Anesthesia Duration & Tear Fluid Recovery: An Experimental Study
Anuncio
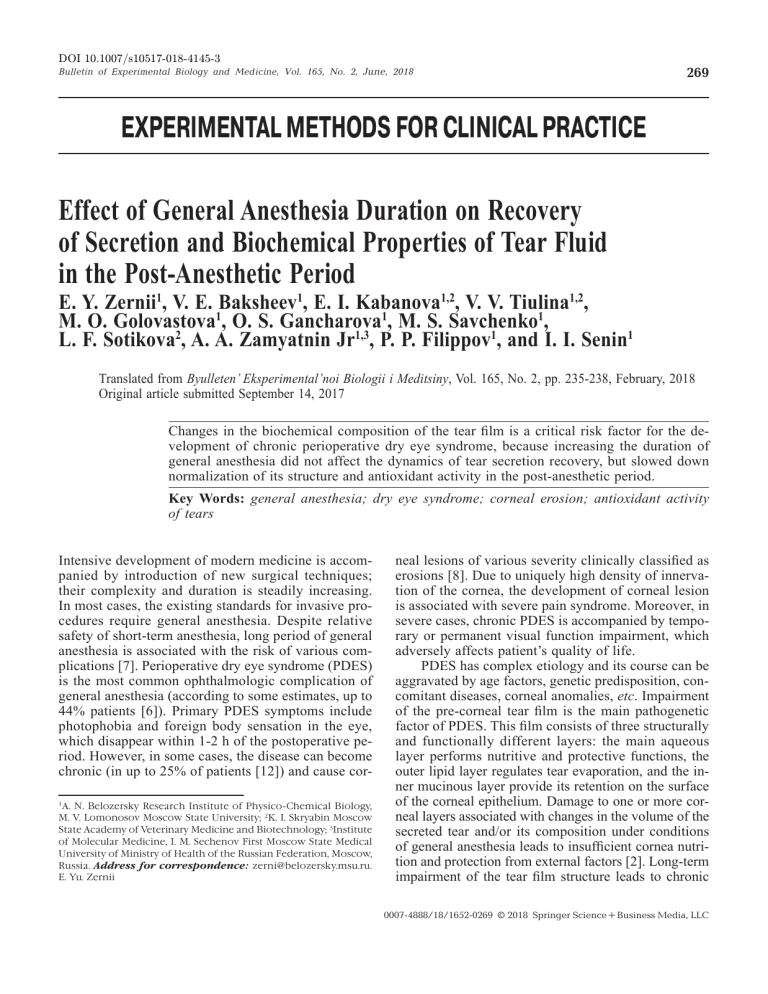
DOI 10.1007/s10517-018-4145-3 Bulletin of Experimental Biology and Medicine, Vol. 165, No. 2, June, 2018 269 EXPERIMENTAL METHODS FOR CLINICAL PRACTICE Effect of General Anesthesia Duration on Recovery of Secretion and Biochemical Properties of Tear Fluid in the Post-Anesthetic Period E. Y. Zernii1, V. E. Baksheev1, E. I. Kabanova1,2, V. V. Tiulina1,2, M. O. Golovastova1, O. S. Gancharova1, M. S. Savchenko1, L. F. Sotikova2, A. A. Zamyatnin Jr1,3, P. P. Filippov1, and I. I. Senin1 Translated from Byulleten’ Eksperimental’noi Biologii i Meditsiny, Vol. 165, No. 2, pp. 235-238, February, 2018 Original article submitted September 14, 2017 Changes in the biochemical composition of the tear film is a critical risk factor for the development of chronic perioperative dry eye syndrome, because increasing the duration of general anesthesia did not affect the dynamics of tear secretion recovery, but slowed down normalization of its structure and antioxidant activity in the post-anesthetic period. Key Words: general anesthesia; dry eye syndrome; corneal erosion; antioxidant activity of tears Intensive development of modern medicine is accompanied by introduction of new surgical techniques; their complexity and duration is steadily increasing. In most cases, the existing standards for invasive procedures require general anesthesia. Despite relative safety of short-term anesthesia, long period of general anesthesia is associated with the risk of various complications [7]. Perioperative dry eye syndrome (PDES) is the most common ophthalmologic complication of general anesthesia (according to some estimates, up to 44% patients [6]). Primary PDES symptoms include photophobia and foreign body sensation in the eye, which disappear within 1-2 h of the postoperative period. However, in some cases, the disease can become chronic (in up to 25% of patients [12]) and cause cor1 A. N. Belozersky Research Institute of Physico-Chemical Biology, M. V. Lomonosov Moscow State University; 2K. I. Skryabin Moscow State Academy of Veterinary Medicine and Biotechnology; 3Institute of Molecular Medicine, I. M. Sechenov First Moscow State Medical University of Ministry of Health of the Russian Federation, Moscow, Russia. Address for correspondence: zerni@belozersky.msu.ru. E. Yu. Zernii neal lesions of various severity clinically classified as erosions [8]. Due to uniquely high density of innervation of the cornea, the development of corneal lesion is associated with severe pain syndrome. Moreover, in severe cases, chronic PDES is accompanied by temporary or permanent visual function impairment, which adversely affects patient’s quality of life. PDES has complex etiology and its course can be aggravated by age factors, genetic predisposition, concomitant diseases, corneal anomalies, etc. Impairment of the pre-corneal tear film is the main pathogenetic factor of PDES. This film consists of three structurally and functionally different layers: the main aqueous layer performs nutritive and protective functions, the outer lipid layer regulates tear evaporation, and the inner mucinous layer provide its retention on the surface of the corneal epithelium. Damage to one or more corneal layers associated with changes in the volume of the secreted tear and/or its composition under conditions of general anesthesia leads to insufficient cornea nutrition and protection from external factors [2]. Long-term impairment of the tear film structure leads to chronic 0007­-4888/18/16520269 © 2018 Springer Science+Business Media, LLC 270 Bulletin of Experimental Biology and Medicine, Vol. 165, No. 2, June, 2018 EXPERIMENTAL METHODS TO CLINIC destructive processes in the cornea, including oxidative stress and local inflammatory responses, induction of apoptosis and necrosis of corneal epitheliocytes, erosive changes, and manifestations of PDES symptoms. It is currently accepted that primary PDES is associated with a decrease in the volume and quality of tear produced under conditions of general anesthesia. On the one hand, the supressive effect of anesthetics on parasympathetic innervation of the main lacrimal glands significantly inhibits tear production. On the other hand, general anesthesia affects also other tissues producing tear components, such as meibomian gland and conjunctiva [10]. We have previously demonstrated that not only the volume of produced tears decreased, but also protein composition (antioxidant protection enzymes, inflammatory cytokines, etc.) and, probably, lipid composition of the tear film are changed under conditions of general anesthesia, which can also induce pathological process in the cornea [11]. The mechanisms of transformation of primary PDES into the chronic form are poorly understood, but it is known that the incidence of this form increases with increasing anesthesia duration; therefore, the risk of its development is associated with persistence of secretory and biochemical disorders. At the same time, it remains unclear, which of these factors has the strongest impact on the development of chronic corneal lesions. The aim of this study was to specify the relationship between general anesthesia duration and tear production/tear recovery dynamics in the post-anesthetic period, using the previously developed experimental animal PDES model [10-12]. MATERIALS AND METHODS The study was carried out on pigmented rabbits weighing 2.3-3 kg (KrolInfo). The animals were kept under 12/12 h dark/light cycle, at 22-25oC and 55-60% humidity. All procedures were performed in accordance with the recommendations [9]. The study protocol was approved by the bioethics commission of A. N. Belo­ zersky Research Institute of Physico-Chemical Biology (No. 1/2016). The animals were divided into 4 groups (6 rabbits per each) and subjected to general anesthesia lasting 0.5, 1, 3, or 6 h, produced by intramuscular injection of 50 mg/ml tiletamine and 50 mg/ml zolazepam (1624 mg of the mixture per 1 kg body weight). When required, the injections were repeated to maintain narcotic sleep for the required period. Tear production intensity and tear film stability were measured before and immediately after general anesthesia, and also 3 and 6 h, and 1, 2, 5, 7 days after anesthesia completion using Schirmer test [1] and Norn probe [4]. Total antioxidant activity of the tear was measured in samples, obtained by extracting Schirmer test strip fragments with 150 μl of PBS using the hemoglobin-H2O2-luminol system [1]. The chemiluminescence of samples was measured using Glomax-Multi Detection System (Promega). The data were processed statistically using SigmaPlot 11 (SYSTAT Software). RESULTS According to the results of the standardized Schirmer test, a 3-fold decrease in the amount of secreted tear fluid was observed in all animals under conditions of general anesthesia (Fig. 1). However, normal tear production was restored as soon as in 6 h after recovery; recovery rate did not depend on the duration of general anesthesia. A different picture was observed, when tear film stability was monitored (using the Norn probe) in the post-anesthetic period (Fig. 2). Increasing narcosis duration increased the time required for complete recovery of this parameter: from 6 h in cases of 30min and 60-min anesthesia to 1 and 2 days in cases of 3- and 6-h general anesthesia, respectively. Thus, increased duration of general anesthesia did not cause long-term disturbances in tear secretion; its recovery was primarily determined by the total recovery period that lasted ~5 h. At the same time, protein and/or lipid composition of the secreted tear was impaired during anesthesia, as far as tear film structure was disturbed and its recovery was slowed down, and both were worsened upon anesthesia prolongation. Changes in the biochemical composition of the tear during general narcosis can affect not only proteins and lipids, but also other components, which include the set of low-molecular-weight antioxidants (cysteine, glutathione, tyrosine, uric and ascorbic acid salts), which determine the overall antioxidant activity Fig. 1. Dynamics of tear production recovery in animals subjected to general anesthesia lasting for 0.5, 1, 3, or 6 h. E. Y. Zernii, V. E. Baksheev, et al. 271 Fig. 2. Dynamics of tear film stability recovery in animals subjected to general anesthesia lasting for 0.5, 1, 3, or 6 h. Fig. 3. Dynamics of tear antioxidant activity in animals subjected to general anesthesia lasting 0.5 h, 1, 3 or 6 h. of the tear film [3,5]. Indeed, according to our data, already in the course of anesthesia, there was observed more than 2-fold decrease in the antioxidant activity of tear in animals of all groups (Fig. 3). The time required for recovery of this parameter increased by 5 days with the increase in anesthesia duration from 0.5 h to 6 h. Thus, the decrease in the content/acti­vity of biochemical tear components, such as proteins, lipids, and low molecular weight antioxidants, is quite protracted after anesthesia. As a consequence, there is no cornea epithelium protection from damage, including mechanical factors, oxidative stress, infections, etc., for a long time. It is the long-term decrease in the protective properties of the tear film in post-anesthetic period, which can be the main cause of PDES transformation into chronic form, the probability of which, as shown previously, increases with increasing anesthesia duration [8]. Thus, it can be concluded that general anesthesia does not significantly affect the amount of secreted tears, but reduces its protective properties; their recovery is delayed, taking up to several days depending on anesthesia duration. These observations provide grounds for specification of PDES prevention strategies in surgical patients, and suggest the advisability of ophthalmic examinations of patients after prolonged surgical interventions with respect to the risk of postoperative corneal lesions. The study was supported by the Russian Science Foundation (grant No. 16-15-00255). cycle. Prog. Retin. Eye Res. 2015;45:132-164. 3. Choy CK, Cho P, Chung WY, Benzie IF. Water-soluble antioxidants in human tears: effect of the collection method. Invest. Ophthalmol. Vis. Sci. 2001;42(13):3130-3134. 4. Cullen CL, Lim C, Sykes J. Tear film breakup times in young healthy cats before and after anesthesia. Vet. Ophthalmol. 2005;8(3):159-165. 5. Gogia R, Richer SP, Rose RC. Tear fluid content of electrochemically active components including water soluble antioxidants. Curr. Eye Res. 1998;17(3):257-263. 6. Grover VK, Kumar KV, Sharma S, Sethi N, Grewal SP. Comparison of methods of eye protection under general anaesthesia. Can. J. Anaesth. 1998;45(6):575-577. 7. Harris M, Chung F. Complications of general anesthesia. Clin. Plast. Surg. 2013;40(4):503-513. 8. Martin DP, Weingarten TN, Gunn PW, Lee K, Mahr MA, Schroeder DR, Sprung J. Performance improvement system and postoperative corneal injuries: incidence and risk factors. Anesthesiology. 2009;111(2):320-326. 9. Statement for the Use of Animals in Ophthalmic and Visual Research. Association for Research in Vision and Ophthalmology, 2016. [URL: https://www.arvo.org/content-detail/ level2-about2/policies2/statement-for-the-use-of-animals-inophthalmic-and-visual-research/]. 10. Zernii EY, Gancharova OS, Baksheeva VE, Golovastova MO, Kabanova EI, Savchenko MS, Tiulina VV, Sotnikova LF, Zamyatnin AA Jr, Philippov PP, Senin II. Mitochondria-Targeted Antioxidant SkQ1 Prevents Anesthesia-Induced Dry Eye Syndrome. Oxid. Med. Cell. Longev. 2017. 2017. ID 9281519. doi: 10.1155/2017/9281519. 11. Zernii EY, Golovastova MO, Baksheeva VE, Kabanova EI, Ishutina IE, Gancharova OS, Gusev AE, Savchenko MS, Loboda AP, Sotnikova LF, Zamyatnin AA Jr, Philippov PP, Senin II. Alterations in tear biochemistry associated with postanesthetic chronic dry eye syndrome. Biochemistry (Mosc). 2016;81(12):1549-1557. 12. Zernii EY, Gancharova OS, Ishutina IE, Baksheeva VE, Golovastova MO, Kabanova EI, Savchenko MS, Serebryakova MV, Sotnikova LF, Zamyatnin AA Jr, Philippov PP, Senin II. Mechanisms of perioperative corneal abrasions: alterations in tear film proteome. Biomed. Khim. 2016;62(6):683-690. REFERENCES 1. Bhattacharya D, Ning Y, Zhao F, Stevenson W, Chen R, Zhang J, Wang M. Tear production after bilateral main lacrimal gland resection in rabbits. Invest. Ophthalmol. Vis. Sci. 2015;56(13):7774-7783. 2. Braun RJ, King-Smith PE, Begley CG, Li L, Gewecke NR. Dynamics and function of the tear film in relation to the blink

![No se lo digas a nadie [Don`t Tell Anyone], (Peru, Francisco](http://s2.studylib.es/store/data/005872151_1-1dd0893b8e1dbcf7a90c9884036118b5-300x300.png)