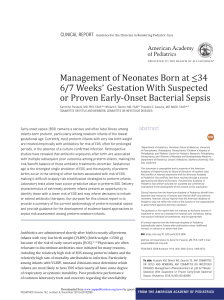
https://doi.org/10.5664/jcsm.9264 S C I E N T I F I C I N V E S T I G AT I O N S Polysomnography use in complex term and preterm infants to facilitate evaluation and management in the neonatal intensive care unit James Kim, MD1; Seyni Gueye-Ndiaye, MD2; Elizabeth Mauer, MSc3; Vikash K. Modi, MD4; Jeffrey Perlman, MBChB1; Haviva Veler, MD2 1 Division of Newborn Medicine, New York-Presbyterian Hospital–Weill Cornell Medical Center, Komansky Children’s Hospital, New York, New York; 2Pediatric Pulmonology, New YorkPresbyterian Hospital–Weill Cornell Medical Center, Komansky Children’s Hospital, New York, New York; 3Division of Biostatistics and Epidemiology, Weill Cornell Medicine, New York, New York; 4Department of Otolaryngology, Division of Pediatric Otolaryngology–Head & Neck Surgery, New York-Presbyterian Hospital–Weill Cornell Medical Center, New York, New York Study Objectives: (1) To determine the characteristics of term and preterm infants for whom polysomnography (PSG) was used as a primary diagnostic tool in infants with recurrent desaturation episodes, suspected obstructive apnea, or both, and the prevalence of abnormal studies. (2) To identify the interventions following PSGs. (3) To assess the added value of airway and swallow evaluations. Methods: Retrospective cohort study of infants evaluated by PSG in the Neonatal Intensive Care Unit at New York-Presbyterian Hospital–Weill Cornell from January 2012 to April 2018. Results: PSGs were performed on 31 infants; 15 (48%) term and 16 (52%) preterm infants. Indications for PSG were persistent desaturations (n = 24), suspected obstructive apnea (n = 15), and stridor (n = 2). Primary comorbid conditions were respiratory (n = 11), craniofacial (n = 9), airway anomalies (n = 6), and neurologic (n = 5). The apnea-hypopnea index was abnormal in 30 (97%) infants. Of those, 23 (74%) were severe, 7 (23%) were moderate, and 1 was normal (3%). Apneic events were predominantly obstructive in 23 infants and predominantly central in 6. The apnea-hypopnea index improved in all but 1 follow-up PSG. The PSG findings resulted in interventions in 24 (77%) infants, in addition to concomitant otolaryngology evaluations (abnormal in 20/25) and swallow studies (abnormal in 9/14). Clinical signs completely resolved in 22 (71%) infants. Conclusions: This is one of the first reports on the diagnostic value of inpatient PSGs in the neonatal intensive care unit in infants with recurrent desaturation episodes, suspected obstructive apnea, or both. Our findings indicate that PSG is an important tool in evaluating and targeting therapies in complex term and preterm infants with a wide variety of comorbidities. Keywords: polysomnography, neonate, neonatal intensive care unit, sleep-disordered breathing, sleep apnea syndromes Citation: Kim J, Gueye-Ndiaye S, Mauer E, Modi VK, Perlman J, Veler H. Polysomnography use in complex term and preterm infants to facilitate evaluation and management in the neonatal intensive care unit. J Clin Sleep Med. 2021;17(8):1653–1663 . BRIEF SUMMARY Current Knowledge/Study Rationale: There are limited studies evaluating the use of polysomnography as a diagnostic tool in the inpatient neonatal population with recurrent desaturation episodes, suspected obstructive apnea, or both. The objective was to determine the population of term and preterm infants for whom polysomnography was used as a primary diagnostic tool in the neonatal intensive care unit. Study Impact: In this retrospective cohort study the use of inpatient polysomnography in infants with recurrent desaturations, suspected obstructive sleep apnea, and stridor was found to lead to positive findings in 97% of cases with change in management plan for most infants. Inpatient polysomnography in the neonatal intensive care unit is an important tool in evaluation and targeting of therapies in complex term and preterm infants. children.1,2 In term infants, apnea and intermittent hypoxemia can result from significant craniofacial anomalies, such as Pierre Robin sequence and micrognathia, 3,4 or from neurologic disease, particularly in those associated with neuromuscular weakness.5–7 Polysomnography (PSG) is a multichannel test used as a diagnostic tool in sleep-related breathing disorders. Indications and utility for inpatient PSG (IPPSG) in complex term infants and preterm infants in the neonatal intensive care unit (NICU) are not well described. To our knowledge, 5 studies have described the use of PSG as a diagnostic tool in the inpatient INTRODUCTION Certain neonatal populations have been shown to be at an increased risk of sleep-related breathing disorders. In preterm infants, the etiology of recurrent apnea, bradycardia, and desaturation events that persist beyond expected resolution is often multifactorial, caused by central, obstructive, and mixed apneas. Immature respiratory control resulting in respiratory pauses, ineffective, and/or obstructed inspiratory efforts, as well as feeding-related respiratory abnormalities are the major precipitants of apnea and intermittent hypoxemia events in these Journal of Clinical Sleep Medicine, Vol. 17, No. 8 1653 August 1, 2021 J Kim, S Gueye-Ndiaye, E Mauer, et al. Polysomnography use in complex term and preterm infants pediatric population, 3 in children ages 1 month to 6.5 years8–10 and 2 in infants in the NICU. One study evaluated infants admitted due to concern for seizures11 and another in infants with myelomeningoceles.12 To further assess the diagnostic potential and benefits of IPPSG in the NICU, we retrospectively reviewed IPPSGs performed in a single tertiary neonatal care center in infants with recurrent desaturation episodes, suspected obstructive apnea, or both. The goals of this study were to describe the use of IPPSG in the NICU by: (1) characterizing the population of term and preterm infants for whom PSG was used as a primary diagnostic tool, (2) determining the indications for IPPSG, (3) identifying the incidence of abnormal PSGs in a selected population of infants with suspected obstructive or central apnea, (4) identifying the associated interventions following PSG, and (5) describing the added value of airway evaluations and swallow studies in establishing a diagnosis and guiding treatment. was based on accepted American Academy of Sleep Medicine criteria. Apnea was scored when peak signal airflow excursions dropped by ≥ 90% of pre-event baseline, and the event met duration and respiratory effort criteria for an obstructive, mixed, or central apnea. Obstructive apnea was scored in apnea that occurred for at least the duration of 2 breaths during baseline breathing in the presence of respiratory effort throughout the entire period of absent airflow. Central apnea was scored when there was an absence of inspiratory effort throughout the event, and at least 1 of the following was met: (1) ≥ 20 seconds in duration, (2) duration of at least 2 breaths during baseline breathing associated with an arousal or ≥ 3% oxygen desaturation, (3) association with a decrease in heart rate to less than 50 beats per minute for at least 5 seconds or less than 60 beats per minute for 15 seconds. Mixed apnea was scored when an apnea occurred for at least the duration of 2 breaths during baseline breathing and was associated with absent respiratory effort during 1 portion of the event and the presence of inspiratory effort in another portion. Hypopnea was scored when: (1) the peak nasal pressure excursions decreased by ≥ 30% of pre-event baselines, (2) the duration of the ≥ 30% drop lasted for at least 2 breaths, and (3) there was a ≥ 3% desaturation from pre-event baseline or associated arousal. AHI was determined as the total number of apneas and hypopneas divided by the total hours of sleep.13 The severity of total AHI in newborns is not well defined, therefore we elected to use pediatric criteria with a total AHI categorized as mild when AHI was between 1 and 4.9 events/h, moderate when AHI was 5–9.9 events/h, and severe when AHI was ≥ 10 events/h.14 The severity of obstructive sleep apnea (OSA) was categorized according to Katz et al.15 OSA is typically characterized as mild when obstructive AHI is between 1 and 4.9 events/h; SpO2 < 90% for 2% to 5% of the night, moderate when AHI is 5–9.9 events/h; SpO2 < 90% for 5% to 10% of the night, and severe when AHI ≥ 10 events/h; SpO2 < 90% for > 10% of the night. According to the aforementioned American Academy of Sleep Medicine guidelines, “central apnea is defined as lack of flow and effort for the length of 2 breaths.” In infants who breath 40 times per minute (or even faster in the premature infant), the length of the event can be very short, such as 1–2 seconds per event, making it difficult to detect and score. Studies have shown that the median value for central AHI (cAHI) in normal infants ≤ 1 month of age is 5 events/h with the 95th percentile ranging from 17.8–45 events/h.16,17 Central sleep apnea (CSA) was defined in a symptomatic infant with a predominant central component on PSG and cAHI > 10 events/h. Additional PSG parameters included oxygen saturation baseline and nadir, time with oxygen saturation < 92%, oxygen desaturation index defined as the number of ≥ 3% arterial oxygen desaturations per hour of sleep, EtCO2 at baseline, maximum value and time with EtCO2 > 50 mm Hg. Sleep parameters for PSGs included total sleep time, arousals index, and sleep efficiency. Recurrent desaturations in preterm infants were defined as those with a clinical diagnosis of apnea of prematurity with desaturations that persisted beyond expected resolution (40 weeks postmenstrual age). In term infants, recurrent desaturations were associated with a suspected obstructive process. METHODS This was a retrospective cohort study of all infants who underwent IPPSG from January 2012 to April 2018 in the NICU at New York Presbyterian–Weill Cornell Medical College, Komansky Children’s Hospital. The data collected included infant demographics, indications for IPPSG, comorbid conditions, IPPSG findings, associated interventions, and concomitant studies. The decision to perform a sleep study was determined by the attending neonatologist in consultation with a pulmonologist and otolaryngologist. All IPPSGs were conducted in the NICU at the infant’s bedside, either in a single room or a quiet section. This study was approved by the Weill Cornell Medicine institutional review board. IPPSG was performed by a mobile unit (Natus Sleepworks; Natus Medical Incorporated, San Carlos, CA), attended by a registered polysomnographic technologist, and included continuous recording of the central, occipital, and frontal electroencephalogram (EEG) derivations, electro-occulograms (EOGs), chin electromyogram (EMG), modified lead II electrocardiogram (ECG), nasal oral thermistor, nasal pressure (Salter Labs, El Paso, TX), pulse oximetry (Masimo oximetry; Irvine, CA), end-tidal CO2 (EtCO2; Capnocheck Sleep Capnograph/Oximeter, Smith Medical, Minneapolis, MN; cannula: Salter Labs), and/or transcutaneous CO2 (SenTec AG, Therwil, Switzerland), and thoracic and abdominal respiratory inductance plethysmography (Dymedix Diagnostics, Shoreview, MN). The patient was observed with a low-light-level video camera (Model ZBN-20Z27F; CNB Technology, Buena Park, CA), and snoring microphone (Sleepmate; Ambu Inc., Columbia, MD). PSG analysis was done during times of “sleep” and excluded “wake” times, such as during feedings and nursing cares. The study was scored using the American Academy of Sleep Medicine recommended rules by a registered polysomnographic technologist, with the entire study reviewed and interpreted by a board certified sleep physician (H.V.).13 Scoring of obstructive, central, and mixed apneas and hypopneas Journal of Clinical Sleep Medicine, Vol. 17, No. 8 1654 August 1, 2021 J Kim, S Gueye-Ndiaye, E Mauer, et al. Polysomnography use in complex term and preterm infants PSG findings Otolaryngology evaluations were done in conjunction with IPPSG to rule out airway anomalies in infants with respiratory comorbidities and also as part of the diagnostic work-up in infants with craniofacial and airway anomalies. Ear, nose, and throat (ENT) evaluation included awake bedside laryngoscopy and, when inconclusive, continued to drug-induced sleep endoscopy (DISE) and/or direct laryngoscopy and bronchoscopy. Swallow studies were performed when there was a suspicion that laryngeal chemoreflex due to feeding issues or acid reflux could be contributing to desaturation events. Swallow studies were performed by the pediatric radiologist and pediatric speech pathologist using varying consistencies of barium. On initial IPPSGs (n = 31), the total AHI was severe in 23 (74%) infants, moderate in 7 (23%), no mild cases, and normal in 1 infant (3%). When broken down into the obstructive and central components, obstructive AHI (oAHI) was severe in 18 (58%) infants, moderate in 6 (19%), and mild in 5 (16%). Ten (32%) infants had CSA with a cAHI > 10 events/h (presumed high in patient no. 28, as data was missing for cAHI/oAHI on the initial study). Comparing preterm and term infants, total AHI was severe in 12 (75%) preterm and 11 (73%) term infants, AHI was moderate in 4 (25%) preterm and 3 (20%) term infants, there were 0 mild AHI patients in both groups, and 1 term infant had a normal study with no respiratory abnormalities detected. Category of AHI by comorbid condition is demonstrated in Figure 1. The total AHIs in the initial studies differed when comparing primary comorbid conditions. The median total AHI was 50 events/h in craniofacial and airway anomalies combined, 44.3 events/h in neurologic comorbid conditions, and 11.1 events/h in respiratory comorbid conditions (P = .02). There was also a difference in oAHI but not in cAHI comparing primary comorbid conditions (Table 3). Oxygen nadir showed a trend toward lower values in the craniofacial/airway anomaly and neurologic group compared to respiratory group (P = .09). A predominant obstructive component (oAHI) on PSG was seen in 23 (74%), and a predominant central component (cAHI) was seen in 6 (19%) infants. One (3%) infant had an equal oAHI and cAHI, and 1 infant had a normal study. Within those with a predominant oAHI, the primary associated comorbidity was craniofacial in 9 (39%) with 5 of these cases being in term infants (Table 1 and Table 2). In contrast, in those with a predominant cAHI, the primary associated comorbidity was respiratory in 4 (67%) infants, all of them preterm (Table 1 and Table 2). Sleep parameters for PSGs included on average: total sleep time 323.8 minutes, arousals index 52.2 arousals/h and sleep efficiency 67%. Additional study results on initial PSGs included average of oxygen saturation baseline: 96.1% (range 92.2% to 99.9%), oxygen saturation nadir: 73.6% (range 33.3% to 92.1%), time with oxygen saturation < 92%: 48.6 min (range 0.1–289.2 min); 29 infants started the study on room air, with 9 of those titrating to O2 via nasal cannula or HFNC, and 2 were on HFNC during the entire study. Oxygen desaturation index: 45.6 desaturations/h (range 2–156.7 desaturations/h), baseline EtCO2: 34.9 mm Hg (range 23.8–49.8 mm Hg), max EtCO2: 49.4 mm Hg (range 35–64.9 mm Hg), and time with EtCO2 > 50 mm Hg: 23 min (range 0–251.6 min). Statistical analysis Patient demographic and clinical characteristics along with PSG results, interventions, and follow-up results were described as N (%) or mean, median, and range. AHI severity groups were compared across diagnosis groups by chi-square/Fisher’s exact tests. For patients with follow-up PSGs after intervention, initial AHIs were compared to final AHIs by paired t tests. All analyses were 2-sided with statistical significance evaluated at the 0.05 alpha level. Analyses were performed in R version 3.5.3. (R Foundation for Statistical Computing, Vienna, Austria).18 RESULTS Patient demographics During the study period 48 IPPSGs were done on 31 infants; 15 (48%) were term and 16 (52%) preterm. There were 14 females. In preterm infants the gestational age at birth ranged from 24-2/7 to 36-6/7 weeks. The mean postmenstrual age (PMA) at time of first PSG was 41-3/7 weeks (median 40-4/7 weeks, range 36-6/7 to 51-1/7 weeks). Seven infants with a clinical diagnosis of apnea of prematurity and recurrent desaturation events had a mean PMA of 41-6/7 wk. In term infants the average age of the first PSG was 16.3 days (median 15 days, range 3–33 days). There were 3 main clinical indications for IPPSG, with the most common being recurrent desaturations (n = 24), followed by suspected obstructive apnea (n = 15) and stridor (n = 2). Ten patients had multiple indications (Table 1 and Table 2). The primary comorbid conditions of those infants undergoing PSG were respiratory in 11, craniofacial anomalies in 9, upper airway anomalies in 5, lower airway anomaly in 1, and neurologic in 5 infants (Table 1 and Table 2). Term infants had a majority of craniofacial anomalies, 6/15 (40%) (all 6 had micrognathia). Preterm infants had a majority of respiratory conditions, 10/16 (63%), with 7 out of 10 having a clinical diagnosis of apnea of prematurity. Three preterm infants with a diagnosis of chronic lung disease had PSG done to rule out a suspected obstructive apnea, 2 with persistent high-flow nasal cannula (HFNC) requirements and 1 with a persistent O2 via nasal cannula requirement. Three patients had confirmed genetic syndromes, including trisomy 21 with hypopharyngeal collapse and glossoptosis, congenital disorder of glycosylation type 1 with central nervous system abnormality and hypotonia, and RAPADILINO syndrome with micrognathia. Journal of Clinical Sleep Medicine, Vol. 17, No. 8 Treatment Following PSG, treatment interventions were implemented in 24 (77%) infants. For patients with a predominant obstructive component (oAHI) on PSG, mandibular distraction (n = 7), continuous positive airway pressure (CPAP)/HFNC (n = 4) and tracheostomy (n = 4) were the most common interventions. In patients with a predominant central component (cAHI), the most common intervention was caffeine (n = 4). In infants with a clinical diagnosis of apnea of prematurity, 3 infants had a predominant cAHI for which 2 were treated with caffeine and 1 had self-resolution of apnea. Four infants had a predominant oAHI for which 2 were treated with O2 via nasal cannula, 1 was 1655 August 1, 2021 J Kim, S Gueye-Ndiaye, E Mauer, et al. Polysomnography use in complex term and preterm infants Table 1—Indication, diagnosis, and results of polysomnography in term infants. ID No. 1 2 Primary O2 Total Comorbid Indication Diagnosis cAHI oAHI Sat Treatment AHI Condition Nadir Neurologic Recurrent Hypotonia of 65.8 48.7 17.1 76 O2 via NC desaturations unknown etiology 63.5 Caffeine No 25.8 38.6 13.4 9.4 12.4 29.2 63 O2 via NC 55.8 CPAP/ HFNC/DNR Yes No 16 1.7 14.1 81.7 Tracheostomy Yes 5.2 0 5.2 89 Yes 3 5.5 0.3 2.6 2.6 2.9 95 92.1 Mandibular distraction (further distraction) 1.4 8.7 0.2 0.2 1.2 8.5 94 78.7 Mandibular distraction Yes 100.1 Recurrent desaturations/ Micrognathia/ Craniofacial 21.6 Pierre suspected anomaly Robin sequence obstructive apnea 1.5 142.2 Recurrent desaturations/ Micrognathia/ Craniofacial 6.8 Pierre Suspected anomaly Robin sequence obstructive apnea 3.3 1.4 97.9 34 Yes Recurrent Seizures desaturations and hypotonia Recurrent Hypotonia/ desaturations congenital disorder of glycosylation type 1/glossoptosis 4 Neurologic Recurrent Hypotonia of desaturations unknown etiology 7 8 9 FT with history of fetal-maternal hemorrhage and seizures. Brain MRI with white matter changes predominately on left with minimal changes in basal ganglia and internal capsule. Follow-up study FT with congenital disorder of glycosylation type and multiple congenital anomalies. Brain MRI with marked diffuse volume loss including brainstem, cerebellar hypoplasia, thin corpus callosum, ventricular enlargement. ENT evaluation revealed pooling of secretions and glossoptosis. FT with hypotonia of unclear etiology requiring tracheostomy and g-tube. ENTevaluation revealed edematous epiglottis/arytenoids, general upper airway collapse due to poor tone. Brain MRI with hypoplastic corpus callosum with abnormal white matter. FT with micrognathia (Pierre Robin sequence) requiring intubation and mechanical ventilation. Mandibular distraction performed prior to initial PSG. On RA at time of PSG. Follow-up study FT with micrognathia (Pierre Robin sequence) requiring intubation and mechanical ventilation. Mandibular distraction performed prior to initial PSG. On RA at time of PSG. Follow-up study FT with micrognathia (Pierre Robin sequence) 15 Neurologic 6 FT with hypotonia of unclear etiology. Brain MRI normal. 28 Neurologic Suspected Craniofacial obstructive anomaly apnea Suspected Craniofacial obstructive anomaly apnea Micrognathia/ Pierre Robin sequence Micrognathia/ Pierre Robin sequence Micrognathia/ Craniofacial Recurrent anomaly desaturations/ Pierre Robin sequence suspected obstructive apnea Journal of Clinical Sleep Medicine, Vol. 17, No. 8 Mandibular distraction (further distraction) Mandibular distraction 8.3 13 81.5 Further distraction 0 1.5 89 0.2 141.8 69 Mandibular distraction 0 6.8 90 Further distraction 0 3.3 92 (continued on following page) 1656 Description Yes 44.3 3 5 Symptoms Resolved Yes Yes FT with micrognathia (Pierre Robin sequence) Follow-up study no. 1 Follow-up study no. 2 FT with micrognathia (Pierre Robin sequence) Follow-up study no. 1 Follow-up study no. 2 August 1, 2021 J Kim, S Gueye-Ndiaye, E Mauer, et al. Polysomnography use in complex term and preterm infants Table 1—Indication, diagnosis, and results of polysomnography in term infants. (continued) ID No. 10 11 12 13 14 15 Primary Comorbid Condition Indication Diagnosis Recurrent desaturations/ Micrognathia/ Craniofacial glossoptosis/ suspected anomaly hypotonia obstructive apnea Upper airway anomaly Upper airway anomaly Upper airway anomaly Recurrent desaturations/ Hypopharyngeal collapse/ suspected glossoptosis obstructive apnea Recurrent desaturations/ suspected obstructive apnea Choanal atresia/ epiglottis with intermittent retroflexion/ tracheal sleeve Total cAHI oAHI AHI O2 Sat Treatment Nadir 73 Mandibular distraction Symptoms Resolved Yes 20.4 1.6 18 6.3 1.6 4.7 5.6 36.5 3.7 12 1.6 25 90.1 Further distraction 83.4 66.4 CPAP 154.4 41.2 120 17 35 23 73.2 HFNC 80.9 No 95.6 20.3 69.6 69.4 Tracheostomy Yes FT infant with choanal atresia. ENT evaluation revealed epiglottis with intermittent retroflexion and tracheal sleeve. 50 2.5 47 78.5 Supraglottoplasty No 21.4 95.6 10 20.3 11 69.3 No Yes 1.4 0.8 0.6 78.2 69.4 HFNC then tracheostomy 87.4 None FT with stridor and desaturation with feeds. ENT evaluation revealed laryngomalacia with prolapse of arytenoid mucosa. Supraglottoplasty done with continued stridor at rest. Follow-up study FT infant with recurrent desaturations. ENT evaluation revealed tracheal sleeve. FT infant with recurrent desaturations and bradycardic events associated with apnea and feeding. Symptoms were self-resolving. No Recurrent desaturations/ Laryngomalacia stridor Recurrent Tracheal sleeve Lower desaturations airway anomaly Respiratory Recurrent Apnea desaturations of newborn Description Yes FT infant with multiple congenital anomalies including micrognathia, hypotonia, facial palsy, club feet. ENT evaluation revealed glossoptosis, arytenoid and vocal cord edema. Follow-up study no. 1 Follow-up study no. 2 FT infant with trisomy 21. ENT evaluation revealed hypopharyngeal collapse and glossoptosis. Worsening cAHI in follow-up study no. 1 thought to be from CPAP-induced central apnea. Follow-up study no. 1 Follow-up study no. 2 Bold numbers represent the predominant component of AHI. AHI = apnea-hypopnea index, cAHI = central AHI, CPAP = continuous positive airway pressure, DNR = do no resuscitate, ENT =ear, nose, and throat, FT = full term, HFNC = high-flow nasal cannula, MRI = magnetic resonance imaging, NC = nasal cannula, oAHI = obstructive AHI, PSG = polysomnography, RA = room air, Sat = saturation. treated with HFNC, and 1 was suspected to have gastroesophageal reflux disease, based on the pattern of OSA correlating closely with clinical symptoms, which was treated with a protonpump inhibitor and hydrolyzed formula. There were 7 infants who did not have interventions; 3 self-resolved, 1 had a normal study, 1 infant was recommended intervention but family decided on comfort care with Do Not Resuscitate/Do No Intubate, and 2 infants improved clinically with interventions implemented prior to PSG. Clinical signs completely resolved in 22 (71%) infants; 2 of these patients did not require a change in management (Table 1 and Table 2). treatment with caffeine, 1 with laryngomalacia following supraglottoplasty, 1 with hypopharyngeal collapse following CPAP/HFNC titration, and 1 with micrognathia/glossoptosis following tongue-lip adhesion. For those with a predominant oAHI, the mean time to follow-up PSG was 11.5 days (range 2– 31 days), and for those with a predominant cAHI, the mean time to follow-up PSG was 11.2 days (range 8–15 days). The total AHI was severe in 7 (41%), moderate in 4 (24%), and mild in 6 (35%) infants. Improvement in AHI was observed in all final follow-up PSGs except 1 (patient no. 11). In 9 infants with a predominant oAHI, the mean total AHI improved from 64.34 events/h to 11.48 events/h in the final follow-up PSGs (mean of differences, 52.8, 95% CI 10.1–95.7, P = .02). In 4 infants with a predominant cAHI, the mean total AHI improved from 32.88 Follow-up studies There were 17 follow-up studies done on 13 out of 31 patients, 6 with micrognathia following mandibular distraction, 4 following Journal of Clinical Sleep Medicine, Vol. 17, No. 8 1657 August 1, 2021 J Kim, S Gueye-Ndiaye, E Mauer, et al. Polysomnography use in complex term and preterm infants Table 2—Indication, diagnosis, and result of polysomnography in preterm infants. ID No. 16 17 18 19 20 21 Primary O2 Total Comorbid Indication Diagnosis cAHI oAHI Sat Treatment AHI Condition Nadir Hypoxic 113.9 6.1 87.3 67.8 None Neurologic Recurrent (tracheostomy desaturations/ ischemic encephalopathy recommended, suspected declined for obstructive comfort care) apnea ex-33 week infant, 39 weeks corrected, hypoxic ischemic encephalopathy at birth. ENT evaluation reveled pooling of secretions with aspiration. Brain MRI consistent with HIE. ex-32 week infant, 42 weeks corrected, with VACTERL syndrome, micrognathia, cleft palate and glossoptosis (Pierre Robin sequence), diagnosed with RAPADILINO syndrome. ex-36 week infant with micrognathia and cleft palate (Pierre Robin sequence). Follow-up Study ex-35 week infant, with micrognathia and cleft palate. ENT evaluation revealed glossoptosis. Follow-up study 11.9 RAPADILINO syndrome with micrognathia/ Pierre Robin sequence 1.9 10 89.1 None No Suspected Craniofacial obstructive anomaly apnea Micrognathia/ Pierre Robin sequence 75.2 1.3 74.2 65.6 Mandibular distraction Yes 2.9 144 0 67 2.9 76 Micrognathia/ Pierre Robin sequence 91.5 80.6 Tonguelip adhesion 23 6.4 8.9 85 Laryngomalacia 25.2 11 14 59.7 No change No Soft palate collapse/ glossoptosis 72.2 2.3 64.6 33.3 Tracheostomy Yes Apnea of prematurity 6.7 1.1 4.5 89.9 O2 via NC Yes Recurrent Apnea desaturations of prematurity 7.6 1.3 6.3 89 HFNC Yes 31.4 24 7.3 63 Caffeine No 13.4 12.6 0.9 Yes Yes Recurrent desaturations/ Craniofacial suspected anomaly obstructive apnea Recurrent Upper desaturations/ airway stridor anomaly Upper Recurrent airway desaturations anomaly Respiratory Recurrent desaturations 23 Respiratory Respiratory Recurrent desaturations Yes Apnea of prematurity 25 Respiratory Recurrent desaturations Apnea of prematurity 11.9 9 2.5 77.8 Caffeine dose increased 80.5 None 26 Respiratory Recurrent desaturations Apnea of prematurity 8 2 6 82 Prevacid/ Alimentum Description No Craniofacial Suspected anomaly obstructive apnea 22 24 Symptoms Resolved Yes ex-35 week infant, already on HFNC prior to PSG with symptoms improving over time. ex-25 week infant, 40 weeks corrected with recurrent desaturation episodes requiring HFNC. ENT evaluation revealed soft palate collapse and glossoptosis. ex-31 week infant, 46 weeks corrected, with recurrent desaturation and bradycardic events associated with apnea of prematurity. ex-30 week infant, 44 weeks corrected, with recurrent desaturation and bradycardic events associated with apnea of prematurity. ex-29 wk infant, 39 weeks corrected, with recurrent desaturation and bradycardic events associated with apnea of prematurity. Follow-up study ex-29 6/7 week infant, 40 weeks corrected, with recurrent desaturation and bradycardic events associated with apnea of prematurity. ex-27 week infant, 43 weeks corrected, with recurrent desaturations and bradycardic events associated with apnea of prematurity. Results of PSG interpretation, not classically OSA, occurring with movements possibly related to GERD contributing to apneic events. (continued on following page) Journal of Clinical Sleep Medicine, Vol. 17, No. 8 1658 August 1, 2021 J Kim, S Gueye-Ndiaye, E Mauer, et al. Polysomnography use in complex term and preterm infants Table 2—Indication, diagnosis, and result of polysomnography in preterm infants. (continued) ID No. 27 28 29 Primary Comorbid Indication Condition Respiratory Recurrent desaturations Respiratory Recurrent desaturations Suspected Respiratory obstructive apnea Diagnosis Apnea of prematurity/ feeding immaturity 6.7 1.1 4.5 O2 Sat Treatment Nadir 89.9 No change 39.8 - - 72.6 Caffeine Yes 7.1 16 6.5 13.9 0.6 2 79.1 73.3 Caffeine Yes Total cAHI oAHI AHI Symptoms Resolved Yes Apnea of prematurity/ feeding immaturity Chronic lung disease 4.2 3.8 0.4 91.2 30 Respiratory Suspected obstructive apnea 28.5 Chronic lung disease/ bronchomalacia/ CPAM 0 28.5 85 31 Respiratory Suspected obstructive apnea Chronic lung disease/ pulmonary hypertension 11.1 5 5 77.4 No change Tracheostomy No No Description ex-31 week infant, 41 weeks corrected with recurrent desaturations and bradycardic events associated with apnea of prematurity and feeding immaturity. MBS showed aspiration, thickening of feeds did not resolve events. O2 via NC started prior to PSG, with PSG confirming improvement in events with NC. ex-32 wk, 40 weeks corrected, with recurrent desaturations and bradycardic events associated with apnea of prematurity and feeding immaturity. Discharged home on caffeine. Follow-up study ex-33 week infant, 42 weeks corrected, with persistent tachypnea on O2 via NC. Follow-up study ex-33 week infant, 45 weeks corrected with VACTERL syndrome, CPAM, congenital hypothyroidism and persistent tachypnea requiring HFNC. ENT evaluation revealed soft palate cleft, edema of arytenoids and bronchomalacia. ex-24wk infant, 2 months corrected, with severe chronic lung disease, pulmonary hypertension and hypercarbia requiring persistent HFNC. Bold numbers represent the predominant component of AHI. AHI = apnea-hypopnea index, cAHI = central AHI, CPAM = congenital pulmonary airway malformation, ENT = ear, nose, and throat, GERD = gastroesophageal reflux disease, HFNC = high-flow nasal cannula, HIE = hypoxic ischemic encephalopathy, MBS = modified barium swallow, NC = nasal cannula, oAHI = obstructive AHI, OSA = obstructive sleep apnea, PSG = polysomnography; RAPADILINO = radial malformations, patella and palate abnormalities, diarrhea, dislocated joints, limb abnormalities, little size long, slender nose and normal intelligence; VACTERL = vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, renal anomalies, and limb abnormalities. Figure 1—AHI severity by diagnosis. events/h to 12.62 events/h in the follow-up PSGs (mean of differences 20.25, 95% CI 6.18–34.32, P = .02). For all 13 infants with a follow-up study, the mean AHI improved from 54.7 events/h to 11.8 events/h in follow-up PSGs (mean of differences 42.8, 95% CI 13.6–72.0, P = .007) (Figure 2), the mean oAHI improved from 42.7 to 5.4 (mean of differences 36.9, 95% CI 7.6–66.1 P = .018), and the mean cAHI changed from 12.9 to 5.7 (mean of differences 7.3, 95% CI –4.2 to 18.7, P = .19). Additional supportive studies Concomitant studies, in patients with abnormal PSGs, included ENT evaluations and barium swallow studies. ENT evaluations (n = 25), including fiberoptic flexible laryngoscopies, DISE and/ or direct laryngoscopy and bronchoscopy, revealed 20 abnormal evaluations (Table 1 and Table 2). Swallow studies were completed on 14 infants, 9 showing aspiration of varying Journal of Clinical Sleep Medicine, Vol. 17, No. 8 AHI = apnea-hypopnea index. degrees (5 term and 4 preterm infants). This included aspiration with thin liquids (n = 5), puree thick consistency (n = 1), and all 1659 August 1, 2021 J Kim, S Gueye-Ndiaye, E Mauer, et al. Polysomnography use in complex term and preterm infants Table 3—AHI and O2 nadir in primary comorbid conditions. AHI cAHI Primary Respiratory (n = 11) 11.1 [7.2; 22.2] 1.7 [1.1; 10.2] Craniofacial and Airway Anomalies (n = 15) 50.0 [16.1; 95.6] 2.3 [1.4; 11.5] Primary Neurologic (n = 5) 44.3 [38.6; 65.8] 9.4 [6.1; 28.0] P Overall .02 .21 oAHI O2 nadir 4.8 [3.0; 6.2] 82.0 [75.3; 88.2] 47.0 [12.0; 71.9] 69.4 [66.0; 79.7] 17.1 [15.0; 29.2] 67.8 [63.5; 76.0] .002 .09 Data are reported as median [interquartile range]. AHI = apnea-hypopnea index, cAHI = central AHI, oAHI = obstructive AHI. consistencies (n = 3). Of those with aspiration, 6 patients had severe AHI, and 3 had moderate AHI. Thirteen infants required utilization of all 3 studies (PSG, ENT evaluations, and swallow studies) during evaluation. These included 7 preterm infants and 6 term infants. Figure 2—Improvement in AHI for all patients with followup studies. DISCUSSION There is a paucity of data on the clinical value of PSG in infants and our study adds important findings to the use of this technology in the NICU. The principle indications for an IPPSG were recurrent desaturations, suspected obstructive apnea and stridor, in both preterm and term infants with a variety of comorbidities. In most infants the IPPSG demonstrated moderate AHI (23%) or severe AHI (74%), and results differed significantly depending on the comorbidity. Thus craniofacial and airway anomalies had the highest AHI, followed by infants with neurologic abnormalities, and lowest among those with respiratory abnormalities. An ENT examination with awake flexible fiberoptic laryngoscopy, followed by DISE and/or direct laryngoscopy and bronchoscopy if inconclusive, was an important aspect of the workup in neonates with OSA. We observed that targeted interventions, based on the PSG findings, led to complete resolution of clinical signs or improvement in AHI in most patients. Although a limited study with only 31 patients, these were complex infants selected for a high suspicion of obstructive or central apnea with an attempt to find the diagnosis that would provide the most meaningful information to the treatment team. The diagnostic value of IPPSG, along with advances in technology, has enhanced the ability to perform IPPSGs in the NICU, and consequently has facilitated more studies being done in our unit in those with suspected recurrent central or obstructive apnea. Although most patients with follow-up studies had improved AHIs and resolution of symptoms, none “normalized” with an AHI < 1 event/h. The definition normal sleep apnea in a population of premature infants and term infants with underlying illnesses is not clear. Preterm infants who reach a postconceptual age of 40 weeks and term infants have been shown to have similar breathing patterns.15 In term infants one study found an obstructive apnea rate of 0.6 events/h at 3 weeks, 1.1 event/h at 6 weeks, 0.4 events/h at 3 months, and 0.2 events/h at 6 months of age,19 and another found a obstructive apnea rate of 0.7 events/h at 1 month, 0.6 events/h at 3 months, and 0.2 events/h at 6 months of age.20 In preterm infants, an obstructive apnea rate of 1 event/h was observed at a post-conceptual age of Journal of Clinical Sleep Medicine, Vol. 17, No. 8 The ends of the box are the upper and lower quartiles, the median is marked by the horizontal line inside the box and the two lines outside the box represent the highest and lowest AHI values. The black lines connect each patient’s AHI on initial study to AHI on final study. AHI = apneahypopnea index, PSG = polysomnography. 40 weeks, 0.7 events/h at a post-conceptual age of 44 weeks, and 0.5 events/h at a post-conceptual age of 52 weeks.20 More recently Daftary et al showed in term infants a mean AHI of 14.9 events/h with hypopneas being the most common, followed by central (5.4 events/h), obstructive (2.3 events/h), and mixed (1.2 events/h) apneas.21 Clinical significance for normal AHI values is likely in between these observations, although average AHI values for preterm infants and term infants with underlying illnesses still remains unclear. In infants, there is a known association between OSA and craniofacial and upper airway anomalies. Tawfik et al looked at the incidence of PSGs in a pediatric population less than 1 year of age and found laryngomalacia and craniofacial anomalies highly predictive of inpatient PSGs.10 In a case series of infants with a mean age of 4.6 months diagnosed with OSA, 24% had laryngomalacia and 16.5% had a craniofacial abnormality, with the AHI being moderate in 20% and severe in 39% of cases.22 1660 August 1, 2021 J Kim, S Gueye-Ndiaye, E Mauer, et al. Polysomnography use in complex term and preterm infants Separate studies have similarly shown that craniofacial anomalies are strongly associated with OSA in infants, and specifically those with Pierre Robin sequence have been shown to have a high prevalence of OSA.23,24 Our study in the NICU was consistent with these studies showing that neonates with craniofacial (all micrognathia) and airway anomalies all had OSA with a median AHI of 50.0 events/h. Improvements in AHI have been shown following surgical treatment of micrognathia with distraction osteogenesis in infants less than 1 year of age25 and following surgical treatment of laryngomalacia with supraglottoplasty in children as young as 1 month of age.26,27 In our population, 7 infants with micrognathia underwent mandibular distractions and 1 had a tongue-lip adhesion. One infant with laryngomalacia underwent supraglottoplasty. Eight of these patients had follow-up IPPSGs that all showed improvement in AHI. Additional surgical treatments included tracheostomy in infants diagnosed with tracheal sleeve, soft palate collapse/glossoptosis, and choanal atresia with retroflexion of epiglottis. Additional medical treatments included HFNC for laryngomalacia and hypopharyngeal collapse. The infant with hypopharyngeal collapse (patient no. 11) was the only patient who did not show an improvement in the AHI after treatment. This patient, initially started on CPAP, was transitioned to HFNC due to worsening cAHI. A further escalation of respiratory support was considered, but when planning an infant’s disposition, home CPAP for infants younger than 1 year of age is not the standard discharge protocol in our NICU. HFNC is better tolerated and is the treatment for OSA in this patient population. An equally important aspect of the work-up for all these patients were ENT evaluations that included an awake flexible fiberoptic laryngoscopy followed by a DISE and/or direct laryngoscopy and bronchoscopy if inconclusive. ENT evaluations sometimes preceded PSG when the diagnosis was obvious, such as micrognathia, but in many cases with a severe oAHI and unclear diagnosis, more invasive evaluation was necessary and invaluable in determining a diagnosis. Our results show that in a select population of infants with craniofacial or airway comorbidities and concern for OSA, IPPSG in the NICU with supportive ENT evaluation can be used to guide surgical and medical treatment and may be an important aspect in targeting therapies to individual needs. Similar to patients with craniofacial and airway anomalies, patients with a variety of neurologic comorbid conditions have been shown to have an increased incidence of OSA or hypoventilation compared to neurologically normal children.5 Specifically those with hypotonia (eg, Down syndrome) and neuromuscular diseases have been shown to have increased risk for OSA.7,28 A prospective cohort study of neonates admitted to an NICU with suspected seizures demonstrated a median AHI of 12.3 events/h with predominantly central apneas,11 and a casecontrol study of infants with myelomeningocele admitted to the NICU showed a higher AHI in those with myelomeningocele vs controls (34.2 events/h vs 19.3 events/h) with predominantly central apneas. In those with abnormal PSGs who returned for clinical follow-up, 5 were treated with caffeine and 4 received supplemental O2 for CSA.12 In our study we found a median AHI of 44.3 events/h that was higher than those seen in previous studies. This is likely due to the fact that 3 of the 5 infants had Journal of Clinical Sleep Medicine, Vol. 17, No. 8 OSA, which seems to be associated with a higher AHI compared to those with CSA for infants in the NICU. Of the 3 infants with OSA, 1 required a tracheostomy due to significant hypotonia, 1 was treated with CPAP, and another was recommended for a tracheostomy but redirected care. Two infants with CSA were treated with caffeine and O2 via nasal cannula. Compared to previous studies that have looked at targeting therapies for infants, we showed that IPPSG can be applied to neonates with neurologic comorbidities in the NICU, leading to clinical improvement. IPPSG may also be valuable in targeting treatment for infants with apnea of prematurity. For most preterm infants (approximately 98%) the expected resolution of apnea of prematurity has been shown to occur by 40 weeks PMA.29 However for infants who have apnea that persists beyond this period, the cause is often multifactorial related to central or obstructive apnea and/or feeding related issues.1,2 In a review of the literature, 1 study used polygraphy in infants with apnea of prematurity who did not respond to caffeine. Those presumed to have gastroesophageal reflux disease were treated with an antireflux regimen,30 although a more recent clinical report found there is no evidence to suggest that treatment of gastroesophageal reflux disease decreases the risk of apnea.31 No other studies to our knowledge have examined the diagnostic use of PSG in evaluating recurrent apnea to guide treatment in the NICU. In this report 7 premature infants (mean PMA 41-3/7 weeks) presented with recurrent desaturation and bradycardic events consistent with a clinical diagnosis of apnea of prematurity and sleep-disordered breathing. Three of these infants had CSA and 4 had OSA. The IPPSG helped target treatment to the specific causes of apnea with clinical improvement seen in all of these patients. Although PMA is strongly associated with CSA, obstructive AHIs change minimally during the first year of life and significant improvements in obstructive AHI are assumed to be due to the intervention. These findings suggest that the use of IPPSG may be helpful in differentiating the etiology of recurrent apnea in infants to facilitate evaluation and targeted treatment in preterm infants. Limitations This was a retrospective study done at a single level-IV referral center NICU, which may have led to a selection bias of patients for more severe symptoms and treatment options not available in other NICUs. The study also described infants over a 6-year period which may have affected the data as a result of potential changes of practice in neonatology and sleep medicine over this time period. The small number of infants enrolled in this study and the diversity of medical conditions present may have limited the ability to determine the appropriate indications for PSG and did not allow for more elaborate statistics and conclusions. Last, we want to emphasize that although a majority of infants had abnormal results, this does not represent the prevalence of apnea in infants but rather the presence of apnea in infants with underlying illness and clinical suspicion of apnea. The selection of study participants based on clinical opinion limits the generalizability of the study to different NICUs. In spite of all these limitations, the goal was to introduce the potential role of utilizing PSG as a diagnostic tool for infants in the NICU 1661 August 1, 2021 J Kim, S Gueye-Ndiaye, E Mauer, et al. Polysomnography use in complex term and preterm infants 8. Tkachenko N, Singh K, Abreu N, et al. Establishing a role for polysomnography in hospitalized children. Pediatr Neurol. 2016;57:39–45.e1. who present recurrent desaturation episodes and suspected obstructive apnea. 9. Zenteno D, Rodríguez-Núñez I, Molina I, et al. [Polygraphy in hospitalized children under 3 months]. Rev Chil Pediatr. 2017;88(2):230–235. 10. Tawfik KO, Sedaghat AR, Ishman SL. Trends in inpatient pediatric polysomnography for laryngomalacia and craniofacial anomalies. Ann Otol Rhinol Laryngol. 2016;125(1):82–89. CONCLUSIONS To our knowledge this is one of the few reports on the diagnostic value of IPPSGs in the NICU in infants with recurrent desaturation episodes, suspected obstructive apnea, or both. In this patient population AHI was moderate to severe in most infants (86%), and most often obstructive in nature (74%). Targeted medical/surgical interventions resulted in clinical improvement in 22 infants (71%) and improvement on follow-up studies in 12 out of 13 infants. These findings indicate that PSGs in the NICU, coupled with concomitant studies, are an important diagnostic tool in evaluating and guiding management of complex term and preterm infants with recurrent apnea. Prospective studies will be required to determine clear guidelines and indications for performing PSGs in the NICU. 11. Meerkov MS, Hassan F, Chervin RD, Barks JD, Carlson MD, Shellhaas RA. Sleep-disordered breathing is common among term and near term infants in the NICU. Pediatr Pulmonol. 2019;54(5):557–562. 12. Shellhaas RA, Kenia PV, Hassan F, Barks JDE, Kaciroti N, Chervin RD. Sleepdisordered breathing among newborns with myelomeningocele. J Pediatr. 2018; 194:244–247.e1. 13. Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5): 597–619. 14. Beck SE, Marcus CL. Pediatric polysomnography. Sleep Med Clin. 2009;4(3): 393–406. 15. Katz ES, Mitchell RB, D’Ambrosio CM. Obstructive sleep apnea in infants. Am J Respir Crit Care Med. 2012;185(8):805–816. 16. Ng DK, Chan CH. A review of normal values of infant sleep polysomnography. Pediatr Neonatol. 2013;54(2):82–87. ABBREVIATIONS 17. Daftary AS, Jalou HE, Shively L, Slaven JE, Davis SD. Polysomnography reference values in healthy newborns. J Clin Sleep Med. 2019;15(3):437–443. AHI, apnea-hypopnea index cAHI, central apnea-hypopnea index CPAP, continuous positive airway pressure CSA, central sleep apnea DISE, drug-induced sleep endoscopy ENT, ear, nose, and throat EtCO2, end-tidal CO2 HFNC, high-flow nasal cannula IPPSG, inpatient polysomnography NICU, neonatal intensive care unit oAHI, obstructive apnea-hypopnea index OSA, obstructive sleep apnea PMA, mean postmenstrual age PSG, polysomnography 18. R Core Team. A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2019. 19. Guilleminault C, Ariagno R, Korobkin R, et al. Mixed and obstructive sleep apnea and near miss for sudden infant death syndrome: 2. Comparison of near miss and normal control infants by age. Pediatrics. 1979;64(6):882–891. 20. Hoppenbrouwers T, Hodgman JE, Cabal L. Obstructive apnea, associated patterns of movement, heart rate, and oxygenation in infants at low and increased risk for SIDS. Pediatr Pulmonol. 1993;15(1):1–12. 21. Daftary AS, Jalou HE, Shively L, Slaven JE, Davis SD. Polysomnography reference values in healthy newborns. J Clin Sleep Med. 2019;15(3):437–443. 22. Ramgopal S, Kothare SV, Rana M, Singh K, Khatwa U. Obstructive sleep apnea in infancy: a 7-year experience at a pediatric sleep center. Pediatr Pulmonol. 2014; 49(6):554–560. 23. Anderson IC, Sedaghat AR, McGinley BM, Redett RJ, Boss EF, Ishman SL. Prevalence and severity of obstructive sleep apnea and snoring in infants with Pierre Robin sequence. Cleft Palate Craniofac J. 2011;48(5):614–618. 24. Lam DJ, Jensen CC, Mueller BA, Starr JR, Cunningham ML, Weaver EM. Pediatric sleep apnea and craniofacial anomalies: a population-based casecontrol study. Laryngoscope. 2010;120(10):2098–2105. REFERENCES 1. Eichenwald EC, Aina A, Stark AR. Apnea frequently persists beyond term gestation in infants delivered at 24 to 28 weeks. Pediatrics. 1997;100(3):354–359. 25. Almajed A, Viezel-Mathieu A, Gilardino MS, Flores RL, Tholpady SS, Côté A. Outcome following surgical interventions for micrognathia in infants with Pierre Robin sequence: a systematic review of the literature. Cleft Palate Craniofac J. 2017;54(1):32–42. 26. Farhood Z, Ong AA, Nguyen SA, Gillespie MB, Discolo CM, White DR. objective outcomes of supraglottoplasty for children with laryngomalacia and obstructive sleep apnea: a meta-analysis. JAMA Otolaryngol Head Neck Surg. 2016;142(7): 665–671. 27. Camacho M, Dunn B, Torre C, et al. Supraglottoplasty for laryngomalacia with obstructive sleep apnea: A systematic review and meta-analysis. Laryngoscope. 2016;126(5):1246–1255. 2. Martin RJ, Miller MJ, Carlo WA. Pathogenesis of apnea in preterm infants. J Pediatr. 1986;109(5):733–741. 3. Buchenau W, Urschitz MS, Sautermeister J, et al. A randomized clinical trial of a new orthodontic appliance to improve upper airway obstruction in infants with Pierre Robin sequence. J Pediatr. 2007;151(2):145–149. 4. Monasterio FO, Drucker M, Molina F, Ysunza A. Distraction osteogenesis in Pierre Robin sequence and related respiratory problems in children. J Craniofac Surg. 2002;13(1):79–83, discussion 84. 5. Masters IB, Harvey JM, Wales PD, O’Callaghan MJ, Harris MA. Clinical versus polysomnographic profiles in children with obstructive sleep apnoea. J Paediatr Child Health. 1999;35(1):49–54. 28. Suresh S, Wales P, Dakin C, Harris MA, Cooper DG. Sleep-related breathing disorder in Duchenne muscular dystrophy: disease spectrum in the paediatric population. J Paediatr Child Health. 2005;41(9-10):500–503. 6. Goldberg S, Shatz A, Picard E, et al. Endoscopic findings in children with obstructive sleep apnea: effects of age and hypotonia. Pediatr Pulmonol. 2005; 40(3):205–210. 29. Henderson-Smart DJ. The effect of gestational age on the incidence and duration of recurrent apnoea in newborn babies. Aust Paediatr J. 1981;17(4): 273–276. 30. Paul K, Melichar J, Miletín J, Dittrichová J. Differential diagnosis of apneas in preterm infants. Eur J Pediatr. 2009;168(2):195–201. 7. Brooks LJ, Olsen MN, Bacevice AM, Beebe A, Konstantinopoulou S, Taylor HG. Relationship between sleep, sleep apnea, and neuropsychological function in children with Down syndrome. Sleep Breath. 2015;19(1):197–204. Journal of Clinical Sleep Medicine, Vol. 17, No. 8 1662 August 1, 2021 J Kim, S Gueye-Ndiaye, E Mauer, et al. Polysomnography use in complex term and preterm infants Children’s Hospital, 525 East 68th Street, N-506, New York, NY 10065; Tel: (212) 746-3530; Email: jmk9018@med.cornell.edu 31. Eichenwald EC; Committee on Fetus and Newborn. Diagnosis and management of gastroesophageal reflux in preterm infants. Pediatrics. 2018; 142(1):e20181061. SUBMISSION & CORRESPONDENCE INFORMATION DISCLOSURE STATEMENT Submitted for publication August 17, 2020 Submitted in final revised form March 16, 2021 Accepted for publication March 16, 2021 Address correspondence to: James Kim, MD, Division of Newborn Medicine, New York-Presbyterian Hospital–Weill Cornell Medical Center, Komansky Journal of Clinical Sleep Medicine, Vol. 17, No. 8 All authors have seen and approved the manuscript. Work for this study was performed at New York-Presbyterian Hospital – Weill Cornell Medical Center, Komansky Children’s Hospital. The authors report no conflicts of interest. 1663 August 1, 2021