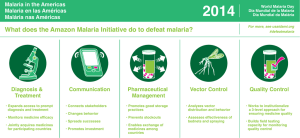
Costing analyses for interventions to be implemented by the
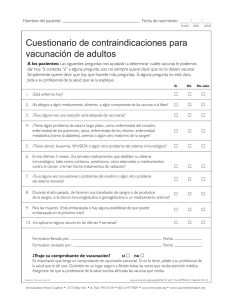
Anuncio

Costing analyses for interventions to be implemented by the Mesoamerican Health Initiative Instituto Nacional de Salud Pública Prepared by: Aracena Genao, Belkis Danese De Los Santos, Laura González Domínguez, Dayana Martínez Pérez, Araceli Sosa Rubi, Sandra Valencia-Mendoza, Atanacio Cuernavaca, Mexico, December 2009 CONTENTS BACKGROUND AND INTRODUCTION ...................................................................... 33 PRINCIPLES OF COSTING ........................................................................................... 55 Direct incremental unit costs ................................................................................................55 Incremental unit costs .............................................................................................................66 Costing Methods Overview .....................................................................................................66 Data Collection ...................................................................................................................................... 77 Data Management and Cost Estimations ................................................................................... 77 VECTOR-BORNE DISEASES ........................................................................................ 77 Methods .........................................................................................................................................77 Description of the interventions ................................................................................................... 88 Methods for unit costs estimation........................................................................................... 11 Estimation of the resource needs for Malaria .................................................................... 13 Estimation of the resource needs for Dengue .................................................................... 14 Data sources ..................................................................................................................................... 15 Results ..................................................................................................................................... 15 Malaria ................................................................................................................................................ 15 Dengue ................................................................................................................................................ 17 Discussion: ............................................................................................................................. 19 IMMUNIZATIONS..................................................................................................... Methods ................................................................................................................................... Interventions.................................................................................................................................... Vaccines costs .................................................................................................................................. Scaling-up .......................................................................................................................................... Results ..................................................................................................................................... Discussion .............................................................................................................................. NUTRITION ............................................................................................................... 19 19 19 21 23 24 24 27 Methods ................................................................................................................................... 27 Interventions and ........................................................................................................................... 27 target populations.......................................................................................................................... 27 Delivery Platforms ......................................................................................................................... 28 Results ..................................................................................................................................... 30 1. Promotion of breastfeeding and appropriate complementary feeding practices ................................................................................................................................................................ 31 2. Improved water, sanitation, and hygiene behaviors .................................................. 32 3. Prenatal micronutrient supplements ................................................................................ 33 4. Universal food fortification programs ............................................................................. 33 5. Vitamin A supplementation .................................................................................................. 34 6. Therapeutic zinc supplements ............................................................................................. 34 7. Multiple micronutrient powders ........................................................................................ 34 8. Clinical management of severe acute malnutrition (SAM) ...................................... 35 9. Fortified complementary food - Prevention/treatment of moderate malnutrition. ................................................................................................................................................................ 35 Discussion .............................................................................................................................. 36 MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH .............................. 36 Methods ................................................................................................................................... 36 1 Interventions.................................................................................................................................... 36 Costs analysis ................................................................................................................................... 37 Results ..................................................................................................................................... 37 Panama .................................................................................................................................................... 37 Mexico ...................................................................................................................................................... 38 Guatemala............................................................................................................................................... 39 Nicaragua................................................................................................................................................ 39 Discusion ......................................................................................................................................40 CONSULTED BIBLIOGRAPHY .................................................................................... 41 ANEXXES......................................................................................................................... 43 2 BACKGROUND AND INTRODUCTION Funded by the Bill & Melinda Gates Foundation (BMGF), the Mesoamerican Health Initiative (MHI) is a joint regional effort, which seeks to reduce health disparities among Mesoamerican populations. To this end, MHI has established four thematic axes according to the most relevant health conditions in Mesoamerica, namely relating to: nutrition, maternal and child health, vaccination and vector-borne diseases, particularly malaria and dengue fever. The Mesoamerican region is formed by the seven countries of Central America (Belize, Costa Rica, El Salvador, Guatemala, Honduras, Nicaragua, and Panama) and the ten states of the Southeastern region of Mexico (Campeche, Chiapas, Guerrero, Morelos, Oaxaca, Puebla, Quintana Roo, Tabasco, Veracruz, and Yucatan). In 2008, the total population across the Mesoamerican region was estimated to be approximately 71,785,000 inhabitants, where 41,778,000 were of Central America and 30,007,000 were of Southeastern Mexico. The region is generally poor, but there are marked differences in economic development and per capita income. For example, per capita income, as defined by the World Bank, ranges from ―very low‖ in Nicaragua (US$1.025, ranked 142nd out of 182 countries) to ―mediumlow‖ in Panama (US$6.784, ranked 71st in the same World Bank list) (World Bank, 2009). The region is considered to be in the process of urbanization, albeit with significant differences among countries. While Panama is 73.2% urban, Honduras and Guatemala have the lowest proportions of urban population at 47.9% and 48.5%, respectively. The proportion of the population who is indigenous also varies greatly among countries: 40% of Guatemala’s population is comprised of indigenous groups, while in Costa Rica and El Salvador, only 1.7% and 0.2% of the populations, respectively, are indigenous. On the other hand, there are several aspects in which the countries present very similar characteristics — mainly related to inequalities in the access to and quality of services available for the poor, rural populations, and indigenous people. Health systems are chronically underfinanced and the resources available tend to concentrate in more metropolitan areas, where the majority of qualified health personnel also are concentrated. Additionally, due to rapid rates of urbanization, many population groups are living in marginalized urban areas in conditions equal to or worse than those found in rural areas. To address the specific components under each of the MHI axes (nutrition, maternal and child health, vaccination and vector-borne diseases), technical thematic groups have been formed from the following participants: representatives from the Ministries of Health (MoH) in Belize, Guatemala, Honduras, El Salvador, Nicaragua, Costa Rica, Panama, and Mexico; regional and international experts in the four MHI intervention areas; and representatives from several collaborating agencies. To select health interventions specific to each of the four components of focus for the MHI, extensive literature reviews were conducted in parallel to identify evidence-based practices that have effectively been shown to be effective and 3 cost-effective. This required documenting outcomes, impacts, and the costeffectiveness of a variety of health interventions, the most promising health interventions were then selected from what had been gathered. These interventions were discussed extensively within the working group and with the country representatives. In October 2009, each of the four technical thematic groups released a master plan according to its respective component of health and in which a series of interventions had been proposed for scale-up as part of the MHI. The objectives stated in the master plans are the following: The main objective of the nutrition component is to reduce the prevalence of maternal and child undernutrition in Mesoamerica by supporting the evidence-based and effective implementation of programs and regional actions. The primary target populations are children less than 2 years of age and pregnant or breastfeeding women who live in poor and disadvantaged households or belong to disadvantaged populations, such as indigenous populations. The objectives of the maternal, neonatal and reproductive health component are to reduce maternal mortality by 75%, reduce neonatal mortality by 50%, and achieve universal access to reproductive health services, including family planning by the year 2015, in line with the United Nations 2009 Millennium Development Goals (MDGs) report. The main objective of the vaccination component is to systematically identify the barriers to vaccination in the most vulnerable populations in Mesoamerica and to use innovative approaches to address the barriers in order to achieve ≥ 90% effective vaccination coverage among target populations, as well as to decrease the burden of vaccine-preventable diseases and childhood mortality in the most vulnerable populations. The objectives of the vector-borne diseases component are to eliminate local malaria transmission in the Mesoamerican Region (southern Mexican states and all countries in Central America) and to effectively reduce dengue transmission and mortality in Mesoamerica. Although the master plan suggests a basic package of health interventions, policy makers in each country must define the specific strategic plan to allocate resources in order to cover health needs and reduce health disparities in specific areas within their countries. One of the critical steps before scaling-up the interventions will be to generate information on how much additional funding is necessary to reach desired levels of coverage and to generate information on the particular levels of coverage that are achievable given particular amounts of resources. A large number of studies have attempted to estimate global resource needs for the scaling-up of health interventions aimed at meeting MDGs 1, 4, 5, and 6, which overlap with the MHI objectives. However, these single global estimates of intervention costs are not precisely relevant to individual countries or regions of the MHI, since global estimates for the MDGs tend to have a greater emphasis on costs estimated for Africa and Asia, where personnel and supply costs differ from those for the Mesoamerican region. 4 The objective of this analysis is to estimate direct incremental unit costs of the interventions proposed for the MHI in the areas of nutrition and maternal, neonatal and reproductive health. In the case of the vector-borne diseases and vaccines components, we estimate incremental unit costs (taking into account direct and indirect costs) at the time that we present preliminary projections of the resource needs to meet the objectives. It is important to mention that for the specific interventions proposed by the technical thematic groups, some information required to estimate resource needs is lacking in the master plans and initial diagnostics. For instance, except for the vaccination component, initial coverage levels for the interventions planned for scale-up are missing, which has introduced difficulties in estimating the extent to which interventions need to be scaled-up to meet the objectives. Secondly, a diagnostic tool for infrastructure availability and capacity utilization rates is missing, which is very important to know where and to what degree interventions can be scaled-up. Finally, there is not a diagnostic to measure current human capacity availability, which is also important to determine where and to what degree interventions can be scaled-up. During the writing of this document, it has not been possible to accurately estimate resource needs to meet the MHI objectives in the maternal, neonatal and reproductive health area as well as in the nutrition one. Rather, at this time, we present estimations of the incremental unit costs for the interventions, which is an important ingredient to estimate the amount of additional funding required to meet the MHI objectives once the aforementioned information is generated. Incremental unit costs as well as direct incremental unit costs will be a very useful ingredient for the Mesoamerican countries and potential donor for health financial planning and for making grants when seeking additional funding for scale-up. This document is organized as follow. First, an overview of the costing principles and methods that is common to the four health areas is given. Then we present in separate sections each of the methods, results and discussion of each health component. PRINCIPLES OF COSTING Direct incremental unit costs were estimated for the nutrition and maternal, neonatal and reproductive health, while incremental unit costs were estimated for the case of vector-borne diseases and vaccines. In this section we overview the costing principles and methods that were common to the four health areas. Direct incremental unit costs The analysis of direct incremental unit costs is concerned with marginal changes in costs, and it assumes that overhead items, such as infrastructure, administrative, among other overhead costs, will remain approximately the same while scaling-up a given set of interventions. This kind of analysis is appropriate for mobilizing resources from donors who are interested in 5 financing just the recurrent costs (no capital costs) for scaling-up interventions, just as in this case with the BMGF. Also, it is the appropriate analysis for when the planned level of scaling-up does not require an extra level of infrastructure, organizational resources, and other overheads because the organization/facility is not working at its full capacity. In contrast, using direct incremental unit costs is not an appropriate approach when scaling-up interventions requires a significant investment in infrastructure, administrative staff, and other overheads. In such a case, an assessment of the required investment in overheads would be necessary. Incremental unit costs The analysis of incremental unit costs is concerned with marginal changes in costs, and it allow variations in overhead items, such as infrastructure, administrative, among other overhead costs, while scaling-up a given set of interventions. As apposite to the direct incremental unit costs, this kind of analysis is appropriate for mobilizing resources from donors who are interested in financing the total cost ofscaling-up interventions. This is the appropriate analysis when planning to scale-up interventions that requires a significant investment in infrastructure, administrative staff, and other overheads. It is also necessary to clarify that both type of analyses do not include the costs necessary to ensure that the intervention activities are able to function well, nor does it include health information system and monitoring and evaluation costs. Some governance aspects, such as improving strategic vision, accountability, transparency (including regulation), participation, and consensus orientation, which could be required for a successful implementation of the MHI, are not costed in the MHI. Costing Methods Overview For the case of the nutrition; vector-borne diseases and maternal, neonatal and reproductive health areas, the interventions’ incremental unit costs were obtained using an ingredients approach. In the ingredients approach, the cost of any input to a production process is the product of the quantity used and the value (or price) of each unit. The ingredients approach is useful for many reasons. The most important are that it allows analysts and policy-makers to validate the assumptions used, to judge whether estimates presented can be applied to their settings, and, if necessary, to change some of the parameters to replicate the analysis for their settings. All costs are expressed in terms of 2009 constant, rather than current US dollars. They therefore do not try to project rates of inflation, but they reflect real costs. For the case of the vaccination area, a mixed approach was used. In such approach the costs analysis was split into two parts, vaccine costs and nonvaccine costs. The vaccine costs were estimated using an ingredients approach, while the non-vaccine costs of scaling-up vaccination was extrapolated to the Mesoamerican countries from published literature (more details are given in the vaccines section). 6 Data Collection For the nutrition; vector-borne diseases and maternal, neonatal and reproductive health components of the MHI, the interventions in the master plans were translated into quantities of ―ingredients‖ or quantities of inputs (personnel time, medicines, medical supplies, etc.) directly needed to carry out them. Such translations were obtained through structured interviews with experts in each of the four components. To prepare the structured interviews, literature and clinical guidelines were reviewed to get a sense of the resources necessary for each intervention. For the maternal, neonatal and reproductive health interventions, the quantities of ingredients were obtained by interviewing nurses, physicians and obstetrician/gynecologists involved in obstetric and neonatal care. For the nutrition, immunization, and vector-borne areas, interviews were carried out with program managers in the respective components to translate interventions into ingredients. Once the information on quantities of ingredients was obtained, we developed instruments for price and cost data collection (the instruments are supplemented in separate files). In order to collect cost data from the countries in the Mesoamerican region, these cost data collections instruments were sent to the component-specific representatives from all of the MoHs. Collected cost data is provided in a separate supplemented Excel file. Data Management and Cost Estimations Collected data were compiled and compared to form the basis of a set of costing sheets in Excel for the different interventions. The cost of each intervention was obtained by the sum of the products of the quantity used and the value (or price) of each unit of inputs. Equipment and vehicle costs were considered as capital costs in the case of the vector-borne diseases and vaccines components. Following standard practice, capital costs were annualized over the useful life of the factor input, i.e. the 'equivalent annual costs' were calculated. For country-specific analysis, the local rate of return on long-term government bonds would ideally be used as the social discount rate for costs. For our purposes, a 3% discount rate was used, as recommended by most economic evaluation guidelines (Drummond et al., 1997). All costs figures were converted to 2009 dollars using the exchange rates for November 12, 2009 according to the different currencies within the Mesoamerican region. VECTOR-BORNE DISEASES Methods The resource and cost estimation processes detailed in this report were conducted between September and December 2009. The main purpose of this exercise was to calculate the needed resources to confront dengue and malaria issues in the Mesoamerica region. All eight Mesoamerican countries (i.e. Honduras, Nicaragua, Guatemala, Costa Rica, El Salvador, Panama, Belize, and the southeastern part of Mexico) within the initiative were 7 considered in this report, and calculations were performed to reach effective levels of control for dengue and malaria in the region. Description of the interventions Malaria Selecting the interventions for malaria control are essentially focused on avoiding the vector-to-human mode of transmission, as well as fighting the effects associated with the disease. In that context, actions that would direct the effective control of malaria, and even its eradication in the near future, were identified. These actions were organized in four packages that differed in terms of the combination of included interventions and the time and duration proposed for each intervention’s application. The design of the four intervention packages was based on the length of malaria persistence among targeted communities, and this report on resources is based on this structure; therefore, it is important to mention the difference among the strata. The first stratum contains the communities that have had seven or more years of persistence in the transmission of malaria. The second stratum contains the communities that have had four to six years of persistence. The third stratum corresponds to the communities that have had a malaria persistence of two or three years. The last stratum consists of those communities that have had one year of malaria persistence. The four packages contain similar interventions with minor differences among each other. The first group of actions Focalized Intensive Treatment (TFzI) consists of offering a unique dose of malaria treatment per month for a period of three months. At the same time of delivery as the first dose, 100% of the houses in the community and it’s periphery will be sprayed based on the radio of flight of the vector and the resting places of the mosquito. Another action included in this package is the cleaning of natural breeding places, and the application of larvicide in those places where the entomological study has made recommendations. The delivery of insecticide-treated bednets (ITNs) was another action included. Additionally, the working group came to a consensus about the need of strengthening the epidemiological alertness, and following this construction of this objective, they proposed the establishment of a network consisting of volunteer notifiers (1 for every 100 inhabitants). In this package, the delivery of medicines to confirmed cases of malaria and cohabitants of the cases has been included, along with the active surveillance of those cases by personnel of the malaria control program in applicable countries. The second package Focalized Treatment (TFz) includes the spraying of 100% of the houses within the community, treatment with the massive unique dose treatment, distribution of ITNs, strengthening the epidemiological alertness, treatment of confirmed cases and cohabitants, and additional measures of physical control. The Focal Treatment (TFc), the third package of actions, includes the focus on spraying houses only where cases have been reported and have also received treatment, in addition to strengthening the epidemiological surveillance and evaluation of the usage of ITNs, according to the characteristics of the community. 8 The fourth group of actions (VEE) was specifically directed to the epidemiological and entomological surveillance alertness and the focused treatment of detected cases. The expectation of this group was that at the moment of implementing this package, the levels of malaria transmission would be completely controlled and the presence of cases would be very low. The implementation structure for these groups is depicted below in Table 1.1. Table 1.1. Interventions for malaria: implementation structure for the four targeted groups. Stratum 1 TFzI TFz TFc + VEE TFc + VEE I II III IV 2 TFz TFz TFc + VEE TFc + VEE 3 TFz TFz VEE VEE Years 4 TFc TFc VEE VEE 5 TFc TFc VEE VEE 6 TFc VEE VEE VEE Dengue Regarding dengue, the strategies were conceived in three categories: (1) The actions of control, including: domestic hygiene promotion (physical control measures), community participation interventions (environmental control), elimination of disposable breeding sites (clean-up campaigns), control of breeding sites (application of chemical or biological agents), insecticides spraying (focalized in areas where cases have been confirmed), emergency control (aerial spraying of insecticides in outbreak situations); (2) The adequate management of severe cases by strengthening clinical capabilities of health personnel to adequately identify and treat severe dengue cases, which is the most appropriate intervention to prevent premature mortality (lethality) by dengue infection. (3) Definition of surveillance and control interventions by stratifying the levels of risk and population size. Control interventions are implemented according to the population size (< 100,000, 100,000 to 350,000, and >350,000) into: Basic: passive surveillance, community participation (CP) and health promotion (HP) with local resources Selective: active surveillance, CP, HP, elimination and control of productive breeding sites, focalized treatment of areas with transmission Integrated and intensive: active surveillance, early case detection, CP, HP, elimination and control of productive breeding sites before and after transmission cycles, focalized treatment of areas with transmission, use of ovitraps, entomological surveys to measure the impact of control 9 According to level of risk, localities are defined as: Low-risk: occasional dengue transmission Moderate-risk. Irregular dengue transmission High-risk: frequent dengue transmission, concentration of more than 50% of cases, detection of severe dengue The package of interventions is organized to universally cover all areas at-risk with at a minimum of actions: community participation schemes, environmental control and elimination of breeding sites, and clinical management of cases. As the risk increases, the type and intensity of the interventions proposed in lower risk areas does as well. For example, elimination of breeding sites in high-risk areas will be performed before, during, and after the transmission period, while in moderate- and low-risk areas, it will be performed only before the transmission period. The idea behind the strategy to intensify the elimination of breeding sites after the transmission period was to decrease the risk of vertical transmission to emerging adult female mosquitoes that could reignite transmission early in the next season. In the same sequence, the use of insecticide spraying with ultralow volume (ULV) was restricted to high-risk areas and areas with intensive transmission, regardless of their risk situation. The organization for detecting dengue cases by levels of risk was based on the passive surveillance of suspected cases already in place in the low-risk areas and was supported by the health reports of health units and under the notification rules within each country. The detection of cases in moderate-risk areas will be supported by the establishment of febrile clinics in an attempt to detect early cases of dengue, especially in areas classified as high-risk by entomological surveys. In high-risk areas, case detection activities will be intensified once a case is confirmed within 100 to 300 meters around the suspected index case. Community participation and health promotion Community involvement and health promotion strategies will be an essential component of the vector control activities, especially in the low- and moderate- risk areas where other interventions will not be so intensive. It is expected that community participation will be modulated by the entomological environment and intensified according to the transmission period. Emphasis should be established before the transmission period starts in order to decrease the availability of breeding sites before the rainy season. Health promotion will guide the community as to what activities must be performed in order to tackle the main breeding sites and to identify the warning signs that correspond to increased risks of severity for dengue infection. Environmental control of breeding sites Multisectorial involvement will be required to tackle the main determinants of dengue breeding environment. Besides the health sector, municipal and government agencies responsible for urban planning must be incorporated into discussions in order to recover urban public spaces and reduce the breeding potential in urban centers by improving basic urban infrastructure and the provision of regular potable water. 10 Elimination and control of breeding sites Efforts toward the control of larval densities are focused on the threshold of less than 1% of households with breeding mosquitoes in order to reduce transmission risks. These levels of control are not attainable in all countries, nor in every urban center or city in the region. Therefore, the strategy proposes to concentrate the control efforts toward targeting the most productive breeding sites and eliminating risks of disposable breeding. These activities should be performed before the transmission cycle and the rainy season in the low- and moderate-risk areas and intensified in the high-risk areas before, during, and after the transmission cycle in order to reduce the vector densities all year long and prevent the vertical transmission into the next season. Focalized treatment Evidence demonstrates the clustering of dengue transmission in the early stages of the epidemic and around the first index cases; therefore, the strategy considers the performance of intensive control actions around index cases and the houses surrounding such cases in order to decrease dispersal of transmission on a local and regional basis. Actions must be performed at the earliest detectable moment possible for a suspected or confirmed case, and the actions that must be performed include spraying of households, elimination and control of breeding sites, intensive search for febrile cases until confirmation in an area within 100 to 300 meters of a care depending on the ability of detection (the shorter distance, the earlier the detection). The minimum distance has been determined to be at least 9 blocks surrounding the index case. Spatial spraying and use of ovitraps Aerial spraying with ULV machines and vehicles is proposed in outbreak situations and once the interventions for control have proved inefficient. Use must be restricted to high-risk areas and in situations that outreach local resources. Ovitraps must be incorporated in high-risk areas to evaluate the impact of all interventions performed especially when insecticide spraying is used. Clinical management of cases includes upgrading skills of health personnel to identify and treat dengue cases. Issues included in the costing exercise are laboratory tests for serology and treatment costs in primary health centers as well as the costs for hospitalization of severe cases. Methods for unit costs estimation Cost data were collected and analized using an ingredients-based costing methodology based on Mexican Vectors Program guidelines (Centro de control de Enfermedades Transmitidas por Vectores-CENAVECE). The interventions were translated into input types and quantities by an expert consultant and the personnel working on the programs of dengue and malaria in Mexico. To account for the likely variability between countries in aspects, such as, inputs combination used to implement the interventions and prices/costs of such inputs, two questionnaires were designed, one for dengue and one for 11 malaria to explore local quantity and price of every input used to implement the interventions (see supplemented files 1.1 and 1.2). Both questionnaires underwent a pilot test under the responsibilities of the national program for malaria and dengue, respectively, with both programs in correspondence with the person in charge of the vectors program in Morelos, Mexico. Finally, these questionnaires were sent by e-mail to those responsible for the vector control programs in each country. In addition to the detailed questionnaires and to assess the costs for activity inputs, it was requested that each country fill out a form to register the purchase prices for each of the resources used in the activities. The calculations estimated for all the interventions were assumed to have a pyramidal structure formed by brigades, in which the basic unit is the promoter or technician of the program who functionally assumes the rolls of seeking the assets for the infected cases, as well as finding the trainer of volunteers who will notify the community in which he/she works, motivating the community to undertake measures to avoid contact with the vector and to obtain appropriate attention for an individual presenting any symptoms that suggests the presence of dengue or malaria. The pyramidal structure also includes the brigades’ functions that are related to applying insecticide both inside and outside the domicile and supporting the community activities to physically control the vector. Brigades for intervention cost estimates integrate four technicians led by one brigade commander. The brigades are grouped by sector and a head of the sector leads each sector. Over the sector is the district head, which is responsible for the supervision of all four sectors. These considerations were taken while estimating the unit costs and served to prorate those resources, and although, they are not a direct part of the cost of the interventions, they are essential to the accomplishment of activities. Regarding personnel compensation, all workers were considered to have effectively worked seven hours a day for 220 days per year. For the estimation of the intervention costs, activities were identified that may contain two or more tasks. For example, the physical treatment for breeding zones includes two big activities. First, communal meetings take place in which training and motivation is provided to the inhabitants of the community so that they understand the importance of their participation in the interventions. The second activity corresponds to the cleaning, which includes hydroentomological recognition of the affected zone, pre- and post-cleaning surveys and the cleaning itself of the breeding place. The estimation of costs of the interventions considered three groups of inputs: personnel costs, such as the salaries of the applier and the brigade leader among other personel; capital costs, which include the costs related to furniture and equipment, such as vehicle, machines for the application of the insecticide; and supplies, which includes insecticide, gasoline, and medicines. The costs attributable to the payment of per diem were included under the category for other items. The prices/costs of the items used in the analysis correspond to the average of those reported by the countries. Information on input costs was requested to all the countries in the Mesoamerican region, however we just got data from Costa Rica, Guatemala and Mexico. 12 Therefore, the average includes data from Costa Rica and Guatemala, in addition to the following reports from Mexico: the CENAVECE, the state of Morelos, and the cities of Tapachula and Tuxtla Gutiérrez in the state of Chiapas, Mexico. Capital costs were discounted at a rate of 3%. The analysis was performed from the perspective of the financer, and the estimations are annual. The populations at which the interventions were directed, which are the populations at risk, are presented in Tables 1.2 and 1.3. Table 1.2. Mesoamerica dengue epidemiology situation Country Risk population Households Belize 177,591 Costa Rica 3,793,146 El Salvador 4,417,610 Guatemala 3,374,626 Honduras 5,072,228 Mexico 24,075,769 Nicaragua 5,234,876 Panama 2,655,920 Source: PAHO 1999-2008. Average annual suspected cases 39,465 842,922 981,691 749,917 1,127,162 5,350,171 1,163,306 590,204 54 11,754 7,448 5,293 17,888 23,354 4,685 2,063 Severe dengue cases 0 55 128 18 973 2,228 266 3 Confirmed cases 7 264 6,827 931 462 16,987 1,140 654 Table 1.3. Mesoamerica malaria epidemiology situation Country Belize Costa Rica El Salvador Guatemala Honduras Mexico Nicaragua Panama Risk population Households 227,477 1,595,907 2,226 825,351 809,125 1,898,142 505,119 479,914 71,259 450,165 673 250,443 244,489 388,289 145,762 152,890 Average annual cases 746 1,693 38 17,900 997 1,880 1,745 1,745 Source: data provided by the national programs Estimation of the resource needs for Malaria The element that most influence the estimation was the specific stratum in which the communities have been organized. The households located in communities from the first stratum will be treated with intra-domiciliary spraying during the first four years of the execution of the project, and in the last two years, only 10% of the households will be sprayed. Additionally, for resource estimation, the first year, which will be the most intensive for this stratum, was the only year that accounted for the recruitment and training of one voluntary notifier per 100 inhabitants. Because the estimation of active surveillance resources included treatment for all malaria cases and the their cohabitants, each household with a malaria case was estimated to have five persons (at least 4.5 cohabitants per case). Also in the first year, resources were counted so that 100% of the inhabitants were treated with a unique dose every three months. For years 2, 3 and 4, the amount of resources were associated with offering this treatment to 50% of the inhabitants, and 15%, in the last two years. The resources for treating breeding places were estimated under the assumption of each community having three breeding places. For 13 the resource estimation, during the six-year duration of the project, resources were accounted for the plans to physically treat all breeding sites, including chemical treatment of 50% of them during the first year of project implementation. The last element considered in the estimation of resources for the malaria activities was the distribution of two ITNs for 80% of the houses within the communities. The resource estimations for the residing population in localities categorized in Stratum II assumed that 100% of households would be treated with intradomiciliary spray during the first three years, 10% in the fourth and fifth years, and given that the previously described package focuses on epidemiological surveillance, for the sixth year, the spraying of houses was not considered. The criterion for estimating resources for recruiting and training notifiers was similar to that of the previous stratum, where total resources were calculated for the first year of execution and for each 100 inhabitants having one notifier. The criterion for the active search of cases, as well as treating cases with unique dose, was similar to that of Stratum I, differing only in that in this stratum, it was assumed that this strategy was highly effective and that no more than 6% of the population presented an event associated with malaria. Additionally, the resource estimations for the physical treatment of the deposits was the same as that in Stratum I; however, since this stratum did not consider chemical handling, this intervention was not considered in the estimation. Regarding the distribution of ITNs, the method for resource estimation was similar to that explained for Stratum I. In Stratum III, all the houses of the localities were sprayed during the first two years. Similar to Strata I and II, the recruitment and training of a volunteer notifying per hundred inhabitants were included in the estimation. As for the active search for cases, in addition to the administration of single-dose treatments during the first 2 years, 100% of the awaited cases and their cohabitants were accounted for in the resource estimation. To obtain the expected cases, the average of registered cases in the past three years was used, and similar to the previous strata, 4.5 cohabitants per case was assumed. In years 3 to 5 of implementation, an annual reduction of 70% is expected, and 80%, between the fifth and sixth years. The treatment of deposits is similar to the previous stratum, and, additionally, no ITNs will be distributed among the inhabitants of these localities. Estimation of the resource needs for Dengue Estimation of resource needs for dengue control was established by taking the population in each locality and deriving the number of households with the assumption that each household has 4.5 cohabitants. Since the total number of dengue cases per locality and year for a 5-year period was not available, an average of the annual cases per year for each country was taken to estimate the resources needed for surveillance, control, and clinical management. According to epidemiological records and statistics published, we distributed the proportion of cases to the various risk levels in the following way: 70% in high-risk areas, 20% in moderate-risk, and 10% in low-risk areas. All estimates were performed according to this proportion. 14 Community participation and health promotion interventions were estimated by combining a set of strategies performed in a community, and the overall estimate of this package of activities was then attributed to every 50,000 people receiving the package twice a year. The control activities were estimated by dengue cases within a target area of 200 households as the basic parameter of the interventions. Control activities were estimated according to the distribution of cases by levels of risk. Aerial spraying was only estimated for moderate- and high-risk areas in the case of an epidemic. Intra-domiciliary spraying was estimated for moderate- and highrisk areas depending on the proportion of cases. Serological estimates for the minimum number of tests performed by country per year were derived from the number of suspected cases or the proportion of cases confirmed. Isolation tests were estimated by taking only 10% of the confirmed cases. The number of blood count tests was estimated based on the number of tests for all dengue hemorrhagic fever cases at three tests for every DHF case. Data sources The input prices used in this analysis were obtained from the reports of three countries: Costa Rica, Guatemala, and Mexico. The information regarding the useful life of the capital goods was obtained either directly from the countries or from the WHO-CHOICE database (WHO-CHOICE, 2009). As we are projecting resource needs over a period of 6 years in the future, it is important to express the resource needs for each year in prices of that year. Therefore, the rates of inflation were obtained from official agencies, such as central banks and offices of statistics representative of the country under view. Epidemiological and geographical information (e.g. whether a locality was marshy, presence of dengue, geographical and population sizes, number of households, cases) were provided by the countries representatives and by PAHO. Results Malaria Table 1.4 shows the unit costs for the malaria control interventions. The chemical treatment of the deposits was the most expensive activity, followed by the physical handling of deposits. Although this activity is community-led, it requires the support of program personnel and the participation of the promoter of the program in the verification surveys (pre- and post-cleaning of deposits), which was the element that most influenced the cost of this activity. The third most expensive activity was that of intra-domiciliary spraying. Treatment by unique dose was the cheapest activity, costing only US$1.40. 15 Table 1.4. Unit cost of Malaria control interventions Intervention Control interventions Chemical control breeding places* Intradomiciliar spraying Insecticide treated nets Community participation interventions Recruitment and training of the voluntary notifiers Physical control breeding places Treatment interventions Suppressive treatment A unique dose treatment Expression of unit costs Cost in US$ Cost per breeding chemically treated Cost per household treated Cost per net distributed 30.5 Cost per notifier 14.6 Cost per breeding physically treated 24.9 Cost per suspected case treated Cost per confirmed case treated 0.8 23.1 9.5 1.4 *Its does not included the hydroentomologicol recognition, which has a cost of US$11.90. Table 1.5 shows the estimated amount of resource needs for controlling malaria in the region of Mesoamerica by intervention type across the six years that the project is foreseen to last. The analysis by country indicates that the greatest percentage of the total resource needs corresponds to Mexico, possessing 32% of the total resources, followed by Honduras and Guatemala with 23% and 21% of the total amount, respectively. Corresponding with just 0.1% of the total resources, El Salvador possessed the smallest percentage, though this is dependent on the malaria eradication situation in the country. The distribution of resources by activity, also shown in Table 1.5, depicts how the major proportion of resources, more than the 89% of the total, will be destined to household spraying, an activity that has been identified as highpriority to prevent human-vector contact. Table 1.5. Resource needes to control malaria in Mesoamerica by country and by intervention (US$ thousands) Intradomi ciliar spraying 13,816.6 Recruitme nt and training of the voluntary notifiers 73.0 Active surveillan ce 11.8 A unique dose malaria treatment 522.4 Physical control breedingplaces 346.6 Chemical control breedingplaces 4.5 Impregnat ed nets 923.1 Total 15,697.9 Costa Rica El Salvador 16,357.3 261.7 24.2 355.9 52.5 0.1 475.9 17,527.5 4.4% 221.9 0.3 0.5 8.5 6.2 0.3 11.9 249.7 0.1% Guatemala 72,609.1 125.0 223.4 3,079.7 2,118.6 29.0 4,063.6 82,248.3 20.7% Honduras 81,301.9 127.9 137.4 3,476.8 2,418.2 95.0 4,195.2 91,752.2 23.1% 115,430.5 339.9 37.6 5,087.4 3,249.2 23.6 4,420.1 128,588.3 32.4% 15,615.2 36,712.5 81.2 72.1 25.2 22.1 541.8 1,346.0 674.2 2,162.8 12.1 27.0 764.2 2,462.0 17,713.9 42,804.6 4.5% 10.8% 352,065.0 88.8% 1,081.1 0.3% 482.2 0.1% 14,418.5 3.6% 11,028.2 2.8% 191.6 0.0% 17,315.9 4.4% 396,582.5 Country Belize Mexico Nicaragua Panama Total % Table 1.6 shows the estimates of resource needs by year across countries. Given the structure of the project, which possesses an intensive phase in the 16 % 4.0% first year, the largest percentage of the resources (25.3%) should be applied in the first year, 68% in years 2, 3, and 4. The smallest percentage (3.4%) corresponded to year 6 of activities, when actions are focused on epidemiological and entomological awareness. Table 1.6. Resource needs to malaria control in Mesoamerica for country and type of intervention (US$ thousands) Country Belize Costa Rica El Salvador Guatemala Honduras Mexico Nicaragua Panama Total % 1 5,041.3 6,221.1 64.4 22,035.0 22,681.3 26,090.3 4,939.1 13,221.6 100,294.2 25.3% 2 4,310.7 6,221.6 55.0 18,750.3 20,060.3 26,541.0 4,586.4 11,496.9 92,022.3 23.2% Year 3 4,225.8 2,763.1 56.6 18,944.1 21,166.8 29,891.1 4,003.9 11,639.6 92,690.9 23.4% 4 1,400.1 1,721.7 59.2 17,670.2 21,686.2 34,428.0 3,097.7 4,047.8 84,111.0 21.2% 5 531.7 376.9 7.1 2,500.3 3,034.8 5,406.1 618.9 1,671.3 14,147.1 3.6% 6 188.2 223.1 7.4 2,348.4 3,122.8 6,231.8 467.9 727.4 13,317.0 3.4% Total 15,697.9 17,527.5 249.7 82,248.3 91,752.2 128,588.3 17,713.9 42,804.6 396,582.5 The distribution for strata (shown in Table 1.7) shows that 79.5% of the resources will be used for Stratum I, 17% for II, and the remaining 3.5% for Stratum III. Table 1.7. Resource needs to control malaria in Mesoamerica by country transmission levels (US$ thousans) Country Belize Costa Rica El Salvador Guatemala Honduras Mexico Nicaragua Panama Total % Stratum I US$x1000 % 4,388 1.4% 5,959 1.9% 250 74,715 87,427 118,845 11,439 12,191 315,213 79% 0.1% 23.7% 27.7% 37.7% 3.6% 3.9% 100% Stratum II US$x1000 % 10,794 16.0% 4,235 6.3% 7,245 4,057 6,353 4,446 30,292 67,422 17.0% 0.0% 10.7% 6.0% 9.4% 6.6% 44.9% 100% Stratum III US$x1000 % 516 3.7% 7,333 52.6% Total US$x1000 15,698 17,528 0.0% 2.1% 1.9% 24.3% 13.1% 2.3% 100% 250 82,249 91,753 128,589 17,714 42,805 396,583 289 268 3,391 1,830 321 13,947 3.5% Dengue Table 1.8 shows the results on unit costs for the interventions considered for the effective control of dengue throughout the region of Mesoamerica. The promotion activities, which include diverse and directed actions for obtaining active participation of the community in the control of dengue, were the most expensive, totaling up to US$2,307 in a community of 50,000 inhabitants. The hospitalization costs of patients with hemorrhagic dengue were the second most expensive intervention with US$116.30. Table 1.8. Unit costs for dengue interventions in the Mesoamerica region Intervention Expression of unit costs Cost in US$ 17 Vectors control interventions Intradomiciliar spraying Space spraying Household larval control Diagnosis inteventions Virus isolated Serology Hematology biometry Community participation interventions Promotion Treatment interventions Ambulatory health care Inpatient health care Cost per household controlled Cost per hectare treated Cost per household controlled 1.92 5.95 1.65 Cost per laboratory test Cost per laboratory test Cost per laboratory test 7.65 25.59 5.1 Cost per package by 50,000 people twice a year 2,307.15 Cost per case treated Cost per severe case treated 35.08 116.32 According to the results, the accomplishment of the dengue control activities requires an investment of US$63.3 million per year, of which approximately 63% of costs correspond to Mexico (See Table 1.9). Excluding Mexico, the total amount of resources required drops to US$23.7 million per year, with Nicaragua requiring approximately 21% of the total require investment. Table 1.9. Annual resources needed to confront dengue in Mesoamerica by country and by intervention (US$ thousands) Intradomicil iar spraying Costa Rica El Salvador Guatema la Hondura s Mexico Nicaragu a Panama Belice Total % Space sprayin g Househo ld larval control Virus isolate d Serolo gy Hematolo gy biometry Promoti on Ambulato ry health care Hospitala ry health care Total % 811.4 0.0 2,264.9 0.0 61.5 0.2 71.2 82.5 1.3 3,293.0 5.2% 1,513.9 41.2 2,283.8 2.9 201.0 1.1 71.8 143.7 8.2 4,267.5 6.7% 81.2 0.0 3,939.1 0.1 17.5 0.0 123.9 20.4 0.2 4,182.4 6.6% 459.5 135.3 3,006.5 0.2 38.6 10.0 94.5 42.0 75.8 19,167.6 280.0 15,696.7 12.7 1,765.0 33.4 493.5 1,835.4 254.0 3,862.5 39,538. 3 6.1% 62.5 % 1,203.9 530.1 1.5 130.5 70.2 0.0 3,245.2 2,311.6 115.8 0.6 0.3 0.0 102.9 46.6 0.1 2.8 0.0 0.0 102.0 72.7 3.6 113.4 48.5 0.1 21.4 0.2 0.0 7.8% 4.9% 0.2% 23,769.1 37.6% 657.2 1.0% 32,863.5 51.9% 16.9 0.0% 2,233.2 3.5% 47.5 0.1% 1,033.3 1.6% 2,286.1 3.6% 361.1 0.6% 4,922.6 3,080.3 121.1 63,267. 8 Table 1.10 that the at-risk localities with populations between 100,000 and 350,000 inhabitants will need US$32.6 million per year, an amount equivalent to 52% of the total necessary resources per year to anticipate and fight the consequences of the fastidiousness in the entire region. Nevertheless, after excluding Mexico, the total resource needs drops to US$23.7 millions. In both scenarios, the stratum for high-risk populations needed the largest percentage of resources (70% including Mexico and 57.5% without Mexico) (Table 1.11). Table 1.10. Annual resources needed for dengue control in Mesoamerica by level of risk and by population (US$ thounsands) Localities size/Risk <100,000 inhabitants 100,000 to 350,000 inhabitants >350,000 inhabitants Total Low risk Moderate risk 501 High risk Total 2,073 2,574 5,949 4,250 22,399 32,597 6,057 12,506 2,213 6,463 19,827 44,298 28,096 63,268 Table 1.11. Annual resources needed to dengue in Mesoamerica by level of risk and by population, excluding Mexico (US$ thounsands) 18 Localities size/Risk <100,000 inhabitants 100,000 to 350,000 inhabitants >350,000 inhabitants Total Low risk Moderate risk 0 High risk Total 121 121 2,895 3,332 3,691 9,918 3,867 6,761 0 3,332 9,824 13,636 13,691 23,729 Discussion: The results shown in the present study, aimed at informing the initiatives with the goals of achieving an effective control of dengue and malaria, has estimated that an annual investment of US$129.4 million will be required, of which 51.1% will be needed for the control of malaria. The country that pulled a considerable proportion of these costs was shown to be Mexico, and by excluding Mexico from the analysis, the investment total was reduced to US$68.4 million per year. By including malaria control activities and excluding dengue control activities for Mexico, the required annual total was shown to be US$89.8 million. The average cost per inhabitant comes out to be US$10.40 for malaria and US$1.30 for dengue. When excluding Mexico, the average cost per inhabitant is reduced to US$7.50 dollars for malaria and US$0.95 dollars for dengue. It was intended that unit costs be estimated for each country to calculate estimations with a high level of precision and specificity, while taking into consideration the national production factors and the national prices for the production factors. Though general parameters exist, contents in the guides of the international organizations (e.g. WHO, PAHO) and operation forms in reality differ among countries, which is to be expected. Nevertheless, the few resource and cost responses from the countries detailed in this report prevented the attainment of this objective, which is why these resource estimations by country may not reflect the necessities of each country in an individual way. However, since the strategy is focused on the Mesoamerican region and does not distinguish results by country, the exercise complies with the fundamental purpose of informing stakeholders the total resource requirements in the region to effectively control the effects of dengue and malaria. IMMUNIZATIONS Objective: To estimate resource needs to reach 95% vaccination coverage rates for the following biological vaccines in the Mesoamerica region: BCG1, DPT3, HepB3, Hib3, Sabin2 or IPV2, MMR1, PCV7-2 and Rotavirus2. Methods Interventions The Immunizations Working Group proposed a set of interventions in three different lines of action: (1) pilot projects to fill gaps in knowledge; (2) strengthening immunization policy; and (3) implementation of evidence-based practices. These lines of action are based on the idea that pilot projects can be used along with policy advancements to scale-up interventions through the 19 use of data-driven decision making. Taken from the master plan, Table A1 in the Annex shows the proposed effective practices or interventions, the process for implementation, geographical context, target population(s), scale, countries where practices were implemented, and sources for information. At the time of writing this report, there was not enough information to cost the pilot projects for filling key gaps in knowledge, since the policymakers in Mesoamerica together with technical experts had yet to determine the type and scope of pilot projects appropriate for their countries. The same can be said with respect to interventions aimed at strengthening immunization policy. Based on this, this report only estimates the incremental costs for reaching 95% vaccination coverage rates for the following biological vaccines in the Mesoamerica region: BCG1 (Bacille Calmette-Guérin), DPT3 (diphtheria, pertussis, and tetanus), HepB3 (Hepatitis B), 3 Hib (Haemophilus influenzae type B), OPV2 (oral polio vaccine, also known as the Sabin vaccine) or IPV (inactivated polio vaccine), MMR1 (measles, mumps, and rubella), PCV7-2 (heptavalent Pneumococcal conjugate vaccine) and Rotavirus2. The estimated costs included vaccine costs and scale-up costs for cold chain supplies, training and supervision, vehicles and transport, social mobilization, surveillance, monitoring and evaluation (M&E), waste management, personnel, and overhead costs. Vaccines costs included the costs for all the vaccines used in the national immunization program and were based on each country’s vaccination schedule for BCG1, DPT3, HepB3, Hib3, Sabin2 or IPV, and MMR1,vaccines as well as vaccines that will be newly adopted into the schedule, PCV7-2 and Rotavirus2. The vaccine costs included the vaccine price as purchased through the PAHO Revolving Fund (PAHO, 2009). Cold chain equipment costs included the annual capital cost of existing and newly purchased cold chain equipment specifically used for the purpose of the National Immunization Program. These costs typically consisted of the costs for freezers, refrigerators, cold boxes, and vaccine carriers. Training costs included short-term, in-service training expenditures for immunization activities that were reported to occur on a regular basis for any type of health staff involved (e.g. introductory training for new vaccines, injection safety, logistics, vaccine management). Vehicles costs included the annual value of existing vehicles that were being used specifically by the National Immunization Program. These typically consist of cars, four-wheel drive trucks, motorcycles, bicycles, and/or boats. Transport costs included the costs related to the operations and maintenance of vehicles for the delivery of vaccines, supplies, and immunization services (e.g. fuel). Social mobilization/IEC (information, education and communication) costs included all spending on social mobilization activities and materials for IEC regarding the benefits of immunization. Disease surveillance and monitoring: costs captured all spending for disease surveillance, as well as supervision and monitoring activities. Personnel costs included the salary and benefits of fulltime and program-specific personnel involved with the organization and delivery of immunization activities. Personnel costs also included per-diems and other incentives for service delivery and outreach activities. Maintenance and overhead costs included the maintenance costs of cold chain equipment and building overhead costs (e.g. electricity). 20 Vaccines costs Vaccines were estimated as ―bundled‖ costs for the purchased prices through the PAHO Revolving Fund. These costs covered safe injection supplies, such as, syringes and safety boxes. Adjusted for wastage based on vial sizes, shipping and freight were also included as a percentage of the price per dose as done by Wolfson et al. (2008), as shown in Table 2.1. Costs for disposable items (e.g. syringes, safety boxes) were based on 2005 international prices assuming 10% wastage for the auto-disposable syringes, reconstitution syringes, and safety boxes. Table 2.1. Vaccine costs Price per dose, US$ of 2009 0.1054 0.158 3.45 3.6 Average vaccine wastage rate (%)** % of vaccine price charged for freight Average vaccine wastage rate** BCG DTP 50 0.7 DTP-Hib 30 1.5 DTP-Hepatitis B-Hib 15 5.8 DTP-IPV-Hib 10 5.5 OPV 0.17 IPV 30 1.1 Measles / MMR 0.92 Hep B 0.2679 40 7.3 Hib 3.45 27.7 0 Rotavirus 5.5 15 9.5 Measles &Rubella 0.51 5 6 PCV7 21.75 40 7.3 Varicella 9.365 5 2.5 Hep A 7.3963 */Prices for Vaccines Purchased Through the PAHO Revolving Fund, 2009. Source: IMMUNIZATION NEWSLETTER, Volume XXXI, Number 1, February 2009 **/ taken from Bulletin of the World Health Organization 2008;86:27–39 For each vaccination strategy, the required number of doses was based on the appropriate target population (in this case, newborns), combined with the gap between current and desired coverage levels for each Mesoamerican country, where desired coverage rates were set at 95%. Table 2.2 shows the current immunization coverage rates by country. Since rotavirus and pneumococcus vaccines were recently introduced in Honduras, Mexico and Nicaragua and pneumococcus in Panama, we assumed that the current coverage rates were 50% for both rotavirus and pneumococcus vaccines based on recent estimations from Mexico. Table 2.3 shows the projected number of newborns that would remain unvaccinated if the vaccination coverage rates are maintained at these levels. Table 2.4 shows the additional number of newborns that should be reached to achieve 95% coverage rates for all the biological vaccines of interest. Table 2.2. Vaccination coverage rates in the Mesoamerican countries, 2005 21 Belize Costa Rica El Salvador Guatemala Honduras México Nicaragua Panamá Coverage BCG 96 88 84 96 91 99 99 99 Polio3 96 91 89 92 91 98 87 86 DPT1 97 89 89 99 88 99 92 95 DPT3 96 91 89 92 91 98 86 85 Hib3 96 89 89 39 91 98 86 85 Hep B3 96 90 89 39 91 98 86 85 MMR 95 89 99 93 92 96 96 99 MMR2 87 … 87 NA NA 97 NA 89 BCG: bacille Calmette-Guérin (anti-tuberculosis vaccine) Polio3: third dose of polio vaccine (oral polio vaccine or inactivated polio vaccine) DPT1: first dose of diphtheria-pertussis-tetanus vaccine (as DPT or combination vaccine) DPT3: third dose of diphtheria-pertussis-tetanus vaccine (as DPT or combination vaccine) Hib3: "third dose of Haemophilus influenzae type b (Hib) vaccine (as monovalent Hib or combination vaccine)" Hep B3: third dose of hepatitis B vaccine (as monovalent hepatitis B or combination vaccine) MMR: first dose of measles, mumps, rubella vaccine MMR2: second dose of measles, mumps, rubella vaccine (when offered in the routine program) Source: PAHO, Immunization in the Americas, 2006 summary. Available at http://www.paho.org/English/AD/FCH/IM/IMBrochure_2006.pdf Table 2.3. Projected number of newborns uncovered by vaccination (in thousands) Belize Costa Rica El Salvador Guatemala Honduras México* Nicaragua Panamá Total Total 1 newborns 7.0 79.5 165.6 438.1 206.9 601.8 153.9 70.1 1722.9 BCG 0.3 9.5 26.5 17.5 18.6 6.0 1.5 0.7 80.7 Polio3 0.3 7.2 18.2 35.0 18.6 12.0 20.0 9.8 121.2 DPT1 0.2 8.7 18.2 4.4 24.8 6.0 12.3 3.5 78.2 DPT3 0.3 7.2 18.2 35.0 18.6 12.0 21.5 10.5 123.4 Hib3 0.3 8.7 18.2 267.2 18.6 12.0 21.5 10.5 357.2 Hep B3 0.3 8.0 18.2 267.2 18.6 12.0 21.5 10.5 356.4 MMR 0.4 8.7 1.7 30.7 16.6 24.1 6.2 0.7 88.9 BCG: bacille Calmette-Guérin (anti-tuberculosis vaccine) Polio3: third dose of polio vaccine (oral polio vaccine or inactivated polio vaccine) DPT1: first dose of diphtheria-pertussis-tetanus vaccine (as DPT or combination vaccine) DPT3: third dose of diphtheria-pertussis-tetanus vaccine (as DPT or combination vaccine) Hib3: third dose of Haemophilus influenzae type b (Hib) vaccine (as monovalent Hib or combination vaccine) Hep B3: third dose of hepatitis B vaccine (as monovalent hepatitis B or combination vaccine) MMR: first dose of measles, mumps, rubella vaccine MMR2: second dose of measles, mumps, rubella vaccine (when offered in the routine program) */ includes just the newborns from the 10 states within the mesoamerican health initiative 1/Source: PAHO, Immunization in the Americas, 2006 summary. Available at http://www.paho.org/English/AD/FCH/IM/IMBrochure_2006.pdf Table 2.4. Number of newborns who need to be covered to reach 95% coverage rates by vaccine Costa El Belize Rica Salvador Guatemala Honduras México* Nicaragua Panamá Total BCG 0.0 5.6 18.2 0.0 8.3 0.0 0.0 0.0 32.1 Polio3 0.0 3.2 9.9 13.1 8.3 0.0 12.3 6.3 53.2 DPT1 0.0 4.8 9.9 0.0 14.5 0.0 4.6 0.0 33.8 DPT3 0.0 3.2 9.9 13.1 8.3 0.0 13.9 7.0 55.4 Hib3 0.0 4.8 9.9 245.3 8.3 0.0 13.9 7.0 289.2 Hep B3 0.0 4.0 9.9 245.3 8.3 0.0 13.9 7.0 288.4 MMR 0.0 4.8 0.0 8.8 6.2 0.0 0.0 0.0 19.7 BCG: bacille Calmette-Guérin (anti-tuberculosis vaccine) Polio3: third dose of polio vaccine (oral polio vaccine or inactivated polio vaccine) DPT1: first dose of diphtheria-pertussis-tetanus vaccine (as DPT or combination vaccine) DPT3: third dose of diphtheria-pertussis-tetanus vaccine (as DPT or combination vaccine) Hib3: third dose of Haemophilus influenzae type b (Hib) vaccine (as monovalent Hib or combination vaccine) Hep B3: third dose of hepatitis B vaccine (as monovalent hepatitis B or combination vaccine) MMR: first dose of measles, mumps, rubella vaccine */ includes just the newborns from the 10 states within the mesoamerican health initiative Table 2.5 shows the current vaccination schedules for each of the Mesoamerican countries. As depicted in the table, different countries in the 22 region use different combination vaccines. To achieve 95% coverage rates for each biological, this suggests that different countries will be required to buy different vaccines, respective of their schedules. For example, all countries except Costa Rica, use the combined vaccine DTP-Hepatitis B-Hib, while Costa Rica uses separate DTP, Hepatitis B and Hib vaccines. Table 2.5. National immunization schedules for all Mesoamerican countries BCG DTP DTP-Hib DTPHepatitis B-Hib DTP-IPVHib OPV IPV Measles / MMR Hep B Mexico 2009 NB Guatemala 2007 NB Belize 2008 NB El Salvador 2007 NB Honduras 2008 NB Nicaragua 2007 NB 4y 1.5y,5y 4 years 1.5y,4y 1.5y,4y 1.5y 2m,4m,6m 2m,4m,6 m 2m,4m,6 m 2m,4m,6 m 2m,4m,6m, 1.5y,4y 2m,4m,6 m, 4y 2m,4m,6 m,1.5y,4y 2m,4m,6 m,1.5y,4y 2m,4m,6 m 1y 1y, 2y 1y,4y 1y NB,1m,7 m 1y 2m,4m,6 m 2m,4m,6 m,1.5y 1y,6y NB,2m,4 m Hib Rotavirus Measles &Rubella 2m,4m 2m,4m Costa Rica 2008 NB 2m,4m,6 m,1.25y,4 y Panamá 2007 NB 2m,4m,6 m 4y 1.5y DTPHepatitis B-Hib 2m,4m,6 m,4y NB,2m,4 m,6m,1.5 y,4y 1.25y,esc uela NB,2m,6 m 2m,4m,6 m,1.25y 2m,4m,6 m 1y,4y NB 2m,4m 1y-4y 2m,4m,6 m 2m,4m,6 PCV7 2m,4m,1y m Varicella Hep A BCG: bacille Calmette-Guérin (anti-tuberculosis vaccine) DPT: diphtheria-pertussis-tetanus vaccine Hib: haemophilus influenzae type B vaccine Hep B hepatitis B vaccine OPV: oral polio vaccine IPV: inactivated polio vaccine MMR: measles, mumps & rubella vaccine PCV7 heptavalent Pneumococcal Conjugate Vaccine Hep A hepatitis A vaccine m: months of age; y: years of age */Prices for Vaccines Purchased Through the PAHO Revolving Fund, 2009. Source: IMMUNIZATION NEWSLETTER, Volume XXXI, Number 1, February 2009 **/ taken from Bulletin of the World Health Organization 2008;86:27–39 1y 1.5y Scaling-up Non-vaccine costs of scaling-up capacity to increase vaccination coverage rates for existing vaccines and new vaccines was obtained from Wolfson et al. (2008). Departing from their system for estimating scale-up costs (nonvaccine costs) in low- and middle-income countries, we estimated nonvaccine scale-up cost per child born (US$8.50), and used it for our estimations in the Mesoamerican countries. In estimating costs of scaling-up, Wolfson et al. used country-specific variables to define likely production function rules for each component (2008). The main assumptions and variables Wolfson et al. (2008) used for each component (both capital and recurrent costs) were derived from various 23 sources, including: a country classification used by McKinsey & Company management consulting firm in a report to the GAVI Alliance on barriers to improved performance in immunization systems (McKinsey, 2004), the Commission on Macroeconomics in Health infrastructure index (Ranson et al. 2003), a transportation index based on available modes for transportation and communication (Limao et al. 2001), as well as district-level vaccine coverage and country-reported, immunization-specific indicators (WHO 2005). The McKinsey & Company’s classification categorizes countries into three types: TU or ―turn around‖ countries, which are low performers where major system strengthening is required; SI or ―strategic intervention‖ countries, which are middle performers in need of targeted interventions; and SA or ―stand alone‖ countries, which are higher performers with good infrastructure. The classification is based on an assessment of political and financial commitment, physical infrastructure and equipment availability, monitoring and information systems, human resource availability, and social mobilization strategies (McKinsey, 2004). Additionally, non-vaccine costs for scale-up were broken down into the following cost categories using the estimated distribution reported by Wolfson et al. (2008) for the WHO Region of the Americas: cold chain (20%), training and supervision (31%), vehicles and transport (11%), social mobilization (13%), surveillance and M&E (10%), waste management (1%), personnel (9%), and overheads (5%). Results Table 2.6 shows the estimates for the resources needed to vaccinate a cohort of newborns each year and by country, according to the type of vaccine and scaling-up cost concept. According to the results, an estimate of US$109.5 million would be required to reach 95% vaccination coverage rates for all biologicals, including new vaccines (rotavirus and pneumococcus). Of the US$109.5 million, 0.5% would be required to fill the coverage gap for currently in-use vaccines, while 86.1% of the costs would go towards introducing the new vaccines, and the remaining 13.4% corresponds to system scale-up (non-vaccine costs). The resource needs by county are as follows: US$0.59 million for Belize, US$6.82 million for Costa Rica, US$14.17 for El Salvador, US$37.2 for Guatemala, US$9.8 for Honduras, US$28 for Mexico, US$7.3 for Nicaragua, and US$5.6 for Panama. Discussion Estimates presented here rest on the current available data on coverage rates, which are thought by the experts that need further validation. As pilot projects are implemented and coverage rates are validated, it will allow us to project more reliable estimates. Projections presented here were done without an appropriate assessment of the infrastructure availability and current capacity utilization levels as well as an appropriate assessment of the current human capacity availability. Both diagnostics are essential to accurately estimate non-vaccine costs of scalingup. 24 It is also important to mention that hereby we are no costing the pilot projects to fill gaps in knowledge, nor the needed interventions for strengthening immunization policy that would be required for achieving the objectives of the MHI in its immunization component. 25 Resource Needs to reach 95% coverage rates of vaccination in a birth cohort in the Mesoamerican region Costa Rica El Salvador BCG Polio3 DTPHepatitis BHib 1 DTPHepatitis BHib 3 MMR in use vaccines 0 0 Belize NA NA 0.9 2.1 (1.1) (2.7) 2.9 8.9 (2.1) (6.5) 0.0 11.7 (0) (15) 1.3 7.4 (0.8) (4.3) 0 0 NA NA 0.0 8.2 (0) (8.5) 0.0 7.0 (0) (19.4) 5 45 (0.9) (7.6) 0 NA 47.2 (59.6) 82.6 (60.9) 0.0 (0) 120.4 (70) 0 NA 38.4 (39.8) 0.0 (0) 289 (48.3) 0 0 NA NA 22.5 6.5 (28.4) (8.2) 41.3 0.0 (30.4) (0) 54.6 11.9 (69.8) (15.2) 34.4 8.4 (20) (4.9) 0 0 NA NA 49.9 0.0 (51.7) (0) 29.1 0.0 (80.6) (0) 232 27 (38.8) (4.5) 0 NA 79 1.2 136 1.0 78 0.2 172 1.8 0 NA 96 1.3 36 0.6 598 0.5 Rotavirus Neumococo New vaccines Total vaccines 77.0 456.8 (14.4) (85.6) 874.5 5,187.4 (14.4) (85.6) 1,821.6 10,805.4 (14.4) (85.6) 4,819.1 28,586.0 (14.4) (85.6) 1,138.0 6,750.1 (14.4) (85.6) 3,309.9 19,634.0 (14.4) (85.6) 846.5 5,021.0 (14.4) (85.6) 385.6 4,574.0 (7.8) (92.2) 13,272 81,015 (14.1) (85.9) 534 90.0 6,062 88.9 12,627 89.1 33,405 89.8 7,888 80.3 22,944 81.8 5,867 80.7 4,960 88.7 94,287 86.1 534 90.0 6,141 90.1 12,763 90.1 33,483 90.0 8,060 82.1 22,944 81.8 5,964 82.0 4,996 89.3 94,885 86.6 Cold chain Training & supervision Vehicles and transport Social mobilization Surveillance, M&E Waste management Personnel Overheads Costs of scaling-up 11.9 (20) 135.2 (20) 281.5 (20) 744.8 (20) 351.7 (20) 1,023.1 (20) 261.6 (20) 119.2 (20) 2,929 (20) 18.4 (31) 209.5 (31) 436.4 (31) 1,154.4 (31) 545.2 (31) 1,585.8 (31) 405.5 (31) 184.7 (31) 4,540 (31) 6.5 (11) 74.3 (11) 154.8 (11) 409.6 (11) 193.5 (11) 562.7 (11) 143.9 (11) 65.5 (11) 1,611 (11) 7.7 (13) 87.8 (13) 183.0 (13) 484.1 (13) 228.6 (13) 665.0 (13) 170.1 (13) 77.5 (13) 1,904 (13) 6.0 (10) 67.6 (10) 140.8 (10) 372.4 (10) 175.9 (10) 511.5 (10) 130.8 (10) 59.6 (10) 1,464 (10) 0.6 5.4 3.0 (1) (9) (5) 6.8 60.8 33.8 (1) (9) (5) 14.1 126.7 70.4 (1) (9) (5) 37.2 335.1 186.2 (1) (9) (5) 17.6 158.3 87.9 (1) (9) (5) 51.2 460.4 255.8 (1) (9) (5) 13.1 117.7 65.4 (1) (9) (5) 6.0 53.6 29.8 (1) (9) (5) 146 1,318 732 (1) (9) (5) 59.5 10.0 675.8 9.9 1,407.6 9.9 3,723.9 10.0 1,758.7 17.9 5,115.4 18.2 1,308.2 18.0 595.9 10.7 14,645 13.4 Total 593.3 6,816.8 14,170.3 % of the grand total 0.54 6.22 12.94 BCG 0 NA 0.9 (1.1) 2.9 (2.1) 1/Number in parentheses indicate percentages within their categories. Guatemala Honduras México* Nicaragua Panamá 37,207.2 9,818.7 28,059.3 7,272.1 5,591.6 33.97 0.0 8.96 1.3 25.62 0 6.64 0.0 5.11 0.0 (0) (0.8) NA (0) Total 109,529.3 (0) 5 (0.9) 26 NUTRITION Methods To address the main nutrition problems in the Mesoamerica region, the Nutrition Technical Group recommended ten selected practices that have demonstrated efficacy or effectiveness in many countries for reducing stunting and micronutrient deficiencies and for improving maternal, neonatal, and child health outcomes related to nutrition. For the purpose of this costing exercise, the proposed effective practices were enumerated and are shown in Table 3.1 with its respective target population. Table 3.1. Nutrition interventions Intervention Nutrition Education 1. Promotion of breastfeeding and appropriate complementary feeding practices U n i v e r s a l a. Breastfeeding promotion and support. b. Complementary feeding promotion (not provision of food ). Details Target Group Costed delivery platform(s) a. Primary health care system. b. Communication campaign. c. CCTs or/and C-BPs. Individual and group counseling about adequate breastfeeding and complementary feeding practices. Pregnant mothers/ parents of infants under 6 months of age and children under 2 years of age. Improved hygiene. Counseling about food safety, use of soap, hand washing, etc. Improved water and sanitation Improve water quality (use of bleach, filters). Populations with high prevalences of infectious diseases and to areas where water safety is not guaranteed CCTs or/and Community Nutrition Programs. Iron-folate supplements. Pregnant women. Primary health care system. Maintain and strengthen ongoing universal food fortification programs (example: flour, sugar or salt fortification). Entire population. Market-based delivery systems. 5. Vitamin A supplementation Biannual supplementation of megadoses of vitamin A. Children 6-59 months of age, from poor rural areas and urban slums and indigenous and afrodescendant populations. Vaccination campaigns. 6. Therapeutic zinc supplements Use of 10 to 14 day treatment course with zinc as part of the standardized treatment for diarrhea. Children under the age of 5 in areas with high prevalences of infectious diseases and evidence of zinc deficiency. Primary health care system. Micronutrient powders for home fortification. Children younger than 2 years in low-income households. CCTs or/and Community Nutrition Programs. Severe primary undernutrition cases. Primary health care system. Populations with high prevalence of children 6-24 months of age with WAZ< - 2SD. CCTs or/and Community Nutrition Programs. 2. Improved water, sanitation and hygiene behaviors Micronutrients 3. Prenatal micronutrient supplements 4. Food fortification programs a. Iron supplements b. Folic acid supplements Micronutrient fortification of staples/other foods Micronutrients 7. Multiple micronutrient powders L o c a l i z e d Complementary and Therapeutic Feeding 8. Clinical management of severe acute malnutrition (SAM) 9. Fortified complementary food Use of standardized, evidencebased protocols to manage severe acute malnutrition at a clinical setting. Identification of circumstances in which food supplementation is needed. Provision of complementary food in these circumstances. Related interventions 10. Conditional Cash Transfers (CCT) Interventions and target populations The practices were grouped in three different packages targeted to different populations, and one core group of cost-effective interventions was recommended for national level implementation. In the core group, the practices for universal coverage included: counseling for breastfeeding and adequate complementary feeding practices, food supplementation with 27 vitamin A, therapeutic zinc supplementation, hygiene promotion, prenatal supplements, and fortification of staple. Two other intervention packages were proposed to reduce undernutrition in areas with high prevalences of stunting, micronutrient deficiencies, food insecurity, and poverty. In addition to the basic core of interventions, the first package includes conditional cash transfer (CCTs) programs and the provision of fortified complementary foods. The second package includes the basic core interventions plus fortified complementary foods or micronutrient powders, which is considered a less costly intervention for effectively reducing stunting. Finally, the recent emergence of cases of severe acute malnutrition in Guatemala due to extreme climate conditions motivated the inclusion of clinical management of severe acute malnutrition (SAM), which has demonstrated efficacy, as part of the proposed interventions. Delivery Platforms The costs of the nutrition interventions depend on the systems through which they are delivered (Horton, Sheekar et al. forthcoming). Each of the selected interventions for nutrition possessed a variety of delivery platform possibilities that targeted different population groups and required different personnel and supplies. There were five delivery platforms considered for implementing the nine proposed interventions. Interventions are proposed to be delivered through one or more of the following: the primary health care system, vaccination campaigns, market-based systems, communication campaigns and/or CCTs or Community-Based Nutrition Programs (C-BPs). For costing purposes, each intervention was placed within a delivery platform that was considered most appropriate and feasible (see Table 3.2). 28 Delivery Platform Intervention ID · Promotion of breastfeeding and 1 appropriate complementary feeding practices. 3 1 Primary health care system. · Prenatal micronutrient supplements/ iron and folic acid. 6 · 8 2 3 Vaccination campaigns. Market-based delivery. Conditional Cash Transfer Programs / 4 Community-Based Nutrition Programs. 5 Communication campaigns. Therapeutic zinc supplements. Children under 2 years old. Pregnant women. Children under the age of 5 years in areas with high prevalences of infectious diseases and evidence of zinc deficiency. In poor rural areas and urban slum and indigenous and afro-descendant population. In poor rural areas and urban slum and indigenous and afro-descendant population. Areas with high prevalences of infectious diseases and evidence of zinc deficiency. · Clinical management of Severe Acute Severe primary undernutrition cases. Malnutrition (SAM). 5 · Vitamin A supplementation. · Fortification of staple food (Salt 4 iodization, sugar with vitamin A, wheat, maize, rice, vegtable oil). · Promotion of breastfeeding and 1 appropriate complementary feeding practices. · Improved water, sanitation and 2 hygiene behaviors. 7 Target population Children 6-59 months of age. National level. All populations in the region. National level. Children under 2 years old. High prevalences of infectious Low income population where water diseases and to areas where water safety is not guaranteed. safety is not guaranteed. · Distribution of micronutrient powders Children 6-24 months of age. for children 6-24 months of age. · Complementary food (delivery of 9 complementary food) for children 6-24 months of age. · Promotion of breastfeeding and 1 appropriate complementary feeding practices. Low-income households in rural areas and urban slums. Children 6-24 months of age. Low-income households in rural areas and urban slums. Children under 2 years old. National level. Instead of considering CCTs as a single intervention for the program, it was considered as a delivery platform. CCT programs can support nutrition improvement, but they were not costed in this document. This is because they often have multiple components aiming to address multiple objectives, such as, reducing household vulnerability and breaking the intergenerational transmission of poverty, not contained within the scope of the Mesoamerican initiative. However, it is important to address the situations where CCTs have previously been instituted, where nutrition interventions targeted to lowincome populations could be delivered through already-existing CCT mechanisms at a lower cost. Several of the selected interventions have the potential to be delivered simultaneously through several of the aforementioned platforms. For example, the vitamin A intervention can be delivered simultaneously through the health care system and through vaccination campaigns; however, for this analysis, it was costed only through vaccination. In communication campaigns, which can promote any education message, such as, hygiene or prenatal supplements, it is reasonable to assume that the cost of a campaign does not vary according to the message, but rather according to the media and exposure time. Because of this, breastfeeding promotion was selectively costed in this platform and was then extrapolated to other platforms. Across the program, breastfeeding promotion and complementary feeding practices was the only practice costed for three different delivery platforms simultaneously – primary health care system, communication campaign and though CCTs or C-BPs. Grouped by delivery platforms, eleven interventions were costed (see Table 3.2). 29 Results For resource inputs costs, data from Mexico, Panama, Nicaragua, and Guatemala were obtained through data collection instruments filled out by each country. In addition, information on quantities came from WHO guidelines, literature, and expert opinion: complementary information on prices came from WHO-CHOICE1 and published literature. Incremental costs for the interventions are presented in Table 3.3 and described below. 1 Within WHO-CHOICE classification regions AMR B includes Belize, Costa Rica, El Salvador, Honduras, Mexico and Panama and AMR D includes Guatemala and Nicaragua. 30 Five years incremental costs 4. Food fortification programs 2009 US$ in millions Guatemala Food Private sector costs Mexico Public sector Total Private + costs Public sector costs Sugar Vegetable oil Wheat flour Maize flour expanded fortification package Maize flour reduced fortification package 14.00 0.97 14.97 Private sector costs Total Private + Public sector Public sector costs costs 174.54 136.08 1.03 1.27 175.57 137.35 0.87 1.10 1.97 11.35 1.45 12.79 367.97 10.05 378.02 3925.60 97.23 4022.82 156.32 9.78 166.10 1667.66 96.95 1764.62 Reduced package: iron, folic acid and vitamin B-12 Expanded package: Includes reduced package + vitamins B-1, B-2, B-3, B-6, vitamin A, and zinc Sugar and vegetable oil, only vitamin A was included Source: Fiedler and Macdonal (forthcoming) 1. Promotion of breastfeeding and appropriate complementary feeding practices Promoting exclusive breastfeeding within the first hour of birth and continued exclusive breastfeeding for 6 months after childbirth has been shown to be one of the most cost-effective nutrition health interventions. Continued breastfeeding beyond six months should be accompanied by consumption of nutritionally adequate, safe, and appropriate complementary foods that help meet nutritional requirements when breast milk is no longer sufficient (UNICEF 2008). These two interventions are heterogeneous in design; thus, their costs depend largely on program planning and implementation. 1.1 Primary health care system Within its primary health care system, the Nicaraguan Ministry of Health has been working with the Mother Baby Friendly Health Units Initiative (MBFHI). Taking into account the costs for seven health centers, the average cost of certifying a hospital to be Baby Friendly was US$6,489 per health center, and the average cost of monitoring was US$375 (Nicaragua contact). With the ingredients approach, the estimated incremental cost (including time per medical officer and nurse plus materials, such as laminates and flyers) for breastfeeding promotion was estimated to be US$4.29 for Mexico and US$4.79 for Panama. For other countries, information was not available for inputs, and total results may be somewhat underestimated. Training is an essential component of this intervention. It may include videos and teaching 31 packs for pediatric and medical staff. A training workshop cost around US$450 per 15 health personnel (see Table 3.3). 1.2 CCTs or/and C-BPs Delivered with Community-Based Programs (C-BPs), breastfeeding is more focalized, but resulted in a higher cost. Fiedler (2003) (Fiedler 2003) did a very detailed, activity-based costing analysis of the Honduras CommunityBased Integrated Child Health Program AIN-C. He estimated a recurrent cost of US$8.16 per child per year. 1.3 Communication campaign Finally, based on media costs from WHO-CHOICE and costs from Panama, a 4-month, television and radio communication campaign based on short spots (20 seconds) within the districts was estimated to cost around US$120,670 dollars. An example of the amount of resources needed for a health-related communication campaign can be taken from the 10-week, national campaign for HIV/AIDS in El Salvador ―Unámonos contra la discriminación", which costed US$400,000 (Gesaworld 2006). Thus, depending on the duration and specific communication channels (e.g. national or district television, radio channels) the cost may vary widely. Countries thus need to select a specific communication strategy that fits within their goals and their available modes of communication. 2. Improved water, sanitation, and hygiene behaviors Hygiene promotion, basic sanitation facilities, and water supply (water for domestic purposes) are well recognized to reduce morbidity. The simple measure of washing hands with soap has shown to be associated with a reduction of 43 percent in diarrheal disease (Curtis and Cairncross 2003). However, the cost of such an intervention significantly varies depending on its magnitude (ingredients). Therefore, it is suggested that countries define what will be included according not only to local needs but also to budget constraints. For the costing analysis, two basic packages were considered. The first involves hand washing with soap, filters, or chlorine for water improvement education. This practice might be included as an extra subject for CCTs (already in Mexico through Oportunidades program workshops) or C-BPs), which would have an estimated minimal incremental cost of US$0.34 per child, including the incremental time of the personnel plus extra educational materials per child. The second package involved the construction of basic sanitation facilities (excreta disposal, such as household pit latrine). This intervention, according to the Global Water Supply and Sanitation Assessment 2000 Report, cost US$60 per capita for Latin America. Taking a relatively short lifetime of five years for a latrine and straight-line amortization resulted in an annual cost of US$12 per capita per year (Cairncross and Valdmanis 2006) 32 3. Prenatal micronutrient supplements During pregnancy, a woman’s daily intake requirements for certain nutrients, such as folic acid (folate) and iron, increases. Prenatal micronutrient supplementation is a standardized intervention, and across the countries within this initiative, the dose period varies. For calculations routine supplementation tablets containing 60 mg elemental iron once daily for 14 months and 0.4 mg/d folic acid daily for 12 months was recommended for every pregnant woman. The costs included iron and folic acid supplements in addition to the time of the medical practitioner. The cost of this intervention is mainly the cost of the supplements which varies slightly through countries. On average, it cost $US7.00 per pregnant woman. 4. Universal food fortification programs Cost for fortification — the addition of micronutrients to a processed food to improve the food’s nutritional quality — depends largely on the micronutrient used to fortify, the food vehicle chosen for fortification, and industry structure of the food that is fortified. The staples food candidates for being fortified in the Mesoamerican region identified were: (1) sugar fortified with vitamin A; (2) vegetable oil fortified with vitamin A; (3) salt iodization; (4) maize foritified with iron and folic acid; and (5) wheat flour fortified with iron and folic acid. For costing universal food fortification programs, it is needed to select the specific food vehicle and analyze the consumption of the product as well as the conditions of the industry that produce it. J. Fiedler and Macdonald are working in a forthcoming paper which will cost the fortification of maize flour, wheat flour, sugar, and vegetable oil for 48 countries including Guatemala and Mexico. The estimates for Guatemala and Mexico from their study are presented in Table 3.3. For Guatemala, sugar fortification was not costed in this report since a current country program with adequate coverage exists. Guatemala reported to have a cost of US$1.00 per metric ton/per year, including both public and private costs (Guatemala contact). For Mexico, Fiedler and Macdonald (forthcoming)(Fiedler and Macdonald forthcoming) estimate the total incremental costs of a 5-year sugar fortification program in Mexico to be US$ 175.6 million, including both private and public sector costs. What was of interest for us were the private sector’s incremental costs — those additional costs that the private sector is expected to incur due to fortification. Those costs were estimated in US$1.03 million for the first 5 years. Wheat flour fortified with iron and folic acid and iodized salt are currently operating in Guatemala (Guatemala contact), and public sector costs of fortifying wheat flour were estimated to be US$1.10 million for five years. As depicted in Table 3.3, the cost of fortifying maize was found to be more than ten times the cost of fortifying wheat flour, vegetable oil, or sugar. This is mainly due to the characteristics of the maize flour industry which has significant variations in technology, plant sizes, economies of scale, and, hence, costs. 33 Moreover, Panama reported having salt (iodized) and wheat and maize flour (fortified with iron and folic acid). The incremental costs of such programs were not identified since they are absorbed by the private sector (Panama contact). 5. Vitamin A supplementation Vitamin A supplementation has demonstrated efficiency and costeffectiveness in reducing childhood mortality. According to the WHO, the recommended doses of vitamin A supplementation for the prevention of vitamin A deficiency for infants aged 9-11 months is a megadose (100,000 IU), and for children aged, 1–4 years 200,000 IU. The optimal interval between doses is four to six months. A dose should not be given too soon after a previous dose of vitamin A supplement (the minimum interval is one month) (WHO 2003). Calculations were based on two megadoses per year. This intervention can be delivered using the primary health care system, supplemented by some form of outreach, such as vaccination campaigns. Since the fixed costs for vaccination campaigns are not expected to vary, the costs of providing vitamin A in campaigns and primary health are considered comparable for the purposes of this document. The cost per dose of vitamin A ranges from $0.01 (Mexico contact) to $0.46 (Nicaragua contact). The supplement costs plus the health staff time and informational material was estimated for this intervention in US$1.72. 6. Therapeutic zinc supplements Zinc supplementation has a considerable beneficial effect on the clinical course of acute diarrhea as an adjunct therapy to oral rehydration solution (ORS) (Robberstad, Strand et al. 2004). The standard recommended treatment is one tablet of 20 mg/day of zinc for 14 days. The cost of the supplement significantly varies across countries from US$1.12 (Guatemala) to US$8.23 (Mexico) per treatment. Within this scheme, the intervention cost, which includes the supplement plus the general practitioner’s time to diagnose, varies in function to the cost of the zinc tablets. The average cost is US$5.36 per treated child with diarrhea. 7. Multiple micronutrient powders Costs for micronutrient powders — easily sprinkled onto foods prepared at home to provide the daily requirements — varies from US$0.015 to US$0.038 per sachet. A home fortification regimen consists of 60 single-dose sachets for each child (6-24 months of age), consumed over 60 to 120 days, not exceeding one sachet per day. The costs for distributing this product in already focalized CCTs programs or C-BPs contain a slightly increasing cost for distributing the micronutrient supplement. On average, the incremental costs of delivering micronutrient powders per child was estimated to cost US$2.66, including twice the human resources costs since it is delivered twice per year (Guatemala and Nicaragua contact). 34 8. Clinical management of severe acute malnutrition (SAM) Severely malnourished children — visibly severe wasting, with very low weight for height (below 3 z-scores of the median) or with the presence of nutritional edema — need special urgent care. The standard treatment protocol for managing this condition is a medically intensive treatment in hospital settings(WHO 1999). A severely undernourished child normally needs to be treated, in addition to nutrition restoration, to avoid many potential fatal complications, such as, hypothermia, hypoglycemia, sepsis, as well as associated conditions, such as, vitamin A deficiency, dermatosis, parasitic worms, and diarrhea, which increase the likelihood of contracting infections. To cost this intervention, all inputs for treatments addressing potential complications, infections, and related conditions were identified based on WHO guidelines for managing SAM. The cost of this intervention mainly depends on the number of days the patient remains in hospital, rather than the number of complications, since medicines for treating all complications are fairly similar in prices and do not represent a high percentage of the total cost. Thus, a ―best‖ and ―worst‖ case scenarios were modeled. Since it has been recognized that managing SAM lasts for 3 to 7 days, the worst-case scenario assumes that the patient is hospitalized for seven days and the best case assumes hospital discharge after three days. Clinical management of a severe acute malnourished child is estimated to range from US$201 to US$349. 9. Fortified complementary food - Prevention/treatment of moderate malnutrition. After the period of exclusive breastfeeding (6 months), complementary food should be varied to fulfill the requirements of energy and micronutrients, and in the situation of food insecurity, the use of fortified complementary food may be necessary to ensure adequate intake levels of particular nutrients(WHO 2002). The cost of this intervention varies especially according to the fortified complementary food that a country utilizes. Soy-based fortified food blends are often less costly, ranging from US$12.11 (Honduras Papilla CSB) to US$46.14 (Nicaragua cereal CSB) to feed a child during the period of 6 to 24 months of age. The most expensive types of complementary food are fortified milks, which ranges from US$98.62 (fortified milk in Costa Rica) to US$110.15 (Tenutre in Mexico) to meet the daily requirements during the 624 month age range. The other fortified complementary foods, with the exception of Incaparina in Guatemala which only costs US$10 dollars, are captured within this range. Since this complementary food would be delivered through any of the already CCTs or the C-BPs, the cost of the intervention consists of the fortified food plus extra human resources required to hand out and explain the feeding procedure to the mother/parents of the 6- to 24-month old child. The estimated cost per country is presented in table 3.3, which logically varies depending on the fortified food used. 35 Discussion As expected, interventions with the highest direct costs were the clinical management of severe acute malnutrition and fortified complementary foods, while the less expensive interventions were the micronutrient interventions. An important limitation of this study was the lack of price information for health inputs from most of the Mesoamerican countries. Because of this, it was necessary to impute average costs from the countries which information was available. The direct incremental costs presented here are useful for the countries wishing to more accurately define the interventions planned for implementation and with the information provided for making a diagnosis of the population already covered, it would be possible to estimate the global budget required per country to scale-up interventions. MATERNAL, NEONATAL AND REPRODUCTIVE HEALTH Methods Interventions The most important goals in this area were to reduce maternal mortality by 75%, reduce neonatal mortality by 50%, and achieve universal access to reproductive health services including family planning by the year 2015, in line with the United Nations 2009 Millennium Development Goals (MDG) report. The main interventions proposed in the area of maternal and newborn health were (also in Table A2 in the Anexx): Maternal health: implementation of basic Emergency Obstetric Care (EmOC), and interventions aimed at improving care of obstetric emergencies related to infections, eclampsia, hemorrhage and abortion; and community awareness, education and training to improve these outcomes. Neonatal health: essential newborn care, care for the low birth weight newborn and emergency care for newborns with complications. Reproductive health and family planning: implement quality family planning services for adolescents; ensure access to counseling and services for at least six contraceptive methods ensure access to vasectomy, and post-partum and post-abortion contraceptive counseling and services. In this section we intend to offer basic information related to the direct costs of the list of maternal and newborn interventions defined in the master plan. This information will be a useful ingredient for countries to make projections of the potential costs of investment in specific maternal and newborn health interventions and the costs of reducing gaps in health. We will also disaggregate the direct cost into its various components to identify the items of greatest financial burden for each health intervention. Information on input costs was requested to all the countries in the Mesoamerican region, however we just got data from Guatemala, Mexico, 36 Nicaragua and Panama. Therefore, we intend to develop an exercise to estimate direct incremental costs of each intervention included in the master plan for those four countries in Mesoamerica. Costs analysis Direct costs were collected through the use of input tables consist of medicines, personnel, personnel time invested in each intervention. These tables were developed with information from experts in obstetric and neonatal care in Mexico. This information served as a reference for shaping the information requested to each team of the Mesoamerica country network (See supplemented excel file 4.1). Two aspects were considered to develop the input tables: i) verification of the use of health resources in each intervention according to what was suggested by the literature; ii) interviews to experts in obstetric and neonatal care. The former was used to build the input matrix for each health intervention. The second required to perform semi-structured interviews (Henández-Sampieri, 1999) to physicians and nurses working in maternal and newborn health services areas from hospitals and clinics. Interviews were carried out in September 2009 in the Women’s Hospital in Yautepec, Morelos and the Mexican Institute of Social Security (IMSS) located in Cuernavaca, Morelos. The costs of maternal and newborn interventions were estimated using the Mother Baby Package (MBP) developed by the World Health Organization. The model was developed in the Excel and it contains dynamic cost sheets to estimate different types of costs. The MBP allowed us to estimate costs that can be disaggregated in different type of inputs such as medicines, working-hours, medical inputs, vaccines, laboratory inputs and infrastructure. In this study we focused on estimating the costs related with the use of medicines, working-hours and health inputs. By using the MBP it is possible to obtain direct cost per each intervention: normal delivery, haemorragia, eclampsia, sepsis, family planning including oral contraceptives, injectable contraceptives, condoms, intrauterine device (IUD), vasectomy, sub-dermal implant (Norplant). It is possible to obtain information by type of costs: variable and capital costs. In this study capital costs were not included. Finally it is possible to report costs by level of care; hospital or health centre. Additionally we estimated manually the cost of neonatal complications such as hypoxia and neonatal asphyxia; as well as manual vacuum aspiration (MVA). All costs estimates were converted into dollars of 2009. Results Panama Direct costs per intervention from Panama are reported in Table 4.1. The greatest cost was the cost for sepsis care at a cost of US$1,112, follow by manual vacuum aspiration (MVA) at a cost of US$475.40 and eclampsia at a cost of US$217.30. The lowest cost was for oral contraceptive at a cost of US$0.2 dollars. 37 For the costs per type of health input, in most of the interventions the highest costs are represented by consumable health supplies. The exceptions are two contraceptive methods: IUD and the sub-dermal implant (see Table 4.1). Direct costs for hypoxia and asphyxia were not estimated because we did not have information regarding the input costs in this country. Table 4.1. Direct unit costs per intervention for Panama in 2009 US dollars. Consumable Supplies Maternal Normal Delivery 15.63 (40.3%) Maternal complications Eclampsia 61.44 (28.3%) Hemorrhage 37.05 (64.8%) Sepsis 942.27 (84.7%) Manual vacuum aspiration (MVA) 474.69 (98.8%) Family Planning FP- Oral FP- Condom 5.56 (98.1%) FP- Injection 0.08 (2.3%) FP- IDU 5.06 (28.3%) FP- Sterilization 8.08 (75.3%) (1) FP- Norplant 0.92 (0.7%) Medicines Health Personnel Total Direct Costs 7.59 (19.6%) 15.59 (40.2%) 38.80 10.6 (4.9%) 13.62 (23.8%) 126.17 (11.3%) 145.3 (66.9%) 6.51 (11.4%) 43.56 (3.9%) 217.30 57.20 1,112.00 0.01 (0.0%) 0.74 (0.74%) 475.40 0.02 (10.8%) 0.16 (89.2%) 0.11 (1.9%) 0.16 (4.6%) 0.22 (1.2%) 0.83 (7.8%) 0.62 (0.5%) 0.20 5.70 3.50 17.80 10.70 126.1 3.30 (93.2%) 12.60 (70.5%) 1.81 (16.9%) 124.54 (98.8%) 1. The price of the sub-dermal implant from Panama was taken from the price reported by Mexico. Mexico Direct cost estimations per type of intervention in Mexico are shown in Table 4.2. The health care service with the highest costs was sepsis at a cost of US$858, followed by care for eclampsia at a cost of US$328 and hemorrhages at a cost of US$69. Note that medicine in this country represented the greatest financial burden within the direct costs of most of the interventions. Table 4.2. Direct unit costs per intervention for México in 2009 US dollars. Maternal Normal Delivery Eclampsia Hemorrhage Sepsis Family Planning FP- Oral FP- Condom FP- Injection FP- IDU FP- Sterilization (1) FP- Norplant Consumable Supplies Medicines Health Personnel Total Direct Costs 44.9 (75.7%) 7.6 (12.7%) 6.85 (11.5%) 59.33 69.5 (21.2%) 56.12 (80.5%) 278.5(32.4%) 147.6 (44.9%) 10.04 (14.4%) 456.4 (53.2%) 111.3 (33.9%) 3.55 (5.1%) 123.42 (14.4%) 328.40 69.70 858.38 0.14 (6.9%) 0.09 (4.3%) 0.14 (2.6%) 0.18 (1.7%) 0.35 (2.3%) 0.21 (0.1%) 1.96 2.66 5.10 11.00 15.35 144.48 1.82 (93.1%) 2.57 (96.6%) 0.08 (1.6%) 1.27 (11.6%) 12.99 (84.6%) 20.24 (14.0%) 4.94 (95.8%) 9.50(86.8%) 2.01 (13.1%) 124.03 (85.8%) The costs of asphyxia and hypothermia were not estimated because information regarding prices were not available for the main medical inputs. 38 In general, interventions for the care of maternal complications are considerably more expensive than the care of normal delivery and family planning methods. Training costs of Obstetric Emergency Management The training for obstetric emergency management in Mexico is provided through a 16-hour course provided by the Advanced Life Support in Obstetrics (ALSO). The course fee per person is US$378.79, including two-days worth of training time and course materials. This course is aimed at general physicians, obstetricians, gynecologists, pediatricians and general nurses, and it includes topics such as, acute hypertensive disease in pregnancy, obstructed labor, shoulder dystocia, intrapartum fetal monitoring, prevention and management of postpartum hemorrhage, fetal resuscitation and ultrasound type ―FAST‖ for obstetric emergencies. Guatemala Because some prices of consumable supplies in Guatemala were extremely high and no reliable, the average cost for a few consumable supplies were imputed from Mexico and Panama2. For extremely high prices, we preferred to work with prices closer to international market values. Table 4.3 shows direct costs per intervention for Guatemala. The most costly intervention was the manual vacuum aspiration at a cost of US$672, followed by sepsis care at a cost of US$582 and eclampsia care at a cost of US$206. Table 4.3. Direct costs per intervention from Guatemala, 2009 in US dollars Consumable Supplies Maternal Normal Delivery 46.35 (989.8%) Maternal complications Eclampsia 171.09 (82.7%) Hemorrhage 66.61 (89.8%) Sepsis 571.68 (98.2%) Manual vacuum aspiration (MVA) 672.14 (99.9%) Family Planning FP- Oral 0.00 FP- Condom 3.60 (99.3%) FP- Injection 5.20 (83.9%) FP- IDU 7.02 (94.5%) FP- Sterilization 8.09 (76.5%) (1) FP- Norplant 3.19 (2.2%) Medicines Health Personnel Total Direct Costs 3.32 (6.4%) 1.93 (3.7%) 51.60 3.82 (1.8%) 6.46 (8.7%) 3.79 (0.7%) 31.98 (15.5%) 1.15 (1.5%) 6.74 (1.2%) 206.89 74.20 582.21 0.07 (0.01%) 0.04(0.01%) 672.25 1.44 (97.5%) 0.04 (2.5%) 0.02 (0.7%) 0.04 (0.6%) 0.05 (0.7%) 0.14 (1.3%) 0.10 (0.1%) 1.48 3.60 6.20 7.43 10.57 145.02 0.96 (15.5%) 0.36 (4.8%) 2.34 (22.1%) 141.73 (97.7%) 1. Some prices of the health inputs for the MVA procedure in Guatemala were taken from the prices reported by Panama. 2. The price of the sub-dermal implant from Panama was taken from the price reported by Mexico. Nicaragua Intervention costs in Nicaragua were obtained from a cost sheet provided by the Nicaraguan MoH in 2009. There was information from a single health intervention, normal delivery care coinciding with the 12 health interventions 2 For imputing the prices for Guatemala, the unitary prices for consumable consumptions in Mexico and Panama were averaged. 39 that comprise the basic package defined for Mesoamerican countries. In Table 4.4, we report direct costs of normal delivery care and some medical interventions similar to the interventions included in the basic package defined by the Mesoamerican team of experts (preterm labor and newborn sepsis). The direct cost of the normal delivery is US$16. For this intervention, the highest cost is personnel time at a cost of US$7.17 (44.2%), followed by consumable supplies at a cost of US$ 5.81(35.8%). Costs of normal delivery care in Nicaragua were the lowest compared to the ones estimated in the other three countries. We attribute this low cost to the low level of salaries for health personnel in this country. Table 4.4. Direct costs per intervention from Nicaraguain 2009 US dollars. Some complications Preterm labor Sepsis of Newborn Consumable Supplies Medicines Health Personnel Total Direct Costs 3.19 (4.2%) 13.73 (16.6%) 32.70 (43.4%) 11.51 (13.9%) 39.41 (52.3%) 82.76 (69.5%) 75.30 82.76 5.81 (35.8%) 3.23 (19.9%) 7.17 (44.2%) 16.21 Maternal Normal delivery Discusion Interventions with the highest direct costs were those involving the care of maternal complications (eclampsia, hemorrhage, and sepsis) as well as manual vacuum aspiration. These high costs are mainly attributable to medicine and consumable supply prices. Among the family planning methods, the most expensive were sterilization, sub-dermal implants, and injection. The highest direct cost for normal delivery care was from Guatemala. This high direct cost is attributed to the cost of consumable supplies. In contrast, Nicaragua reported the lowest cost of normal delivery care, in part, related to the country’s reported low cost of consumable supplies and health personnel. These results are also important to identify prices of health supplies and drugs each country is possesses. We have found that prices of some consumable supplies and medicines can vary considerably between countries. It is important to consider that lower prices can represent significant savings when there are plans to expand health intervention coverage to a level that is needed in the region. The main limitation of this work is the lack of price information for health inputs from most of the countries involved in the MHI. Similarly, for those countries partial information has been obtained, we were required to impute some data from where cost information was not available. 40 CONSULTED BIBLIOGRAPHY Cairncross, S. and V. Valdmanis (2006). Water Supply, Sanitation,and Hygiene Promotion. Disease Control Priorities in Developing Countries 2nd ed Disease Control Priorities Project. Washington DC: World Bank. Curtis, V. and Cairncross (2003). "Effect of Washing Hands with Soap on Diarrhea Risk in the Community: A systematic Review." Lancet Infectious Diseases 3(5): 275-281. Drummond MF, O'Brien BJ, Stoddart GL and Torrance GW Methods for the Economic Evaluation of Health Care Programmes 2 ed. Oxford, Oxford Univeristy Press 1997 Fiedler, J. (2003). A Cost Analysis of the Honduras Community-Based Integrated Child Care Program, The International Bank for Reconstruction and Development / The World Bank. Fiedler, J. and B. Macdonald (forthcoming). "A Strategic Approach to the Unfinished Fortification Agenda: Feasibility, Costs and Cost-Effectiveness Analysis of Fortification Programs in 48 Countries." Food and Nutrition Bulletin. Gesaworld (2006). Oportunidades de Inversión en Nutrición Preventiva para Guatemala, Honduras, Nicaragua y El Salvador. Borrrador del Plan de inversiones en Nutrición Preventiva para El Salvador, BID. Hernández Sampieri R., Fernández Collado R, Baptista Lucio P. Metodología de la investigación; cuarta edición; Capítulo 14. Editorial McGrawHill. Pág. 597 Horton, S., M. Sheekar, et al. (2009 forthcoming). Scaling Up Nutrition: What will it cost?, The World Bank. Lara J Wolfson, François Gasse, Shook-Pui Lee-Martin, Patrick Lydon, Ahmed Magan, Abdelmajid Tibouti, Benjamin Johns, Raymond Hutubessy, Peter Salama, Jean-Marie Okwo-Bele. Estimating the costs of achieving the WHO–UNICEF Global Immunization Vision and Strategy, 2006–2015. Bulletin of the World Health Organization 2008;86:27–39. Limao N, Venables AJ. Infrastructure, geographical disadvantage, transport 33. costs, and trade. World Bank Econ Rev 2001;15:451-79. doi:10.1093/wber/15.3.451 McKinsey Consulting. Report to the GAVI Board, April 2004.31 Pan American Health Organization. Immunization Newsletter Volume XXXI, Number 1, February 2009. ISSN 1814-6244. Available at: http://www.paho.org/French/AD/FCH/IM/Snf3101.pdf Ranson MK, Hanson K, Oliveira-Cruz V, Mills A. Constraints to expanding 32. access to health interventions: an empirical analysis and country typology. J Int Dev 2003;15:15-39. doi:10.1002/jid.964 Robberstad, B., T. Strand, et al. (2004). "Cost-effectiveness of zinc as adjunct therapy for acute childhood diarrhoea in developing countries." Bulletin of the World Health Organization 82(7): 523-531. 41 UNICEF. (2008). "Complementary feeding." Retrieved Sept, 2009, from http://www.unicef.org/nutrition/index_24826.html. WHO. Vaccine-Preventable Diseases: Monitoring System 2005 Global 34. Summary. Geneva: WHO; 2005. Available at: http://www.who.int/immunization_monitoring/data/en/ WHO (2003). "Immunization, vaccines and Biologicals." from http://www.who.int/vaccines/en/vitamina.shtml. WHO (2002). Complementary feeding. Report of the global consultation, World Health Organization. WHO (1999). Management of Severe Acute Malnutrition: a manual for physicians and other senior health workers WHO/UNICEF Product information sheets36. . Geneva: WHO; 2000 (WHO/V&B/00.13). Available at: http://www.who.int/vaccinesdocuments/DocsPDF00/www518.pdf World Health Organization. Mother-Baby package; implementing safe motherhood in countries. Rev. 1. Ginebra: WHO, Division of Reproductive Health; 1994 42 ANEXXES Table A1. Opportunity map (Inteventions) Areas of Opportunity Strategies to reach target populations Monitoring and Evaluation Indicators Validity of Immunization Coverage Levels Lot quality sampling assessment baseline and subsequent assessments Percentage of validity assessments performed/assessments planned Serologic analysis of a sample of patients to validate coverage levels (tetanus or hepatitis B) Percentage of concordance between reported rates and those identified during the assessment Rapid monitoring assessment supervision and evaluation Coverage level by specific biologic agent and with full vaccine schedule . Increase effective coverage Reaching 95% coverage rate per biological Prevent missed opportunities and unmet needs by: - Community-based educational campaigns to reach the most socially excluded populations with culturally appropriate messages regarding the benefit of vaccination - Supplementary outreach campaigns that take services out into communities through mobile camps usually accompanied by energetic information campaigns regarding the benefits of vaccination Integrated rapid-impact package of intervention with other health-related interventions (maternal, nutrition, vector-borne diseases) (see probable indicators on table 7). Number and % of municipalities distributing culturally appropriate materials Number of persons reached with educational materials, talks or workshops Percentage of community-based workshops conducted versus those planned Percentage of people reached by education activities / community population Change in the coverage rate from baseline to intervals Public-private partnerships to develop social marketing strategies Verified effective vaccine coverage rate in target population Capacity-building at all levels with a focus at the community level and then at every level of the national immunization program An alternative proxy measure has been suggested by the COFVAL, correlating 1) the data on mortality and morbidity with 2) the data on raw coverage for each disease-vaccine by federal, state/provincial and local level. Unify information systems at the country level (Use mobile technology and internet-based systems to assist in vaccination-registry or a unified regional vaccination registry) For permanent health-centers need more hours of operation (weekends, holidays, and evenings) Effective vaccine use, contrast: a) the number of doses bought (at national, district, municipal level) b) coverage for a specific disease Percentage of health centers with extended service hours (among those for which this was a problem in the community). Information Systems Unify information systems at the country level (Use mobile technology and internet-based systems to assist in vaccination-registry or a unified regional vaccination registry – nominal census data) Capacity building at all levels Number of children/% of children in registry from target population Number of municipalities/% of municipalities using mobile technology to collect data/register children Number of municipalities/% of municipalities using internet based systems to assist in vaccine registry or regional vaccination registry Number of health works/% of health workers that have been trained to use 43 mobile technology and/or internetbased systems of vaccine registry Monitoring and Evaluation of National Immunization Programs Capacity building of personnel at the community level for monitoring vaccine uptake/demand of vaccine Percentage of active vaccine at the different locations (national, regional, local, and community level Supervision of cold-chain activities Number/Rate of illness due to VPDs in target population Community needs assessment Use a performance improvement and process evaluation approach to diagnose and systematically improve services, starting at the facility level by the community Providing community-health workers with information on how to use data for monitoring and evaluation, how to engage community leaders, and how to better manage vaccine stocks Number/Rate of deaths due to VPDs in target population Change in the burden of VPD in target population Change in the differences between the burden of VPDs in target populations and national averages Number of lab tests for VPDs completed for target population Epidemiologic Surveillance Improved detection by laboratory-based surveillance Creation or strengthening of a regional network of surveillance (epidemiologic and laboratory-based) Operational Activities of the National Immunization Program - Cold-Chain Increased number of supervisors and increased training of supervisors Use a performance improvement and process evaluation approach to diagnose and systematically improve services, starting at the facility level by the community - Human Resources Number of staff trained at all levels Percentage of workshops at all levels including community-based conducted versus those planned Percentage of supervisions conducted at all levels including community-based conducted versus those planned Knowledge Management **Web-based Library as part of the Mesoamerican Public Health Institute as a site for exchanging information on guidelines’, norms, technical procedures, publications, effective practices. Number of virtual websites Number of publications in peerreviewed journals Number of contributions to national or regional guidelines Number of effective practices shared by countries through the use of virtual information networks Introduction of New Vaccines Introduction of vaccines that may have a higher impact on decreasing the burden of disease in children under 5: -Rotavirus -Conjugate pneumococcal heptavalent Percentage of countries that introduce rotavirus (monovalent or pentavalent) Use seed money and search for other sources of sustainability to introduce these vaccines through PAHO, local governments, and GAVI (Honduras and Nicaragua) Percentage of countries that introduce conjugate pneumococcal heptavalent vaccine Taken from the Immunization Master Plan, September 30 2009. ** There is an existent web-based library platform established by the Virtual Mesoamerican Public Health Institute where countries can build upon their interventions and activities 44 Table A2. List of maternal and neonatal interventions and delivery platforms costed Intervention Maternal Normal delivery care Details Target Group Potential delivery platform(s) Prevention and management of infections: Clean delivery Antibiotics Vaccines Skin Care-to-skin Maternal- Complications Interventions to The Pan American Health reduce maternal Organization (PAHO) death promotes a more focused for acute postpartum now on effective vaginal bleeding interventions because of the immediately costs, including essential obstetric care (EOC), delivery assistance by trained personnel and better access to health care services maternal quality. Eclampsia Staff, medicines available, protocols available and known to everyone. Staff attending antenatal better prepared to detect early cases of pre-eclampsia Reduction of maternal morbidity and mortality by direct causes Hemorrhage An essential component in the field of mortality from hemorrhage is assured availability of safe blood Reduction of maternal morbidity and mortality by direct causes Sepsis Management of maternal sepsis (including treatment with intravenous or intramuscular antibiotics) Reduction of maternal morbidity and mortality by direct causes Increased number of hospitals with trained personnel to prevent and treat postpartum infections. Availability of highly effective antibiotics Increased frequency of use of effective modern contraception after childbirth and abortion The segmentation analysis of family planning services has shown little attention to rural, indigenous and high maternal and infant mortality. In fact, the existence of an unmet demand indicates the possibility of expanding the scale of public family planning services (Valladares R. y Luigi J. 2008). Increased use of a method for high efficiency and increased male involvement in FP Critical capabilities to manage complications in hospitals and health centers Increasing the rate of continued use of the methods. Decreased fertility Key management capabilities in health centers and hospitals Family planning: Implementation of contraceptive services post-partum and postabortion The "Vasectomy" to the list of methods available to the population actually Implant and IUD Intrauterine device Decreased fertility especially married women. Decreased grand multiparity should have an effect on maternal mortality Improvement of Procedures as offered and delivered contraceptive methods. Better understanding of the cost of program Need training hospitals for the care of complex cases and implement a referral network with efficient transfer can affect costs Reduction of maternal morbidity and mortality by direct causes Improved obstetric care in hospitals and centers. More trained personnel. Better referral systems to solve complex problems Reduction of maternal morbidity and mortality by direct causes An important component is prenatal care that is crucial for early detection of risk cases. The hospital staff should be well equipped to handle emergencies by preeclampsia/eclampsia. Worth the same considerations of high staff turnover that affects training costs Staff trained to treat bleeding complications and identify the need for transfusion and / or transfer to better-equipped center Community campaign: community health workers incorporate messages on vasectomy techniques Source: Prepared with information from the Mesoamerican Health Initiative (MHI), 2009 45