most experienced skull base surgeons. Dural lesions can pose a wide variety of clinical presentations from clinically significant CSF fistulas to dehiscence or scar on dura without CSF leak. Because they can cause potentially vital complications, undiagnosed dural lesions and CSF fistulas (even if the leak is occult) should be considered as life-threatening situations. Bacterial meningitis is the major cause of morbidity and mortality in these patients, independent of the etiological factors, presenting type, or onset time.1–11 This aspect of the problem make it imperative for clinicians to detect, localize, and repair the dural defect and seal the CSF fistula. Dural lesions and CSF fistulas have been found to occur mostly after trauma, specifically, after 10% to 30% of skull base fractures.3–11 Other etiological factors such as neoplasms, congenital malformations, spontaneous CSF leaks, osteoradionecrosis, and prolactinoma therapy are more rare.8 –11 Nevertheless, all patients with a suspicion of a dural lesion and CSF fistula require a reliable state-of-the-art detection or exclusion. In this context, it is essential to diagnose even hidden dural lesions or occult fistulas to minimize the chance of secondary ascending meningitis. For clinically apparent CSF fistulas, a definitive and reliable diagnosis is also essential. Other pathological conditions such as vasomotor rhinitis or rhinorrhea attributable to unilateral autonomic dysfunction after injury might resemble and imitate CSF rhinorrhea, resulting in unnecessary procedures designed to repair presumptive dural defects.12 However, when to use which diagnostic tool to reach the most reliable and accurate result, while possibly avoiding the invasive methods at the beginning, remains an important issue. Moreover, interpreting the combination of CSF tests and imaging studies in conjunction with each other is another important issue, which correlates directly with the diagnosis, localization, Meco and Oberascher: Skull Base Dural Lesions 991 therapy, and, in case of surgery, approach selection and timing. The present study focuses on the development and validation of a state-of-the-art diagnostic algorithm, which allows physicians to identify and repair, possibly, all skull base dural lesions and CSF fistulas by using the most effective CSF diagnostic tests and imaging methods. Symptom-based and etiologically based (thus practical and easy to apply) diagnostic patterns of this algorithm are discussed, along with illustrative cases and possible pitfalls in the diagnosis of dural lesions and CSF fistulas. purpose, a new, faster, less expensive, and more sensitive quantitative CSF test, the -trace protein (TP) test, was performed simultaneously. The TP values calculated from nasal secretions were interpreted as described by Arrer et al.15 Moreover, in selected cases according to the need for further evaluation, the invasive sodium fluorescein (Na-fluorescein) test was used.8,16 After the lumbar intrathecal injection of 0.5 mL fresh, prepared 5% Na-fluorescein, by using a blue light filter, this dye was traced along the skull base with an endoscope as described by Messerklinger.17 The chemical part of this test, which remains the most sensitive test available, was performed as described by Oberascher and Arrer.18 PATIENTS AND METHODS Imaging Methods The setting of the Department of Otolaryngology (Salzburg University Medical School, Salzburg, Austria), which is a tertiary health care center, has been used for the present study. All cases with a suspicion of dural lesion and CSF fistula, as well as all head trauma patients whose diagnostic evaluation has been performed in our department between January 1999 and December 2002 were included. The cases found to have had a neoplasm as the etiological factor were excluded from the group because such cases demand other diagnostic considerations, placing them outside the scope of the present study. Diagnostic workup for the rest of the cases was performed according to etiological factors and symptoms, which were determined by anamnesis and clinical presentation. Topographical Diagnosis In case of a dural lesion or CSF fistula, defining its exact localization is an important part of the diagnostic process. This aspect is an obligatory part for the therapy planning, especially if surgery is needed. For all diagnostic tools that are capable of indicating localization, it is essential to interpret and report findings that are easily understandable for all persons involved in the further steps of management. For the standardization of reporting topographical diagnosis, a clinically oriented anatomical classification of the anterior skull base fractures and defects was used.8 This classification simplifies and constitutes an easily understandable topographical diagnostic terminology that improves communication with other specialists. It is based on anatomical landmarks, which are the main interest for diagnosis and therapy. To reach this aim, the anterior skull base was classified into three (Table I) clinically relevant anatomical compartments. Cerebrospinal Fluid Diagnostic Tests As the components of the diagnostic workup, a number of diagnostic tools were used. These consisted of CSF diagnostic tests and imaging methods. For first-line screening purposes, the gold standard of CSF diagnosis, the 2-transferrin (2-Tr) test, was used as described by Oberascher and Arrer13,14 in 1986. This qualitative test has shown its value for decades, and our laboratory has had a large experience with more than 2800 analyzed samples. In addition, beginning in January 2000, for the same TABLE I. Clinically Oriented Anatomical Classification of the Anterior Skull Base Fractures and Lesions. Compartment I IIa IIb III Laryngoscope 114: June 2004 992 Anatomical Region Frontal sinus Cribriform plate Fovea Sphenoid sinus After the CSF diagnostic tests, imaging methods are the second most important group of tools to diagnose dural lesions and CSF fistulas. The most valuable of them is high-resolution computed tomography (HR-CT), which has been shown to be highly effective, especially in post-traumatic cases.19,20 Highresolution computed tomography can identify the smallest bony defects along the skull base or indicate dural lesions through indirect signs, such as pneumatocephalus or fluid level in the sinuses. In our hospital, we use modern multislice CT systems that enable us to perform the scan of the entire skull base in 4 ⫻ 1- or 16 ⫻ 1-mm fashion in short time sequences of 40 or 10 seconds, respectively. Scanning is performed in the axial plane; thus, no special positioning of the patient is needed. The saved axial raw data are reconstructed in any desired plane. Fast, only-axial-plane scanning also reduces the radiation exposure of the patient. For the precise evaluation of the skull base, both axial and reconstructed coronal planes are needed. The frontal sinus posterior wall (compartment I) and sphenoid sinus lateral and posterior walls (compartment III) can best be assessed on axial plane scans, whereas cribriform plate (compartment IIa), fovea (compartment IIb), and sphenoid roof (compartment III) can be better visualized on coronal plane scans. Similarly, a meticulous examination of the temporal bone (high-resolution positron computed tomography [HR-PCT]) also requires images in axial and coronal planes. All patients in the present study have had either HR-CT of the anterior skull base or temporal bone, or both, according to their clinical findings, except in cases that were evaluated for a possible spontaneous CSF leak but had a negative finding on 2-Tr or TP test. Another imaging method that we use in our diagnostic workup is magnetic resonance cisternography (MR-Cis).20 –22 Although MR-Cis is an imaging examination, it can detect CSF leaks without the need of using contrast material or spinal puncture, by emphasizing and enhancing the CSF signal with suppression and subtraction of the adjacent background tissue signal. Tracing this high-level signal obtained from CSF in coronal and sagittal planes, especially in clinically active CSF leaks, also enables topographical diagnosis of one dural fistula or multilocal dural fistulas along the entire skull base, including the middle fossa and the petrous bone, with additional information such as brain herniation. Because it is a noninvasive and radiation-free examination, it can be safely repeated in cases with intermittent or subclinical occult leaks. In our study, MR-Cis was used in selected cases, mainly if there was clinically suspected rhinorrhea, to detect single or multiple dural lesions, but also to diagnose a possible meningoencephalocele or meningocele. Diagnostic Algorithm According to the presenting symptoms and etiological factors of each patient, the diagnostic tools have been systematically used to reach a diagnosis. Various decisive factors such as sensitivity, specificity, noninvasiveness, ease of use, applicability, and cost have been taken as criteria for their use. Our systematic Meco and Oberascher: Skull Base Dural Lesions approach to reaching a reliable diagnosis based on those criteria has been formatted and is shown in Figure 1 as a diagnostic algorithm. Clinical behaviors for different clinical presentations have been formatted in symptom-based and etiologically based patterns for easy applicability. The algorithm is based on the experience gained over decades in our department concerning diagnosis of dural lesions and CSF fistulas. In the present study, we prospectively applied this diagnostic algorithm, which is easy to use in clinical practice, for skull base dural lesions and CSF fistulas. The collected data were analyzed to check the validity of this new diagnostic algorithm. RESULTS Between January 1999 and December 2002, 236 consecutive cases in all were evaluated in our department for a possible dural lesion and CSF fistula. The majority of the cases occurred in patients who were evaluated after a head trauma, followed by patients assessed for spontaneous CSF rhinorrhea and postoperative CSF rhinorrhea and patients evaluated after recurrent pneumococcus meningitis (Fig. 2). We were not confronted with any other major etiological group. The four different groups had Fig. 1. Symptom-based and etiologically based diagnostic algorithm for dural lesions and cerebrospinal fluid fistulas. Laryngoscope 114: June 2004 Meco and Oberascher: Skull Base Dural Lesions 993 Fig. 2. Patients evaluated with a suspicion of dural lesions and cerebrospinal fluid (CSF) fistulas. their specific characteristics and symptoms at the time of presentation to our clinic. They were classified according to the possible underlying etiological factors by means of anamnesis and clinical presentation. This easy but necessary step helped in nearly all cases in choosing the appropriate diagnostic pattern to apply. Each diagnostic pattern had the best possible diagnostic tools, considering that these groups required different diagnostic approaches and interpretations concerning the dural lesions and CSF fistulas. Head Trauma: Pattern I Patients evaluated after a head trauma made up the largest group with 177 patients. Overall male-to-female ratio was 2.9:1. During the workup for head trauma evaluation, in addition to the 2-Tr and TP determinations in nasal secretions, all patients had HR-CT scans to rule out possible skull base fractures. For head trauma cases, radiological evaluation plays an extremely important role because a dural lesion or CSF fistula can occur only in the existence of a skull base fracture or, randomly, through the olfactory nerve bundles after microtears with the impact of trauma. In 177 head trauma patients, in 84 cases anterior skull base fractures, in 66 cases lateral skull base fractures, and in 27 cases no skull base fractures were found on a radiological basis. As expected, cases showing no fracture on HR-CT scan also had negative 2-Tr/TP test results (pattern Ia). When evaluated, anterior skull base fractures yielded diverse characteristics, from massive dislocated fractures with obvious CSF rhinorrhea to hardly detectable bony fissures. During the examinations 13 patients having positive 2-Tr and TP test results also had positive findings for fractures with dural lesion and CSF fistula on HR-CT scan (pattern Ib). Cerebrospinal fluid fistulas in those patients were validated and repaired by surgery. Eight patients had successful surgery with an endonasal approach. In the other five cases, transfrontal extradural approaches were chosen because the fractures either were in compartment I or were bilateral. From the point of the localization, 10 patients had a fistula at compartment II either alone or together with other compartments. Two patients had fistula only at compartment I, and one patient in compartment III. Of the remaining 71 cases, 67 had a negative 2-Tr or TP test result, and 4 had no statement for a CSF fistula Laryngoscope 114: June 2004 994 with 2-Tr or TP tests. All of the 71 cases had some degree of fracture reported by HR-CT examination. Moreover, some of them also had direct or indirect diagnostic signs for a dural lesion or CSF fistula indicated by the HR-CT. As the next diagnostic step, the invasive Nafluorescein test was performed in those cases. After the lumbar intrathecal application of 0.5 mL 5% Nafluorescein, only in three patients was it possible to find an active CSF fistula [pattern Ic]. Similarly, those patients also had successful surgery, all through an endonasal approach, which showed two fistulas at compartment II and one fistula at compartments II and III. More than 900 Na-fluorescein tests have been performed in our clinic to date, and no complications have been observed after the intrathecal application of Na-fluorescein. There remained 68 patients with negative results or results that were not interpretable (no statement) on 2-Tr and TP tests and negative Na-fluorescein test results, but with a positive HR-CT finding; this was the most challenging group to diagnose (pattern Id). A number of patients had, because of a blood cloth, mucosal edema, bone fragment or brain herniation, temporary closure of the dural lesion, consequently, hiding the fistula and resulting in negative findings on CSF testing. In those cases, the HR-CT findings such as pneumatocephalus or the degree of fracture dislocation played an extraordinary role. Of 68 patients in this group, 7 had pneumatocephalus with dislocations at compartment II (n ⫽ 4), compartment III (n ⫽ 1), and compartments II and III (n ⫽ 2). Pneumatocephalus alone is a direct sign of a dural lesion; thus we performed exploration endonasal endoscopic surgery in these patients, finding a dural lesion in each case, consistent with the HR-CT findings. Similarly, 12 patients had only evident dislocations (⬎3 mm) of the fracture with negative CSF test results and were graded as a having high suspicion for dural lesion in our clinic (Fig. 3). Exploration surgery through an endonasal endoscopic approach also confirmed a dural lesion in eight of those patients at compartment II (four cases), compartment III (two cases), and compartments II and III (two cases). In the other four patients found to have no dural lesion during surgery, the dislocated bone has been moved and replaced by a mucoperiosteal free flap to allow natural healing (compartment II, two cases; compartments I and II, one case; and compartments II and III, one case). EnMeco and Oberascher: Skull Base Dural Lesions testing (Fig. 4). However, nine other patients had surgery for conductive hearing loss caused by ossicula dislocation. Suspicion of Postoperative Cerebrospinal Fluid Fistula: Pattern II Fig. 3. Head trauma (pattern Id) in a 17-year-old male patient after head trauma. All cerebrospinal fluid tests were negative. However, high-resolution computed tomography (CT) indicated (arrow) a right-sided, 4-mm bony defect of the ethmoid roof with dislocation. Endoscopic endonasal exploration revealed a 1-cm dura tear. donasal approach was chosen in three cases, and one case had surgery through a transfrontal extradural approach. The remaining 49 cases had little or no dislocation of the fracture (⬍3 mm). We rated these findings as having a low suspicion for a dural lesion and as an indication for follow-up but not for an exploration surgery. However, in many of these cases, middle face fractures or frontal sinus anterior wall impression fractures accompanied the anterior skull base fracture. Nearly half of our 49 cases (24 cases) had an indication for reduction of these fractures and thus for a functional and reconstructive surgery. The indication for surgery was impression of the frontal sinus anterior wall in 16 cases and different types of Le Fort fractures in 8 of them. In these patients, during the same procedure, an endoscopic examination of the anterior skull base fracture was also performed by applying preoperative Na-fluorescein to exclude a dural lesion. Their fractures were distributed to compartment I (6 cases), compartments I and II (9 cases), and compartment II (9 cases). In none of the 24 cases was a dural lesion identified. In general, if we decide to perform surgery for dural lesions and CSF fistula, we routinely apply Na-fluorescein preoperatively so that we can better detect CSF leak or multiple CSF leaks or control water-tight sealing intraoperatively. The remaining 66 patients had a temporal bone fracture. When compared, patients with anterior and lateral skull base fractures showed different profiles. First, maleto-female ratios were 5:1 and 1.8:1, respectively. Second, 2-Tr and TP test results from nasal secretions were positive in 13 of 84 patients with anterior skull base fractures compared with 4 of 64 with temporal bone fractures indicating an otogenic CSF rhinorrhea (pattern Ie). In all four cases, localization of CSF fistula was detected by HR-PCT and MR-Cis. Middle fossa approach (2 cases), mastoidectomy (one case), and both of these combined (one case) were used to close the dural lesions. Other than these four patients, none of the 62 patients with temporal bone fracture had a surgical indication for a dural lesion based on the HR-PCT scan and findings on 2-Tr and TP Laryngoscope 114: June 2004 Another group that requires dural lesion and CSF fistula diagnosis is made up of patients who have postoperative suspected, generally unilateral rhinorrhea, especially after skull base or endonasal surgery. To rule out a postoperative CSF fistula (pattern II), we use, first, 2-Tr and TP tests and, second, MR-Cis or HR-CT (or both) according to the case. Since 1999, we have had three patients who had a postoperative CSF fistula. All of these cases occurred after a dural repair of the anterior skull base following either trauma or removal of a neoplasm. In all of them, the 2-Tr and TP test results and MR-Cis findings were positive, whereas HR-CT scan indicated a bony lesion. All cases were in compartments II and III (two cases in compartment II and one case in compartments II and III) and had revision surgery confirming the fistula through endonasal approach. Suspicion of Spontaneous Cerebrospinal Fluid Fistula: Pattern III In contrast to presentation after a trauma or surgery, sometimes patients present with clear rhinorrhea with suspicion of CSF without a definitive cause. These patients might be having spontaneous CSF fistulas, allergies, vasomotor rhinitis or other conditions, but a definitive evaluation is required so that a CSF fistula is not missed. In the time interval of the present study, we investigated 52 patients with a suspicion of spontaneous CSF fistula (pattern III). They all had clear nasal discharge. Twenty-three of them were beyond all suspicion Fig. 4. Head trauma (pattern Ie [otogenic cerebrospinal fluid rhinorrhea]) in a 64-year-old man with clinical cerebrospinal fluid rhinorrhea from the right-side nasal cavity. The –trace protein test result was positive. High-resolution computed tomography (CT) scan of the anterior skull base showed no fracture. Axial CT scan of the temporal bone demonstrated (arrows) a dislocated fracture of the posterior fossa accompanied with pneumatocephalus. The coronal planes indicated no fracture of the tegmen. Transmastoid revision and duraplasty were performed. Meco and Oberascher: Skull Base Dural Lesions 995 Fig. 5. Spontaneous cerebrospinal fluid (CSF) fistula (pattern IIIb) in a 55-year-old woman (body mass index, ⬎30 kg/m2). For 6 months, she had had intermittent rhinorrhea from the right side. After referral to our clinic she collected the secretion at home in a test tube. The –trace protein test result was positive. The high-resolution computed tomography (CT) scan (A) of the anterior skull base revealed (arrow) bony defect at the lateral wall of the fossa olfactoria. At the same site, magnetic resonance cisternography (B) showed (arrow) an active CSF fistula. Successful endoscopic repair was performed. because they had unilateral rhinorrhea. We performed screening 2-Tr and TP tests in the first line. Forty-six of the cases were negative (pattern IIIa), and six of them were positive (pattern IIIb). In cases with negative findings, there was no need to conduct other diagnostic evaluation because 2-Tr and TP tests can detect CSF with high sensitivity and specificity, especially concerning draining CSF fistulas. On the other hand, all cases with positive findings on 2-Tr or TP tests also had positive findings on HR-CT scan and MR-Cis testing (Fig. 5). They all presented with a unilateral rhinorrhea. Male-to-female ratio in this group was 1:5, and with the exception of one patient, all patients had a body mass index greater than 30 kg/m2. All six cases had endonasal endoscopic surgery to close the spontaneous CSF fistula, which was also confirmed during the operation. In four cases the dural lesions were located in compartment III, and in two cases in compartment II. Recurrent Pneumococcal Meningitis Without Cerebrospinal Fluid Fistula: Pattern IV The fourth group of patients that we evaluated for a possible dural lesion or CSF fistula comprised patients having recurrent pneumococcus meningitis with or without previous trauma. During the study period, we had four such patients. At the time of diagnostic workup, none of them had a positive finding on 2-Tr and TP testing (pattern IV). In every case, we found a suspected site at the HR-CT examination. To evaluate a possible meningocele or meningoencephalocele, we also performed MR-Cis, which showed meningoceles with CSF accumulation in two cases and a meningoencephalocele in one case (Fig. 6). All of these cases had exploration surgery verifying the site of dural thinning that was causing the meningitis. Their localization was compartment II in two cases and compartment III in two cases. Surgery was performed through endonasal approach in three cases and through a transfrontal intradural approach in one case. Overall Outcome In general, the symptom-based and etiologically based algorithm helped us to reach a reliable diagnose in Laryngoscope 114: June 2004 996 Fig. 6. Recurrent pneumococcal meningitis without cerebrospinal fluid (CSF) fistula (pattern IV): a 30-year-old man had meningitis 18 years earlier, with no trauma history. The patient was unconscious when admitted. Lumbar puncture showed purulent meningitis. High-resolution computed tomography (CT) scan (A) of the skull base showed a normal finding of the temporal bone but a bony defect of the left-side sphenoid sinus (arrow) with suspicion of brain herniation. Magnetic resonance cisternography (B) revealed (arrow) a meningoencephalocele. All CSF test results were negative. every case we evaluated. All patients who had surgery in each diagnostic group, as well as the patients who did not have surgery but had skull base fracture and negative results on CSF tests, were followed for at least 6 months. The follow-up relied on 2-Tr and TP tests, anamnesis, and nasal endoscopy in selected cases. Other than three cases of postoperative CSF fistula, all 2-Tr and TP test results were negative. Among the patients who were followed, no complication (eg, meningitis) has become known to us to date. The average age of 236 examined patients was 44.8 years (age range, 19 mo–75 y). With the stateof-the-art techniques it was possible to detect a dural lesion in 48 patients in a 4-year period. At the time of diagnosis, 33 patients had clinical or occult CSF fistula detected by 2-Tr and TP or Na-fluorescein tests. Head trauma was not only the most common cause for CSF fistula (20 cases) and for dural lesions (35 cases), but also the largest referral group for suspected dural lesions and CSF fistulas. Table II shows the topographic localization of the anterior skull base fractures in the entire head trauma group. Compartment II was the most common localization for anterior skull base fractures, as well as for dural lesions and CSF fistulas. Furthermore, it was also the most commonly affected region in other etiological groups, together with compartment III. Thus, the endonasal endoscopic microscopic approach was the most commonly used approach (79%) to repair dural lesions, which were indicated by the diagnostic algorithm. TABLE II. Topographic Localization of Anterior Skull Base Fractures. Pattern Compartment Ia Ib Ic Id Ie Total No. I I ⫹ II II II ⫹ III III Total No. — — — — — 0 2 3 6 1 1 13 — — 2 1 — 3 10 15 33 6 4 68 — — — — — 0 12 18 41 8 5 84 Meco and Oberascher: Skull Base Dural Lesions DISCUSSION When the etiological factors of dural lesions and CSF leaks are considered, head trauma has the highest incidence. Dural lesions and CSF leaks have been found to occur in 10% to 30% of skull base fractures.7 We had similar outcomes from our case material; 21.3% of all skull base fractures caused a dural lesion with or without CSF fistula. In more detail, anterior skull base fractures (33.3%) had an incidence of dural lesion that was five to six times higher than for temporal bone fractures (6.1%). Whatever the cause, diagnosis of CSF ensures a dural lesion. In our prospective study, the screening 2-Tr and TP tests diagnosed CSF from nasal secretions in 26 cases (54.2%), and Na-fluorescein testing was needed in only three trauma cases (6.3%) in 48 patients with dural lesions. On the other hand, in the remaining 19 cases, 15 cases (31.3%) with anterior skull base fracture did not have active CSF fistulas at the time of sample collection, which resulted in all CSF test findings being negative although there was a dural lesion. Temporary closure of CSF fistula could happen because of a blood clot, bony fragment, mucosal edema, prolapsed brain, brain edema, or the like.8,14 Similarly, in four cases (8.3%) with recurrent pneumococcal meningitis, all CSF test results were also negative. All but one of the four cases had meningoencephaloceles, either congenital or related to previous trauma. Inadequate integrity or healing of dura at its weakest site allowed bacterial migration from the skull base; the cases did not have a CSF fistula.8,14,23 Lack of CSF fistula differentiates this group from cases with meningoencephaloceles having CSF fistula, possibly because of elevated intracranial pressure forcing intracranial contents through inherently weakened areas such as widely pneumatized sinuses, which causes attenuated skull base areas with bony defects in the latter group.24 Independent from the sensitivity and specificity levels or limits of CSF diagnostic tests that may play a role in the diagnosis of occult CSF fistulas, even most modern CSF tests cannot help us if there is no CSF fistula. In such cases, imaging methods play a more important role; however, as has also been shown in our results, they are not able to diagnose every dural lesion or CSF fistula alone. Nonetheless, we ought to arrive at the correct diagnosis in these patients as well. Therefore, to overcome this problem, we need to combine diagnostic tools in a logical way that makes sense for every single case. Only by so doing can we decide to use the next costly, time-intensive, or, more important, invasive examination that might carry risks for the patient. During the decision-making process the valuable hints are in fact given by symptoms and etiological factors of patients. For that reason, it is our opinion that etiological factors play an important role during the planning of an efficient diagnostic process. Moreover, an efficient, reliable diagnosis for dural lesions and CSF fistulas can be reached only through a wellplanned diagnostic algorithm. As explained earlier in the present study, the core rationale is that none of the CSF diagnostic tests and imaging studies alone can identify dural lesions and CSF fistulas in all cases. All of them have their specific limits, which the other examination methods may or may not cover. Therefore, it is of utmost Laryngoscope 114: June 2004 importance to know which method to use when, and also for which patients, to clarify each case in the most specific, sensitive, noninvasive, and cost-effective way. As shown in our results and illustrative cases, our patients with different etiological factors required different examination methods for the definitive diagnosis. Nevertheless, it is also important to mention that, sometimes, even the combination of the most modern diagnostic tools leaves us a “gray zone,” in which we can only discuss a high or low level of suspicion of a dural lesion. In our series, we had such a “gray zone” in pattern Id. Concerning this pattern, within which patients had negative CSF test results but, somehow, had positive HR-CT findings after head trauma, all HR-CT findings showing a pneumatocephalus indicated a dural lesion. In the same way, in two-thirds of patients having bony dislocation of 3 mm or greater at the site of anterior skull base fractures a dural lesion was revealed intraoperatively. In contrast, bony dislocations of less than 3 mm were not an indication for surgery for us in patients in pattern Id who had a low level of suspicion for dural lesion; hence, these patients had only follow-up. With our concept, even in this challenging group, all lesions that most modern diagnostic tools are capable of diagnosing were diagnosed. Consequently, our diagnostic algorithm targets reduction in the number of undiagnosed cases of dural lesion and CSF fistula. Diagnosed cases must be adequately treated, to minimize the chance of secondary ascending meningitis.4 For example, 10% to 25% of cases of untreated head trauma with a CSF fistula proceed to meningitis with a mortality of approximately 10%.6,9 In every patient and with any etiological factor, if we ever have a suspicion of dural lesion or CSF fistula, any further step taken without state-of-the-art detection or exclusion of dural lesion and CSF fistula can, in principle, result in unpleasant consequences. Bateman and Jones12 have shown that lack of reliable diagnosis before surgery can result in unnecessary procedures designed to repair presumptive dural defects. On the other hand, again, to take the necessary measures in trying to prevent the potentially vital complications of dural lesions and CSF leaks, a reliable diagnosis is needed.1– 8 Equilibrium could be achieved by using a new diagnostic algorithm that indicates the definitive diagnosis. It is our strong belief that the definitive, reliable diagnosis obtained by use of our structured algorithm adds important advantages to the surgical planning, to surgery itself, and, as a consequence, to its outcome. In our opinion, these aspects have sometimes been partially neglected in previous studies focusing on surgical decision-making, techniques, and outcomes.9,10,25–27 Furthermore, other proposed diagnostic algorithms have generally targeted diagnosis of CSF fistulas regardless of the underlying etiological factors.11,28,29 Also, they have not sufficiently addressed the cases with a dural lesion but with no active CSF leak. They have concentrated mainly on the CSF diagnostic tests and imaging modalities in a single pattern for all cases. We think that, although these approaches seem to be practical, they could easily reach their limits and be inefficient when dealing with the problem cases. Not only has our experience from the past shown us, but also the Meco and Oberascher: Skull Base Dural Lesions 997 present study has verified, that it is more practical and efficient to use custom-made patterns for different etiological groups of patients. For example, the patient shown in Figure 5 had a clear spontaneous nasal discharge identified as CSF by 2-Tr and TP tests, and HR-CT showed a bony defect on the skull base requiring MR-Cis to localize the point of the leak, as well as to rule out a possible meningoencephalocele or multiple fistulas that might have been overlooked otherwise. Magnetic resonance cisternography has been reported as an efficacious and costeffective imaging technique, with sensitivity, specificity, and accuracy as high as 87%, 57%, and 78%, respectively, along with the recommendation of combining HR-CT scans.21 On the other hand, as in the patient shown in Figure 3, after a head trauma resulting in skull base fracture and epistaxis, the CSF test results were negative but the HR-CT showed a severe bony dislocation in compartment II. In such cases, MR-Cis would not bring any additional information because there is no active CSF leak. Although there are dural lesions, temporary closure of the CSF fistula can happen, as mentioned earlier in the present study. There is no doubt that the most challenging patients are those who have a dural lesion but at the time of presentation are having a temporary closure of the CSF fistula. Nevertheless, MR-Cis can give valuable information even if the CSF test results are negative. This is true when it is used for the indicated group, as in the patient shown in Figure 6, who was admitted to our clinic with recurrent pneumococcal meningitis without a CSF leak. Magnetic resonance cisternography revealed a meningoencephalocele at compartment III, which had inadequate dural integrity as observed during endoscopic repair. Because of such cases and also, more challenging cases, there is a need for a comprehensive, symptom-based and etiologically based diagnostic algorithm to emphasize the advantages and minimize the disadvantages of diagnostic tools for reaching reliable and definitive diagnosis. CONCLUSION The present prospective study has focused on a practical approach to dural lesions and CSF fistulas. Using our anamnesis-guided, etiologically based, and symptombased algorithm, patients were divided into four groups. Through the combination of the most modern CSF tests and imaging methods available, patients in each group were evaluated for the most favorable and precise diagnosis. While developing the diagnostic patterns of our algorithm, ease of use, effectiveness, and noninvasiveness were the main considerations. These measures enable a broader base of use among different specialties. In general, the aim of this algorithm is to help surgeons indicate an enhanced diagnosis, whether or not there is a dural lesion or CSF fistula. In case of a dural lesion, the algorithm extensively targets detection of the site of the lesion (or lesions). Although there are controversies among different centers about dural lesion and CSF fistula management, especially regarding possible surgery timing and approach, the enhanced diagnosis reached by the algorithm in the present study would help us achieve the optimal management for each case. Each pattern of this comprehensive, symptom-based and etiologically based alLaryngoscope 114: June 2004 998 gorithm uses the optimal combination of CSF tests and radiological imaging to reach a synergistic effect for precisely detecting dural lesions and CSF fistulas that has not been reached previously. Accordingly, this would help us to improve our decision-making for the most favorable therapy, especially concerning whether or not surgery is indicated. Furthermore, the algorithm enables surgeons to apply the most appropriate surgical approach for each patient from a spectrum of minimally invasive endoscopic techniques to neurosurgical approaches. BIBLIOGRAPHY 1. Pappas DG Jr, Hammerschlag PE, Hammerschlag M. Cerebrospinal fluid rhinorrhea and recurrent meningitis. Clin Infect Dis 1993;17:364 –368. 2. Crawford C, Kennedy N, Weir WRC. Cerebrospinal fluid rhinorrhea and Haemophilus influenza meningitis 37 years after a head injury. J Infect 1994;28:93–97. 3. Hilary AB. Prophylactic antibiotics for posttraumatic cerebrospinal fluid fistula: a meta-analysis. Arch Otolaryngol Head Neck Surg 1997;123:749 –752. 4. Bernal-Sprekelsen M, Bleda-Vazquez C, Carrau RL. Ascending meningitis secondary to traumatic cerebrospinal fluid leaks. Am J Rhinol 2000;14:257–259. 5. Choi D, Spann B. Traumatic cerebrospinal fluid leakage: risk factors and the use of prophylactic antibiotics. Br J Neurosurg 1996;10:571–575. 6. Eljamel MS, Foy PM. Acute traumatic CSF fistulae: the risk of intracranial infection. Br J Neurosurg 1990;4:381–385. 7. Marentette LJ, Valentino J. Traumatic anterior fossa cerebrospinal fluid fistulae and craniofacial considerations. Otolaryngol Clin North Am 1991;24:151–163. 8. Oberascher G. Rhinoliquorrhoe-otoliquorrhoe. HNO 1998;3: 197–200. 9. Hegazy HM, Carrau RL, Synderman CH, Kassam A, Zweig J. Transnasal endoscopic repair of cerebrospinal fluid rhinorrhea: a meta-analysis. Laryngoscope 2000;110:1166 –1172. 10. Gassner HG, Ponikau JU, Sherris DA, Kern EB. CSF rhinorrhea: 95 consecutive surgical cases with long term follow-up at the Mayo Clinic. Am J Rhinol 1999;13: 439 – 447. 11. Simmen D, Bischoff T, Schucknecht B. Erfahrungen mit der Abklärung von Frontobasisdefekten, ein diagnostisches Konzept. Laryngorhinootologie 1997;76:583–587. 12. Bateman N, Jones NS. Rhinorrhoea feigning cerebrospinal fluid leak: nine illustrative cases. J Laryngol Otol 2000; 114:462– 464. 13. Oberascher G, Arrer E. First clinical experience with 2transferrin in cerebrospinal fluid oto- and rhinoliquorrhea. HNO 1986;34:151–155. 14. Oberascher G, Arrer E. Efficiency of various methods of identifying cerebrospinal fluid in oto- and rhinorrhea. Otorhinolaryngology 1986;48:320 –325. 15. Arrer E, Meco C, Oberascher G, Piotrowski W, Albegger K, Patsch W. -trace protein as a marker for cerebrospinal fluid rhinorrhea. Clin Chem 2002;48:939 –941. 16. Stammberger H, Greistorfer K, Wolf G, Luxenberger W. Operativer Verschlu von Liquorfisteln der vorderen Schädelbasis unter intrathekaler Natriumfluorezeinanwendung. Laryngothinootologie 1997;76:595– 607. 17. Messerklinger W. Nasenendoskopie: Nachweis, Lokalization und Differentialdiagnose der nasalen Liquorrhoe. HNO 1972;20:268 –271. 18. Oberascher G, Arrer E. A new method for using fluorescein to demonstrate oto- and rhinoliquorrhea. Arch Otorhinolaryngol 1996;243:117–120. 19. Lloyd MNH, Kimber PM, Burrows EH. Post-traumatic cerebrospinal fluid rhinorrhea: modern high definition computed tomography is all that is required for the effective demonstration of the site of leakage. Clin Radiol 1994;49: 100 –103. Meco and Oberascher: Skull Base Dural Lesions 20. Shetty PG, Schroff MM, Sahani DV, Kirtane MV. Evaluation of high-resolution CT and MR cisternography in the diagnosis of cerebrospinal fluid fistula. AJNR Am J Neuroradiol 1998;19:633– 639. 21. El Gammal T, Sobol W, Wadlington VR, et al. Cerebrospinal fluid fistula: detection with MR cisternography. AJNR Am J Neuroradiol 1998;19:627– 631. 22. El Jamel MS, Pidgeon CN, Toland J, Phillips JB, O’Dwyer AJ. MRI cisternography and the localization of CSF fistulae. Br J Neurosurg 1994;8:433– 437. 23. Schick B, Weber R, Mosler P, Keerl R, Draf W. Langzeitergebnisse frontobasaler Duraplastiken. HNO 1997;45:117–122. 24. Schlosser RJ, Bolger WE. Management of multiple spontaneous nasal meningoencephaloceles. Laryngoscope 2002;112: 980 –985. Laryngoscope 114: June 2004 25. Lanza DC, O’Brien DA, Kennedy DW. Endoscopic repair of cerebrospinal fluid fistulae and encephaloceles. Laryngoscope 1996;106:1119 –1125. 26. Anand VK, Murali RK, Glasgold MJ. Surgical decisions in the management of cerebrospinal fluid rhinorrhea. Rhinology 1995;33:212–218. 27. Park JI, Strelzow VV, Friedman WH. Current management of cerebrospinal fluid rhinorrhea. Laryngoscope 1983;93: 1294 –1300. 28. Zapalac JS, Marple BF, Schwade ND. Skull base cerebrospinal fluid fistulas: a comprehensive diagnostic algorithm. Otolaryngol Head Neck Surg 2002;126:669 – 676. 29. Marshall AH, Jones NS, Robertson IJA. An algorithm for the management of CSF rhinorrhea illustrated by 36 cases. Rhinology 1999;37:182–185. Meco and Oberascher: Skull Base Dural Lesions 999