Clip Placement after Stereotactic Vacuum-assisted Breast Biopsy’
Anuncio

Laura Liberman,
MD
Andrea
F. Abramson,
#{149}
D. David
Dershaw,
MD
MD #{149}Cynthia
M. Thornton,
Clip Placement
Vacuum-assisted
PURPOSE:
usefulness
ing clip
assisted
AND
METHODS:
Retrospective
review
was performed
of
57 lesions
that underwent
placement
of a localizing
clip after stereotactic
vacuum-assisted
biopsy
with an 11gauge
(n = 42) or 14-gauge
(n = 15)
probe.
The clip was placed
when
images obtained
after stereotactic
biopsy suggested
that the lesion seen at
MATERIALS
Coordiimages
obtained
after placement
were cornpared with lesion coordinates
determined before
biopsy.
Surgery
was performed
in 25 cases. Mammographic
and histopathologic
findings
were reviewed.
The distance
from clip to
lesion
site was less than 1 cm in 40
(95%) of 42 lesions
that underwent
clip placement
with the 11-gauge
probe versus
11 (73%) of 15 lesions
that underwent
clip placement
after
14-gauge
biopsy
(P < .04). The biopsy site was identified
in the surgical specimen
in 19 (100%) lesions
with clips after 11-gauge
biopsy
and
five (83%) of six lesions
with clips
after 14-gauge
biopsy.
No cornplications occurred.
RESULTS:
A localizing
clip can
be placed
in proximity
to the stereotactic biopsy
site through
an 11-gauge
probe.
Clip placement
can enable
accurate
localization
for surgical
excision.
CONCLUSION:
A. Morris,
MD
#{149}
Paul Peter Rosen,
MD
after
Stereotactic
Breast
Biopsy’
To assess
accuracy
and
of placement
of a localizafter stereotactic,
vacuumbreast
biopsy.
mammography
was removed.
nates
of the clip on stereotactic
Elizabeth
RT(R)(M)
#{149}
were
radiopaque
localizing
clip has
been approved
by the U.S. Food
and Drug Administration
for placement after directional,
vacuumassisted
breast
biopsy
(1-3). The goal
of clip placement
is to enable
subsequent
surgical
excision
of the biopsy
site, even if the mammographic
findings
sion
associated
with
the original
were
removed
completely.
or may have
pletely.
Clips
Biopsies
leTo
with
opsy
reotactic,
vacuum-assisted
fered as an alternative
for mammographically
was
instrument
bowl
mm
14-gauge
and
for the
probe
The
were
Biopsies
were
performed
for
dian
of 13 specimens
around
increments
tion
suggested
findings
Index
00.31,
that
Radiology
.
with
Biopsies,
Stereotaxis,
1997;
tissue
the
acquisi-
technology,
00.1261
requests
RSNA,
See also
©
with
patients
(mean,
per
lesion.
a minimum
per lesion
14; range,
The
of eight
by rotating
the face
(1-5).
8-
protocol
speci-
the aperture
of the clock
Additional
of the radiologist
Breast,
biopsy,
00.1261
performing
#{149}
Breast
the biopsy.
neoplasms,
diagnosis,
205:417-422
I From
the Departments
of Radiology,
Breast
and Pathology
(P.P.R),
Memorial
Sloan-Kettering
Received
May 6, 1997; revision
requested
June
reprint
in
specimens
were obtained
to sample
a
larger area of breast tissue at the discretion
lesion
00.1261
obtained
to obtain
mens
stereo-
original
were
was
the mammographic
associated
terms:
00.32
after
in the study.
on a dedicated
table (StereoGuide
DSM; LoRad, Danbury,
Conn). The 11gauge probe was placed to a depth 2 mm
proximal
to the calculated
depth of the
center of the lesion to acquire tissue. A me-
in 1.5-hour
obtained
in 39
median,
prone
of the bowl
tactic images
years;
two. The median
lesion size was 7 mm
(mean, 7 mm; range, 2-15 mm).
after
when
the 11-
42 lesions
43-81
included
34)
biopsy
through
remaining
the 11-gauge probe). No lesions were cxcluded because of small size. A 2 X 2-mm
radiopaque
localizing
clip (MicroMark;
Biopsys
Medical,
Irvine, Calif) was placed
vacuum-assisted
placed
findings
in these
42 lecalcifications
in 26, uncalcified
in 14, and mass and calcifications
mass
(22
27 mm
and
Biopsys
Mammographic
sions
were
to accommodate
probe
was
(age range,
patients
24, 1997, ste-
of the biopsy
Probes
(Mammotome;
clip
localizing
biopsy
was ofto surgical
biopsy
evident
lesions
in
inadequate
the tip
11-gauge
gauge probe after biopsy. Two lesions were
excluded
because
the stereotactic
images
obtained
after clip placement
were not
which surgery
would otherwise
have been
performed
unless (a) the patient had a
bleeding
diathesis,
(b) the patient
was unable to tolerate the procedure,
or (c) the
thickness
of compressed
breast parenchyma
of stain-
Medical)
from October 31, 1996, to April
24, 1997. In 44 (46%)lesions,
the radiopaque
METHODS
May 1, 1996, to April
5, 1997,
used
Retrospective
review was performed
of
mammograms
of 96 consecutive
lesions
that underwent
stereotactic
biopsy with an
11-gauge directional,
vacuum-assisted
bi-
58 years)
From
com-
February
of titanium;
clips
less steel.
available.
AND
removed
before
were constructed
after that time were constructed
date, there is little published
expenience with regard
to use of the clip, to
our knowledge
(1-3). This study
was
undertaken
to assess
the accuracy
and
usefulness
of placement
of a localizing
clip after stereotactic,
vacuum-assisted
breast
biopsy
to enable
subsequent
surgical
excision
of the biopsy
site.
MATERIALS
been
used
Imaging
Section
(L.L., D.D.D.,
E.A.M.,
A.F.A., C.M.T.),
Cancer
Centet
1275 York Ave. New York, NY 10021.
5; revision
received
July 21; accepted
July 23. Address
to L.L.
1997
the article
by Burbank
and Forcier
(pp 407-415)
in this issue.
417
‘p
-.
a.
f.
e.
b.
C.
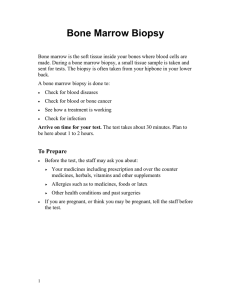
Figure
1.
woman.
Clip
placement
(a) Collimated
through
the il-gauge
craniocaudal
mammogram
probe
in a 63-year-old
demonstrates
a clus-
ter of pleomorphic
calcifications
measuring
1.0 cm in the longest dimension. (b) Stereotactic
images obtained after acquisition
of the first specimen
reveal
the probe in proximity
to the remaining
calcifications.
(c) Stereotactic
images
obtained
after tissue
acquisition
show
air and hematoma
at the biopsy site. No residual
calcifications
are identified.
(d) Stereotactic
images
obtained
after suctioning
and clip placement
show
air at the biopsy
site.
The clip is attached
to a side wall of the biopsy
cavity.
Collimated
(e) craniocaudal
mammogram
and (f) mediolateral
oblique
mammogram
obtamed
after clip placement
demonstrate
the biopsy
cavity
and accurate
positioning
of the clip. Histopathologic
analysis
revealed
benign breast
tissue
with adenosis
and microcalcifications.
d.
The
decision
mens
of the
to obtain
was based
specimens
cifications,
on results
in lesions
visual
specimens,
images.
radiography
tissue
the biopsy
the cutter
at 22 kVp
was
complete,
ply continuous
the
off
bank
F, oral
Stereotactic
the
the
vacuum
button
to ap-
to the bowl,
bowl
360#{176}
twice
communication,
images
were
biopsy
to ascertain
findings
associated
had been removed.
back
“VAC”
vacuum
open
and
the tip of the cutter was at the proximal
end of the bowl. The operator
toggled
the
May
obtained
and
manually
cavity
was suctioned
by pulling
all the way back, turning
off the
and
of the bowl
ing the dial
1996).
after
ter lumen,
system.
of the
The
tional
location
used
(3).
the probe
418
#{149}
Radiology
maneuver,
the
cutter
end
of clip
of the
lated
probe
to be
collected,
to distal
then
The
around
on
into
cleared
the
cut-
The
an
addi-
first
to a
calcu-
ducer,
the
with
the
basis
respect
(z) direction,
to the initial
direction
face
of clip
of the
of (a) the
clock
location
to the lesion
was
of
on pre-
clip
The
was
marks
by
probe
was
the
pulling
withdrawal,
tamed
on
clip
aperture
opening
to the
applied
was
then
squeeze
of
introducer,
to the
of the probe
tubing
in the
advanced
black
was
axis.
first
selectively
chamber)
vacuum
mark
deployed
handles,
and
clip introducer
the
the
the
to the desired
on the clip
was
clip
and
introduced
to the second
the squeeze
leased.
The
turning
probe
introducer
vacuum
the
if the
by
of the
bowl
(collecting
pinching
off the
from
withdrawn
placement
bowl
black
two
and
position;
the clip was placed
in the 6-o’clock
The radiologist
set the direction
of the clip
back.
was
z coordinate.
chosen
pulled
and
5 mm
in the depth
7 mm proximal
placement
this
the
proximal
12-o’clock
“high,”
position.
and back
many
times
by turnon the probe
driver.
Additional
probe
Clip
placement
through
the li-gauge
probe
is illustrated
in Figure
1. Before
clip
placement,
the “tap
tap”
maneuver
was
To perform
the
the
short
bursts
of vacuum
were
applied
while
the cutter
was pulled
back.
This maneuver
allowed
tissue
fragments
in the bowl
or
shaft
lesion
manipulated
from
(Bur-
if the mammographic
with the original
postfire
stereotactic
images
and (b) images obtained
after tissue acquisition.
If
the probe was “low”
with respect
to the
lesion,
for example,
the clip was placed
in
cutter
was pulled
back,
the vacuum
was
shut
off, and the front
vacuum
tube
was
pinched
off. The cutter
was
then
brought
forward
to the precut
stop
position
so that
vacuum
acquisition
pressing
rotating
tissue
of stereotactic
calcifications,
was per-
magnification
pinching
tubing,
of the
and
assessment
In lesions
containing
of the specimens
After
speci-
of radiography
evident
as cal-
inspection
formed
with X1.8
and 4 mAs (3).
vacuum,
additional
from
by
the
on the introby
pressing
vacuum
was rewas withdrawn
handles;
forward
pressure
the hub of the clip
during
was
mainintroducer
November
1997
.
Table 1
Location of the Clip
Lesion Site
Relative
After the side
gauge
calibrated
(Manan
Medical
to
was
Biopsy
Method
:
-
I-
Distance
on
Stereotactic
Images
(mm)
11-gauge
(n = 42)
14-gauge
(n = 15)
0
Total
Median
Mean
Range
5.6
5.5
2.3-12.0
<5mm
5-9 mm
lOmm
22 (52)*
6.7
7.9
1.5-26.8
18(43)*
4(27)*
7 (47)*
2(5)*
Figure
4(27)*
Radiograph
from
1.0
1.2
0.9
1.4
Range
0.0-3.6
0.2-3.8
attached
Mean
Range
3.1
3.0
0.2-5.9
1.5
2.3
0.7-6.1
Median
3.8
5.6
sions
3.8
0.3-11.9
6.9
0.2-26.6
error
Deep
Superficial
23 (55)*
19 (45)*
11 (73)*
to the number
placing
lesion
Numbers
are percentages.
to the depth of the clip relative
needle
in
with
in which
hub.
After
the clip
drawn
emerged
from
introducer
completely,
the
was
bowl
were
obtained
firm
clip
The
The
after
clip
placement
images
were
the
coordinates
of the
clip
aper-
from
May
cording
clip
site
any direction
the absolute
tween
on
reviewed.
ment
obtained
stereotactic
from
clip
to lesion
ages
was
calculated
the sum
distances,
images
of the
The
clip
total
square
of the squares
of the
per the Pythagorean
as
imroot
of
x, y, and
theorem
z
(6).
A mammogram
was
obtained
after
bi-
the location
opsy
site
toma
was
tained
of the clip
on
standard
after
biopsy
in 29 (69%)
obtained
gested
that
lesion
was
the
original
removed
lesions
Volume
Surgical
included
in five
205
procedures
mastectomy
Number
and
2
and
placed
were
after
not obtained;
in 20
excluded
clip
place-
the remaining
15
in the study.
These
in 15 patients
(age
median,
56 years).
A
of 16 specimens
(mean,
17; range,
were obtained
per lesion.
Mammographic
findings
in these 15 lesions
were
calcifications
in 11, uncalcified
mass in
two,
and mass and calcifications
in two.
The median
lesion size was 4 mm (range,
3-10
mm).
Clip placement
after 14-gauge
vacuumassisted
biopsy
differed
from clip placement through
the 11-gauge
probe.
Because
the clip cannot
be placed
through
the 14probe,
the
the biopsy
reotactic
probe
was
withdrawn
cavity
was
were
obtained
images
essary
for
ploy
in the
suctioned.
Ste-
and
a side
the
clip
to attach
breast.
It was
to tissue
believed
The
necto de-
prefer-
of 42 ledimin-
breast.
Targeting
placement
performed
on
after
clip
in seven
excision
was
able for the clip to attach
to a side wall of
the biopsy
cavity
rather
than to a near or
far wall owing
to potential
error in the
depth
(z) direction
in the compressed
sug-
mammographic
patients
#{149}
ob-
biopsy
in 30 (71%)
clip
ac-
previ-
wall of the biopsy
cavity
was targeted.
side wall was targeted
because
it was
of 42 lesions.
after
sions,
obscured
in 10 (24%),
ished
in two (5%).
Surgery
was subsequently
19 lesions.
placement
in
Hema-
on mammograms
30, 1996,
described
8-39)
gauge
to the bi-
projections.
observed
Mammograms
relative
to October
protocol
A localizing
were
after
opsy
that consisted
of craniocaudal
and
mediolateral
oblique
views
of the breast
which
biopsy
was performed
to ascertain
bi-
median
and
the
distance
site on stereotactic
as the
11-51
days)
after
stereotactic
14-
biopsy.
Needle
and surgical
histopathologic
findings
were reviewed.
Data
were analyzed
with a computerized
statistics program
(Epi-Info;
Centers
for Disease
Control,
Atlanta,
Ga). Statistical
significance of results
was determined
with the
2 and
Fisher exact tests.
Table
vacuum-assisted
lesions
were
included
15 lesions
occurred
range,
43-80
years;
in
(x, y, or z) was calculated
value of the difference
be-
the coordinate
in that direction.
lesion
ob-
RESULTS
performed
lesions
(24%) lesions. Five lesions
because stereotactic
images
on the clip and were cornwith coordinates
of the lesion deterbefore biopsy.
The distance
from
to lesion
(3).
was
with
a 14-gauge
Biopsys
Medical)
1, 1996,
to the
ously
to con-
by “targeting”
pared
mined
were
gauge
vacuum-assisted
localization
images
Probes
of 85 consecutive
stereotactic
withand
the
images
were
in 12 lelocalization
review
was performed
(Mammotome;
deployment.
stereotactic
localization
14-gauge
opsy
probe
of the
ture
was rotated
180#{176}
and closed,
probe
was removed.
Stereotactic
of the
images
to the
of mammograms
marks
cleaning
clip.
Needle
A retrospective
black
illustrates
in 11 lesions
were reviewed.
The
interval
from stereotactic
biopsy
to
localization
was 21 days (mean,
30
Biopsies
both
The clip
case
days;
range,
10-92
days).
In all 19 lesions
in which
surgery
was performed,
surgical
histopathologic
findings
were
reviewed.
site.
until
This
the
in 12 patients.
images
median
needle
4 (27)*
of lesions.
in the breast.
stereotactic
tained
to confirm
accurate
positioning,
and
the clip was deployed.
Stereotactic
images
were obtained
to confirm
deployment
of
the clip. Coordinates
of the clip on the stereotactic
images
were compared
with lesion
coordinates
before biopsy.
Mammograms
obtained
immediately
after stereotactic
biopsy
and clip placement
in these 15 lesions showed
a hematoma
in 11 (73%).
Mammograms
obtained
after biopsy
suggested
that the original
mammographic
lesion was completely
removed
in nine
(60%) of 15 lesions,
obscured
in one (7%),
and diminished
in five (33%).
Six lesions
underwent
needle
localization a median
of 15 days
(mean,
21 days;
range,
Mean
Range
Refers
in which
of thorough
before
preoperative
parentheses
t Refers
fragment
in a case
fragment.
the importance
z
z
of a tissue
probe
to deploy
to this
probe
Median
the
the clip failed
Median
Mean
Y
*
2.
retrieved
x
placed,
wall was targeted,
a 13trocar-style
biopsy
needle
Products,
Northbrook,
Ill)
after
necessary
the
11-gauge
the
after
because
probe
the use of vacuum
bowl of the probe.
side
11-gauge
clip
wall
biopsy
placement
for
clip
was
is accomplished
to pull
tissue
not
through
with
into
the
1 shows
the distance
from
the
clip to the lesion
site on steneotactic
images
obtained
after biopsy.
The distance
from
the clip to the lesion
site
was less than
1 cm in 40 (95%)
of 42
lesions
in which
clips
were
placed
through
the 11-gauge
probe
versus
11
(73%)
of 15 lesions
in which
clips
were
placed
after 14-gauge
vacuum-assisted
biopsy
(P < .04). The largest
errors
were
in the depth
or z axis. No complications
on untoward
reactions
to
the clip were
encountered.
In two additional
lesions
in which
stereotactic
11-gauge
vacuum-assisted
biopsy
was performed
during
this
period,
the clip attached
to fragments
in the bowl
of the probe
and failed
to
deploy
in the breast
(Fig 2). One of
these
was the first case in which
clip
placement
was attempted
through
the
11-gauge
probe;
the other
occurred
in
the 2nd month
of our experience
with
this clip.
Needle
localization
images
in 11
patients
who had undergone
clip
placement
after
11 -gauge
stereotactic
vacuum-assisted
biopsy
revealed
hematoma
at the biopsy
site in four
(36%)
patients.
These
hematomas
were
0.6-2.4
cm (median,
1.5 cm;
mean,
1.5 cm). Needle
localization
images
in six patients
who
had undergone
clip placement
after
14-gauge
stereotactic
vacuum-assisted
biopsy
showed
no evidence
of hematoma.
No
air was identified
on images
obtained
during
needle
localization.
Radiology
.
419
In all 19 lesions
in which
surgery
was performed
after
clip placement
through
the 11-gauge
probe,
the biopsy
site was identified
at histopathologic
analysis
of the surgical
specimen
(Fig 3). Correlation
of stereotactic
11gauge
vacuum
biopsy
findings
and
surgical
histopathologic
findings
is
shown
in Table 2. There
were no atypical ductal
hypenplasia
or ductal
carcinoma
in situ “underestimates”
(2). In
three
ductal
carcinoma
in situ
and
‘1
two
atypical
surgical
onstrated
ductal
hyperplasia
lesions,
histopathologic
analysis
demno residual
carcinoma
or
atypical
ductal
hyperplasia,
‘
nespec-
tively,
although
the biopsy
sites were
identified.
Of six lesions
that underwent
surgery after 14-gauge
steneotactic
vacuumassisted
biopsy
and clip placement,
the biopsy
site was
identified
at histo-
‘
a.
b.
pathologic
analysis
in five (83%)
lesions (Table 3). In one patient
in whom
ductal
carcinoma
in situ was diagnosed
at 14-gauge
vacuum-assisted
biopsy,
the clip was 3 mm distant
from
the biopsy
site on stereotactic
images
obtained
after biopsy.
Needle
localization
of the clip was performed,
but neither
the clip nor the carcinoma
were
removed
at surgery.
Subsequent
neexcision
yielded
the clip and nevealed
ductal
carcinoma
in situ.
DISCUSSION
A directional,
vacuum-assisted
biopsy
instrument
is available
for performing
percutaneous
breast
biopsy
(1-5,7,8).
Larger
volumes
of tissue
are
obtained
with
this equipment
than
with
an automated
gun for two reasons.
First,
the vacuum
instrument
enables
acquisition
of larger
tissue
specimens,
with
mean
specimen
weights
of 17 mg for the automated
gun and needle
(5), 34 mg for the 14gauge
vacuum-assisted
instrument
(5), and 100 mg for the 11-gauge
vacuum-assisted
biopsy
instrument
(Burbank
F, oral communication,
April
1997). Second,
the ability of the vacuum
instrument
to obtain
multiple
samples
with
a single
insertion
and to suction
blood
from
the biopsy
site facilitates
acquisition
of a larger
number
of tissue specimens
than
was feasible
previously
(5).
Because
of the large
volumes
of
tissue
that may be removed
with the
vacuum
device,
the mammognaphic
findings
associated
with
the original
lesion
may be removed
completely
at
vacuum-assisted
biopsy.
In two previously
published
series
of 14-gauge
vacuum-assisted
biopsy,
Burbank
et al
(5) and
420
Liberman
Radiology
#{149}
et al (3) reported
d.
C.
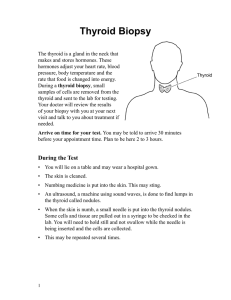
Figure
3.
(a) Collimated
mediolateral
oblique
mammogram
in a 45-year-old
woman
demon-
strates
a cluster
of pleomorphic
calcifications
(arrow)
measuring
0.5 cm in the longest
dimension. (b) Collimated
mediolateral
oblique
mammogram
obtained
after stereotactic
11-gauge
vacuum-assisted
biopsy
and clip placement
demonstrates
no residual
calcifications.
The clip is
located
within
the biopsy
cavity.
Histopathologic
analysis
revealed
ductal
carcinoma
in situ.
(c) Collimated
mediolateral
oblique
mammogram
obtained
during
needle
localization
demonstrates
the wire localizing
the clip. (d) Radiograph
of the specimen
shows
the clip. Surgical
histopathologic
analysis
revealed
ductal
carcinoma
in situ.
complete
removal
of the mammographic
findings
in 48% and 13%, respectively,
of all lesions,
and in 79%
and 58%, respectively,
of lesions
5 mm
in diameter
or less. Complete
removal
of the mammographic
lesion
does
not
ensure
complete
excision
of the histologic
process
(3). Mammographic
findings
after
stereotactic
vacuumassisted
biopsy
are transient
and cannot be relied
on to localize
the biopsy
site for subsequent
surgical
excision
(3). Safe use of the vacuum
biopsy
instrument,
therefore,
necessitates
the ability
to place
a localizing
marker
in proximity
able subsequent
to the biopsy
surgical
site to enexcision
if
necessary.
Our findings
show
ment
of the localizing
that
clip
after
placethrough
an
11-gauge
probe,
the biopsy
site was
identified
successfully
in 100%
of lesions
in which
surgical
excision
was
performed.
After clip placement,
needle
localization
can be performed
successfully, even
if the mammognaphic
findings associated
with
the original
lesion have
been
removed
completely.
For patients
who
undergo
mastectomy
after
clip placement,
a radio-
November
1997
been
tissue
Table 2
Correlation
11-gauge
of Stereotactic
Vacuum-assisted
Biopsy
Surgical
Stereotactic
Biopsy
Benign
Atypical
Ductal
Findings
ductal
carcinoma
Invasive
Findings
Surgical
Ductal
from
is done
Carcinoma
In Situ
4*
0
0
0
2
0
in situ
2
1
0
0
0
4
0
0
0
6
clip
placement.
the breast
other patient.
Both were clusters
of calcifications
that were 0.9 and 1 .0 cm, respectively,
in the longest
dimension.
cavities
were identified
at surgery but no residual ductal carcinoma
in situ was found.
The biopsy
and
Surgical
Stereotactic
Findings
Ductal
Biopsy
Invasive
Carcinoma
Findings
Benign
Atypical
ductal
hyperplasia
Ductal
car-
14-gauge
ing the
sitioning
14-gauge
Carcinoma
In Situ
0
1
0
cinoma
1
insitu
Invasive
carcinoma
*
Findings
yielded
from
ductal
2
1
0
0
subsequent
surgical
carcinoma
1
excision
obtained
ful guide
the clip
been
ence
force
is entirely
the
error
introducer
needle
the
of
biopsy,
along
compression
of the
of force
maximizes
in the depth
vector
the direction
breast.
This
the likelihood
on z axis.
of
vector
of
Z-axis
en-
rons are potentially
of serious
consequence.
In the compressed
breast,
as
in an accordion,
structures
that are
distant
in the z axis are brought
close
together;
when
compression
is re-
leased,
in situ.
through
14-gauge
structures
gethen
move
farther
small
errors
in the
sion could
translate
when
clip
that
close
to-
apart.
Therefore,
z axis in compresinto larger
errors
compression
placed
were
is released.
through
the
The
11-gauge
probe
is introduced
in an angled
or
“ramped”
configuration,
such that the
vector
of force is not entirely
in the
direction
of compression
(Fig 4). Funthenmore,
the operator
uses vacuum
to pull tissue into the bowl of the probe
rather
out
Figure 4. Photograph
shows the localizing
clip and introducer
inside the 11-gauge
probe. Note that the clip emerges
from the
introducer
ration
tirely
(Image
in a sloped
so that
along
the
courtesy
the vector
or “ramped”
of force
configu-
is not en-
direction
of compression.
of Biopsys
Medical.)
than
Volume
205
Number
#{149}
2
pushing
the clip
into
the tissue.
initial
experience
with
the clip
has taught
us several
lessons.
First,
it
is helpful
to suction
the blood
out of
the biopsy
cavity
and obtain
stereotactic images
after tissue
acquisition
is
complete
to ascertain
whether
the
mammographic
findings
associated
with
the original
lesion
have
been
re-
Our
moved.
graph
can be obtained
of the mastectomy
specimen
to assist the pathologist
in identification
of the biopsy
site.
Clip placement
is more
accurate
through
the 11-gauge
probe
than
through
the introducer
needle
used
after
14-gauge
vacuum-assisted
biopsy.
First,
placement
of the clip after
merely
If so, clip
pniate
(9).
free
of tissue
Second,
placement
the
fragments
is appro-
probe
after
to
has
be-
deployed
that
must
clip
by the two
be
before
placement,
as illustrated
cases
in which
the clip failed
to deploy. Clearing
of tissue
fragments
can
usually
be accomplished
by performing the tap tap maneuver
(3); occasionally,
if clogging
of the probe
has
underwent
it
of
biopsy
and
Observed
distances
clip and lesion
site on
steneotactic
images
may underestimate
the true distances,
particularly
in the
depth
or z axis, owing
to the “accordion
effect”
of compression.
By allowing an assessment
of the location
of
biopsy
necessitates
nemovprobe
from
the breast
and poa new needle.
This reposihoning
allows the possibility
of patient
on lesion
movement,
which
can diminish accuracy.
Second,
when
placing
after
stereo-
be obtained
probe
removal
clip placement.
between
the
the clip
standard
Table 3
Correlation
of Stereotactic
Vacuum-assisted
Biopsy
Surgical Findings
the clip
it, as
procedure,
Third,
should
and
that
flush
of the
fore releasing
compression.
Finally,
is prudent
to obtain
a mammognam
* Includes
one lesion yielding
fibroepithelial
tumor (fibroadenoma
vs phyllodes
tumor)
at stereotactic
biopsy
that was proved
to be a fibroadenoma
at surgery,
one lesion yielding
lobular
carcinoma
in situ at
stereotactic
biopsy
and surgery,
and two lesions yielding
benign
ductal hyperplasia
at stereotactic
biopsy
and benign
findings
at surgery. The latter two lesions were excised during mastectomy
for carcinoma at
a separate
site in one patient
and during breast-conserving
therapy for carcinoma at a separate site in the
t
and
outset
tactic
images
clip placement
ensure
problem
during
we remove
the
the breast
at the
before
Invasive
Carcinoma
hyperplasia
carcinoma
probe
Findings
Atypical
Ductal
Hyperplasia
Benign
and
a substantial
acquisition,
relative
to the biopsy
site
projections,
the mammogram
after
biopsy
for subsequent
on
serves
as a useneedle
local-
ization.
There
are other
tions
of a localizing
addressed
in our
potential
clip
study.
applicathat were
not
There
have
reports
of preliminary
expeniwith magnetic
resonance
(MR)
imaging-guided
localization
One limitation
needle
inability
biopsy
and needle
of breast
lesions
(10-17).
of MR imaging-guided
localization
procedures
to document
lesion
because
contrast
is often
essential
at MR imaging,
resected
placed
is the
retrieval,
enhancement,
which
for lesion
detection
is not observed
in the
specimen.
If a clip
at MR imaging-guided
could
be
biopsy
on localization,
radiography
of the
surgical
specimen
could
confirm
retnieval
of the clip, supporting
successful retrieval
of the lesion.
The clip descnibed
in our study
is compatible
with
a magnet
of field strength
1.5 T
or less; the probe
is not MR imagingcompatible,
but clip placement
could
occur outside
the magnet
after placement
of an MR imaging-compatible
introducer
(15,16).
Edeiken-Monroe
al (18) reported
preliminary
experi-
ence
with
sonographically
guided
et
im-
plantation
of metallic
markers
to permanently
localize
the tumor
bed in
patients
with
breast
cancer
receiving
preoperative
chemotherapy.
In eight
(42%)
of 19 cases,
the metallic
marker
was the only
remaining
evidence
of
the site of the tumor
bed.
A localizing
clip could
therefore
be useful
the tumor
site in these
women
locally
advanced
breast
cancer.
Mumtaz
et al (19) described
neous
treatment
interstitial
laser
The
role
cedunes
cen has
placement
to mark
with
percuta-
of breast
cancers
photocoagulation.
of percutaneous
ablative
in the treatment
of breast
not been
established,
but
of a localizing
marker
Rt4nh,ft,
with
procanat
#{149}
LV)1
the tumor
site
could
play
a role
in this
3.
evolving
technique.
It may be necessary to improve
on the accuracy
of
marker
placement
over
that reported
in our
study
for use
4.
in guiding
In summary,
a localizing
proximity
reotactic
our data demonstrate
clip can be placed
to the biopsy
vacuum-assisted
placement
is more
the 11-gauge
probe
gauge
biopsy.
the biopsy
subsequent
the
ated
been
After
site
site
after
biopsy.
mammognaphic
steClip
6.
excision,
findings
with the original
lesion
removed
completely.
7.
for
even
if
associ-
have
#{149}
8.
Acknowledgments:
We thank Lynda T. Zingaro, RT(R)(M), and Youngduk
Paik, RT(R)(M),
for expert technical
support
and David C. Perlman,
MD, for invaluable
assistance.
9.
References
1.
Parker
SH, Burbank
F.
A practical
proach
to minimally
invasive
Radiology
1996; 200:11-20.
2.
Burbank
F.
Stereotactic
breast
Parker SH, Stavros AT, Dennis
15.
10.
ap-
breast
biopsy
of
vesting
with the Mammotome.
1996; 62:738-744.
KaneJW,
Sternheim
MM.
Needle
North
Burbank F, Parker SH, Fogarty
tactic breast biopsy: improved
TJ. Stereotissue harAm
Plane
functions.
Viehweg P, Schaumloffel
U, Heske N. Ein
neues nadelsystem
zur MR-gestuzten
loka-
Am
Surg
16.
geometry
In: Physics.
New York, NY: Wiley, 1978; 627.
Jackman
RJ, Burbank
F, Parker
SH, et al.
Atypical
ductal hyperplasia
diagnosed
at
stereotactic
breast biopsy: improved
reliability
with 14-gauge, directional,
vacuumassisted
biopsy.
Radiology
1997; 204:485488.
MeyerJE,
Smith
DN, DiPiro
PJ, et al.
17.
Ste-
18.
lisation
und
pekten
defunden
19.
transkutanen
biopsie
von susin der brust:
in-vitrobei 1.0 Tesla. ROFO
1997;
untersuchungen
166:342-345.
Heywang-Kobrunner
SH,
Kolem
H, Heinig
A, Viehweg P. A new design for a breast
biopsy device suitable for MR application
(abstr).
Eur Radiol 1997; 7(suppl):243.
Kuhl CK, Elevelt
A, Leutner
CC, GiesekeJ,
Pakos E, Schild HH.
Interventional
breast
MR imaging:
clinical
use of a stereotactic
localization
and
1997; 204:667-675.
Edeiken-Monroe
FA.
reotactic
breast biopsy of clustered
microcalcifications
with a directional,
vacuumassisted
device.
Radiology
1997; 204:575576.
Burbank
F. Mammographic
findings
after
14-gauge
automated
needle
and 14-gauge
directional,
vacuum-assisted
stereotactic
breast
biopsies.
Radiology
1997; 204:153156.
Heywang-Kobrunner
SH, Beck R, Hilbertz
11.
ogy 1990; 177:190-191.
Fischer
U, Vosshenrich
MR-guided
A preliminary
biopsy
device.
BS, Fomage
report
Radiology
BD, Holmes
of sonographi-
cally guided
implantation
of metallic
markers to permanently
localize
the tumor
bed
in patients
with breast
cancer
receiving
preoperative
chemotherapy
(abstr). AJR 1997;
168(suppl):98.
Mumtaz
H, Hal!-Craggs
MA, Wotherspoon
A, et al. Laser therapy for breast cancer:
MR imaging and histopathologic
correlalion. Radiology
1996; 200:651-658.
12.
13.
biopsy
R, Keating
of suspect
D, et al.
breast
lesions
with a simple
stereotaxic
add-on
device
for
surface
coils. Radiology
1994; 192:272-273.
Ore! SC, Schnall
MD, Newman
RW, Powell
CM, Torosian
MH, Rosato
EF.
MR imag-
ing-guided
localization
and biopsy
of
breast
lesions:
initial experience.
Radiology
1994; 193:97-102.
Ore! SC, Schnall
MD, Powell
CM, et al.
Staging
of suspected
breast
cancer:
effect
MR imaging
ology
#{149}
Radiology
MA.
Chin
Brenner
RJ, Shellock
FG, Rothman
BJ, Giuliano A.
Magnetic
resonance
imagingguided
preoperative
breast localization
using freehand
technique.
BrJ Radio!
1995;
68:1095-1098.
Heinig
A, Heywang-Kobrunner
SH,
T, et al. Needle localization
of breast leslons detected
with MR imaging. Radiol-
biopsy.
atypical
ductal
hyperplasia
and ductal
carcinoma
in situ lesions:
improved
accuracy
with directional,
vacuum-assisted
breast
biopsy.
Radiology
1997; 202:843-847.
422
Radiol
and trigonometric
placement,
can be identified
surgical
5.
in
accurate
through
than after 14clip
14.
biopsy
techniques.
1995; 33:1171-1186.
therapy.
that
Liberman
L, Hann
LE, Dershaw
DD, Morris EA, Abramson
AF, Rosen
PP.
Mammographic
findings
after stereotactic
14-gauge
vacuum
biopsy.
Radiology
1997; 203:343347.
1995;
and MR-guided
biopsy.
of
Radi-
196:115-122.
November
1997