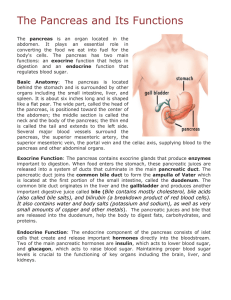
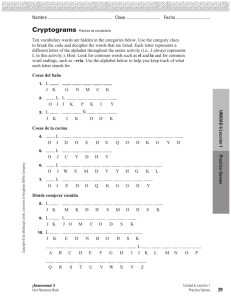
Lección 9. Cohesión y coherencia ¡Domínalo! Médico cirujano Nombre del alumno: Instrucciones: Este documento incluye la tarea que debes hacer para la lección 9. Lee las instrucciones cuidadosamente antes de elaborarla. Antes de enviar tu actividad, toma en cuenta que debes tenerla totalmente conformada por todos los elementos solicitados, mismos que se encontrarán en la rúbrica. Una vez terminada tu actividad, guárdala en el portafolio de aprendizaje y sigue las instrucciones de la guía académica. Valor de la tarea: 13 puntos. Se tomará en cuenta para la evaluación de esta tarea: - - - PARTE A. Diagrama: Tras leer el texto Pancreas: Function, Location & Diseases, completa con vocabulario relacionado a esta lectura el diagrama posterior; con ello se confirma que reconoces la cohesión del texto. PARTE B. En un siguiente espacio lee los tres textos; identifica aquél que no posee cohesión ni coherencia y en un máximo de 80 palabras en español justifica tu respuesta; apóyate en los elementos revisados en la lección. PARTE C. Redacta la idea principal de cada uno de los textos en español. PARTE A Pancreas: Function, Location & Diseases The pancreas is an abdominal organ that is located behind the stomach and is surrounded by other organs, including the spleen, liver and small intestine. The pancreas is about 6 inches (15.24 centimeters) long, oblong and flat. The pancreas plays an important role in digestion and in regulating blood sugar. Three diseases associated with the pancreas are pancreatitis, pancreatic cancer and diabetes. Function of the pancreas The pancreas serves two primary functions, according to Jordan Knowlton, an advanced registered nurse practitioner at the University of Florida Health Shands Hospital. It makes "enzymes to digest proteins, fats, and carbs in the intestines" and produces the hormones insulin and glucagon, he said. Dr. Richard Bowen of Colorado State University's Department of Biomedical Sciences wrote in Hypertexts for Pathophysiology: Endocrine System, "A well-known effect of insulin is to decrease the concentration of glucose in blood." This lowers blood sugar levels and allows the body's cells to use glucose for energy. Insulin also allows glucose to enter muscle and other tissue, works with the liver to store glucose and synthesize fatty acids, and "stimulates the uptake of amino acids," according to Bowen. Insulin is released after eating protein and especially after eating carbohydrates, which increase Lección 9. Cohesión y coherencia ¡Domínalo! Médico cirujano glucose levels in the blood. If the pancreas does not produce sufficient insulin, type 1 diabetes will develop. Unlike insulin, glucagon raises blood sugar levels. According to the Johns Hopkins University Sol Goldman Pancreatic Cancer Research Center, the combination of insulin and glucagon maintains the proper level of sugar in the blood. The pancreas' second, exocrine function is to produce and release digestive fluids. After food enters the stomach, digestive enzymes called pancreatic juice travel through several small ducts to the main pancreatic duct and then to the bile duct, according to the Medical University of South Carolina’s Digestive Disease Center. The bile duct takes the juice to the gallbladder, where it mixes with bile to aid in digestion. Location of the pancreas "The pancreas is located in the upper abdomen behind the stomach," Knowlton said. The right end of the pancreas is wide and called the head. From the head, the organ tapers to the left. The middle sections are called the neck and body, while the narrow end on the left side of the body is called the tail. The Hume-Lee Transplant Center at Virginia Commonwealth University described the pancreas as "j-shaped." The portion of the pancreas called the uncinate process bends backward from the head and underneath the body, according to the Pancreatic Cancer Action Network. Pancreas pain Intense pancreatic pain is usually associated with acute pancreatitis. It can be hard to identify pancreas pain and evaluate pancreas diseases because the organ sits deep in the abdomen, according to The National Pancreas Association. Other signs that the pain may be pancreatic include jaundice, itchy skin and unexplained weight loss. If you are experiencing pancreas pain, consult your doctor. Pancreatitis The National Institutes of Health defines pancreatitis as inflammation of the pancreas, happening when "digestive enzymes start digesting the pancreas itself." It can be acute or chronic, but both forms should be taken seriously and may lead to additional health problems. Chronic pancreatitis There are up to 23 cases of chronic pancreatitis per 100,000 people per year worldwide. In just the United States, it results in more than 122,000 outpatient visits and more than 56,000 hospitalizations per year, according to the Cleveland Clinic. "Chronic pancreatitis is a persistent inflammation (greater than three weeks) of the pancreas that causes permanent damage," Knowlton said. The condition is often caused by "heavy, ongoing" alcohol consumption, but she added that there are other causes, including "those that Lección 9. Cohesión y coherencia ¡Domínalo! Médico cirujano cause acute pancreatitis attacks." Other causes may be cystic fibrosis, high levels of calcium or fat in the blood and autoimmune disorders. Symptoms include upper abdominal pain, nausea, vomiting, weight loss, and oily stools. According to Peter Lee and Tyler Stevens, in an article for the Cleveland Clinic, "clinically apparent" oily stools (steatorrhea) do not appear until "90 percent of pancreatic function has been lost." "Chronic pancreatitis requires dietary modifications, including a low-fat diet and cessation of alcohol [intake] and smoking," Knowlton said. Chronic pancreatitis does not heal and tends to worsen with time, and "treatment options are mostly for pain relief." She added that treatments "may include a pancreas stent or, for severe cases, surgery (either a lateral pancreaticojejunostomy, or a Whipple procedure)." Pancreatiocojejunostomies are designed to decrease pancreatic leakage while the Whipple procedure removes the head of the pancreas where, according to the Mayo Clinic, most tumors occur. There may be a link between chronic pancreatitis and pancreatic cancer. According to the University of California Los Angeles Center for Pancreatic Diseases, "Recent studies reveal a 2-5 times increase in the incidence of pancreatic cancer in patients with chronic pancreatitis from a variety of causes." Acute pancreatitis "Acute pancreatitis is inflammation of the pancreas (lasting less than three weeks), that is most often caused by gallstones," said Knowlton. It usually comes on suddenly and disappears within a few days of treatment. In addition to gallstones, Knowlton said that causes "may include medications, high triglycerides, high calcium in the blood and high alcohol consumption." Pancreas pain is the chief symptom of acute pancreatitis, according to Medscape. The pain is usually severe and sudden. It increases in severity until it becomes a constant ache. This pancreas pain is felt in the upper abdomen. The Mayo Clinic noted that the pain can radiate through to the back, and Knowlton pointed out that it might be worse after eating. Other symptoms of acute pancreatitis include nausea, vomiting, fever and diarrhea. According to Knowlton, "This patient often looks acutely ill, and requires hospitalization (typically for three to five days), intravenous (IV) hydration, nothing by mouth (for bowel rest), pain medication, treatment of underlying conditions, and possibly a radiologic procedure called an endoscopic retrograde cholangiopancreatography (ERCP), which can more specifically target the problem." If the acute pancreatitis was caused by gallstones, doctors may recommend removing the gallbladder. Pancreatic cancer It is hard to diagnose pancreatic cancer early. The Mayo Clinic noted that symptoms typically don't occur until the cancer has advanced. Knowlton said, "Unfortunately, symptoms can be Lección 9. Cohesión y coherencia ¡Domínalo! Médico cirujano vague, but can include abdominal pain, jaundice, severe itching, weight-loss, nausea, vomiting, and digestive problems." Making matters even more complicated is the pancreas' deep-in-the-abdomen location. The NIH pointed out that as a result, tumors cannot usually be felt by touch. Because of the difficulty of early diagnosis and the rapidity with which pancreatic cancer spreads, the prognosis is often poor. Risk factors for pancreatic cancer include smoking, long-term diabetes and chronic pancreatitis, according to the National Cancer Institute. According to the American Cancer Society, pancreatic cancer usually begins in the cells that produce pancreatic (digestive) juices or in the cells that line the ducts. In rare occasions, pancreatic cancer will begin in the cells that produce hormones. According to the University of Texas MD Anderson Cancer Center, to diagnose pancreatic cancer, doctors typically conduct physical exams, blood tests, imaging tests, endoscopic ultrasounds and tests and biopsies. Treatment options include surgery, radiation, chemotherapy and therapies targeted to attack cancer cells without harming normal cells. Artificial pancreas When a person's pancreas isn't functioning properly or has to be removed, doctors may replace or supplement it with an artificial pancreas. These devices that automatically monitor blood glucose and provide the appropriate insulin doses are often called closed-loop systems, automated insulin delivery systems, or autonomous systems for glycemic control, according to the Food and Drug Administration. In a 2014 study published in the journal The Lancet Diabetes & Endocrinology, researchers found that an artificial pancreas offer people with type 1 diabetes a reliable way to keep glucose levels in check, when compared to other treatments. "Our study confirms that both artificial pancreas systems improve glucose control and reduce the risk of hypoglycemia compared to conventional pump therapy," study author Ahmad Haidar, of Institut de Recherches Cliniques de Montreal, said in a statement. Referencia: Szalay, J. (2018, April 12). Live Science. In Pancreas: Function, Location & Diseases. Consultado de https://www.livescience.com/44662-pancreas.html Diagrama (Puedes utilizar el sugerido o puedes incluir uno propio) Lección 9. Cohesión y coherencia ¡Domínalo! Médico cirujano Valor: 1 punto por cada respuesta correcta. Functions Pancreas Locations Disease PARTE B Valor: 4 puntos por respuesta correcta. TEXTO The nervous system is a complex collection of nerves and specialized cells known as neurons that transmit signals between different parts of the body. It is essentially the body's electrical wiring. Structurally, the nervous system has two components: the central nervous system and the peripheral nervous system. According to the National Institutes of Health, the central nervous system is made up of the brain, spinal cord and nerves. The peripheral nervous system consists of sensory neurons, ganglia (clusters of neurons) and nerves that connect to one another and to the central nervous system. Functionally, the nervous system has two main subdivisions: the somatic, or voluntary, component; and the autonomic, or Justificación Lección 9. Cohesión y coherencia ¡Domínalo! Médico cirujano involuntary, component. The autonomic nervous system regulates certain body processes, such as blood pressure and the rate of breathing, that work without conscious effort, according to Merck Manuals. The somatic system consists of nerves that connect the brain and spinal cord with muscles and sensory receptors in the skin. Description of the nervous system Nerves are cylindrical bundles of fibers that start at the brain and central cord and branch out to every other part of the body, according to the University of Michigan Medical School. Neurons send signals to other cells through thin fibers called axons, which cause chemicals known as neurotransmitters to be released at junctions called synapses, the NIH noted. There are over 100 trillion neural connections in the average human brain, though the number and location can vary. For example, a new study published January 2018 in the journal Proceedings of the National Academy of Sciences found that out of the 160 participants studied, the brains of highly creative people have more connections among three specific regions of the brain than less creative thinkers. "You have these three different systems that are all located in different parts of the brain, but they are all co-activated at once," said lead study author Roger Beaty, a postdoctoral fellow studying cognitive neuroscience at Harvard University. "People who are better able to co-activate them [came] up with more-creative responses." A synapse gives a command to the cell and the entire communication process typically takes only a fraction of a millisecond. Signals travel along an alpha motor neuron in the spinal cord 268 mph (431 km/h); the fastest transmission in the human body, according to Discover magazine. Sensory neurons react to physical stimuli such as light, sound and touch and send feedback to the central nervous system about the Lección 9. Cohesión y coherencia ¡Domínalo! Médico cirujano body's surrounding environment, according to the American Psychological Association. Motor neurons, located in the central nervous system or in peripheral ganglia, transmit signals to activate the muscles or glands. [Here's What You'd Look Like as Just a Nervous System] Glial cells, derived from the Greek word for "glue," are specialized cells that support, protect or nourish nerve cells, according to the Oregon Institute of Health and Science University. The brain's connections and thinking ability grew over thousands of years of evolution. For example, a virus bound its genetic code to the genome of four-limbed animals, and the code can still be found in humans' brains today, according to two papers published in the January 2018 journal Cell. This code packages up genetic information and sends it from nerve cells to other nearby nerve cells, a very important process in the brain. The human brain is the command center for the human nervous system. The human brain receives signals from the body's sensory organs and outputs information to the muscles and body. The human brain has the same basic structure as other mammal brains but is larger and amazing in relation to body size than any other brains when it receives several commands. Numbers about the human brain The human brain is the largest brain of all vertebrates relative to body size. It weighs about 3.3 lbs. (1.5 kilograms). The average male has a brain volume of 1,274 cubic centimeters (cm3). The average female brain has a volume of 1,131 cm3. The brain makes up about 2 percent of a human's body weight. The cerebrum makes up 85 percent of the brain's weight. It contains about 86 billion nerve cells (neurons) — the "gray matter." It contains billions of nerve fibers Lección 9. Cohesión y coherencia ¡Domínalo! Médico cirujano (axons and dendrites) — the "white matter." These neurons are connected by trillions of connections, or synapses. The largest part of the human brain is the cerebrum, which is divided into hemispheres, according to the Mayfield Clinic. Underneath lies the brainstem, and behind that sits the cerebellum. The outermost layer of the cerebrum is the cerebral cortex, which consists of four lobes. Like all vertebrate brains, the human brain develops from three sections known as the forebrain, midbrain and hindbrain. Each of these contains fluid-filled cavities called ventricles. The forebrain develops into the cerebrum and underlying structures; the midbrain becomes part of the brainstem; and the hindbrain gives rise to regions of the brainstem and the cerebellum. Introduction Around one billion adults worldwide smoke,1 with high prevalence in developing countries, where 49% of men and 11% of women use tobacco.2 Although the prevalence of current smokers has decreased over time in several countries, the global absolute number of smokers has increased owing to population growth.3 Policies have successfully encouraged people to quit, using aids such as nicotine replacement therapy and electronic cigarettes (e-cigarettes). In the Health Survey for England (2013 and 2014), 26% of current smokers reported that they wanted to cut consumption down but were not trying to stop, and 40-41% said that they smoked less than in the previous year.5 The percentage of smokers who consume one to five cigarettes per day has steadily risen (from 18.2% to 23.6% between 2009 and 20145), with a similar pattern in the US, where the proportion of smokers who consume less than 10 cigarettes per day increased from 16% to 27% between 2005 and 2014.6 A recent Cochrane review discussed the evidence for ways of helping smokers who wish to reduce their consumption. Lección 9. Cohesión y coherencia ¡Domínalo! Médico cirujano Smoking few cigarettes is generally believed to be relatively safe, as has been incorrectly assumed for light/low nicotine cigarettes.8 Among 24 658 US adolescents, 10% thought that light smoking was not harmful, and only 35% of light smokers considered their habits to be associated with “a lot of harm.”9 Reducing consumption might be expected to reduce harm in a proportionate way—that is, that smoking one instead of 20 cigarettes per day has about one twentieth (5%) of the risk. This seems to be the case for lung cancer, for which the large American Cancer Society Prevention Study II showed an approximately linear relation between risk of lung cancer and number of cigarettes smoked per day, but the dose-response for cardiovascular disease is steep at low consumption and then levels off,10 consistent with the shape reported previously. In a seminal systematic review of secondhand smoke and coronary heart disease among never smokers published in the BMJ 20 years ago, Law and colleagues drew attention to the 1.30 risk ratio being relatively large compared with the 2-3 typically seen in studies of active smokers.12 Their conclusions on second-hand smoke were supported by a meta-analysis of active cigarette smoking and risk of coronary heart disease from five cohort studies, in which the modelled relative risk for smoking one cigarette per day (1.39) was consistent with that for exposure to secondhand smoke. Although the non-linear relation between coronary heart disease and low cigarette consumption has been reported before (individual studies, as well as official reports from the US Surgeon General), it still is still not commonly known by the general public or health professionals, particularly those not involved in tobacco and health. We thus aimed to extend the previous work on coronary heart disease,12 by using a systematic review to provide a major body of evidence. We also aimed to show that a similar non-linear relation exists between Lección 9. Cohesión y coherencia ¡Domínalo! Médico cirujano stroke and low cigarette consumption. PARTE C Valor: 1 punto cada una. TEXTO Texto 1 Texto 2 Texto 3 IDEA PRINCIPAL When you finish, name your file as: T9_LASTNAME_NAME .