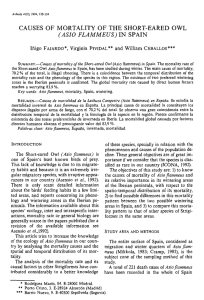
PREVENTIVE CARDIOLOGY SUMMER 2005 167 REVIEW PAPER • CME Heart Rate Recovery After Exercise and Endothelial Function—Two Important Factors to Predict Cardiovascular Events Po-Hsun Huang, MD;1 Hsin-Bang Leu, MD;1 Jaw-Wen Chen, MD;1,2 Shing-Jong Lin, MD, PhD1,2,3 An attenuated heart rate recovery immediately after exercise, thought to be a marker of reduced parasympathetic activity, has been demonstrated to be an independent predictor of all-cause mortality in several large-scale studies; however, the mechanisms by which impaired heart rate recovery confers an increased risk of death are not clear. From clinical observation, vagal reactivation was thought to be the major determinant of the decrease in heart rate during the first 30 seconds of recovery, independent of age and the intensity of exercise; however, patients with attenuated heart rate recovery were also shown to have lower exercise workload, shorter exercise duration, lower numbers achieving 90% target heart rate, and even impaired endothelial function. This review focuses on the roles of heart rate recovery and endothelial function in predicting future mortality and their interaction. (Prev Cardiol. 2005;8:167–170) ©2005 Le Jacq Ltd. O ver the past few years, several large clinical studies have clearly demonstrated the potential value of heart-rate recovery (HRR) immediately after exercise as a simple and valuable tool for predicting clinical events and mortality.1–5 During 6 years of follow-up, Cole et al.1 showed, in a large-scale study of 2428 subjects (mean [±SD] age, 57±12 years; 63% men) without a history of heart From the Division of Cardiology, Department of Internal Medicine, Taipei Veterans General Hospital, Taipei, Taiwan;1 the Cardiovascular Research Center,2 and the Institute of Clinical Medicine,3 National Yang-Ming University, Taipei, Taiwan Address for correspondence: Shing-Jong Lin, MD, PhD, Division of Cardiology, Taipei Veterans General Hospital, No. 201, Sec. 2, Shih-Pai Road, Taipei, Taiwan E-mail: sjlin@vghtpe.gov.tw Manuscript received July 7, 2004; revised December 22, 2004; accepted January 7, 2005 www.lejacq.com ID: 3847 failure or coronary revasculization, that a low value of HRR was a strong predictor of death in a number of important subgroups, including the elderly, women, patients with normal chronotropic response during exercise, and even those taking β blockers. In another large cohort study of 9454 subjects (mean [±SD] age, 53±11 years; 78% men) referred for exercise electrocardiography, HRR was shown to provide prognostic information additional to the established treadmill exercise score.2 After adjusting for age, sex, exercise capacity, left ventricular systolic function, presence or absence of myocardial ischemia, and other confounders, an abnormal HRR remained predictive of death (adjusted hazard ratio, 2.09; 95% confidence interval, 1.49–2.82; p<0.001).4 Patients who had both a normal chronotropic response during exercise and a normal HRR had a 6-year mortality rate of only 3%, or 0.5% per year.1 In the Framingham Heart Study,5 which included a younger population (mean age, 43 years), very rapid HRR immediately after exercise was shown to be associated with lower risk of coronary heart disease and cardiovascular disease, but not related to all-cause mortality. To date, most of the clinical trials seem to support the prognostic value of HRR after exercise to predict future mortality and cardiac events (Table). A reduction in the heart rate of 12 or fewer beats in the first minute after the cessation of exercise was used as the definition of a low value for HRR in several of the large-scale studies.1,2,4 This value was determined by calculating the maximal value for the log-rank chi-square test statistic between the 10th and 90th percentiles. In fact, there is no agreed-upon cutoff value for abnormal HRR in the literature. Some studies have used ≤12 bpm, and others have adopted ≤18 bpm.1,2,4,5 If 12 bpm is used as the cutoff value, the specificity and positive predictive rate for prediction of mortality and cardiovascular events are improved. When HRR decreased less than 12 beats in the first minute after exercise, risk of mortality increased markedly. The studies varied in types of exercise protocol, and several studies included a 2-minute cool-down period.1,2,4 This period was considered a recovery period. However, the impact of these features—with Preventive Cardiology (ISSN 1520-037X) is published quarterly (Feb., April, June, Sept.) by Le Jacq Ltd., Three Parklands Drive, Darien, CT 06820-3652. Copyright ©2005 by Le jacq Ltd. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without permission in writing from the publishers. The opinions and ideas expressed in this publication are those of the authors and do not necessarily reflect those of the Editors or Publisher. For copies in excess of 25 or for commercial purposes, please contact Sarah Howell at showell@lejacq.com or 203.656.1711 x106. 168 SUMMER 2005 PREVENTIVE CARDIOLOGY Table. Previously Published Prognostic Studies of Abnormal Heart-Rate Recovery7 Enrolled (N) Mean age (yr) Mean followup (yr) Men (%) Asymptomatic (%) History of PCI (%) History of CABG (%) Protocol Cool-down exercise Heart-rate recovery “low” limit (bpm) Main finding Comments COLE ET AL.1 2428 57 6 NISHIME ET AL.2 9454 53 5.2 DIAZ ET AL.3 5234 44 12 WATANABE ET AL.4 7163 60 6.7 MORSHEDI-MEIBODI ET AL.5 5438 57 3 SHETLER ET AL.6 2193 59 6.8 63 NA 78 75 61 100 75 NA 63 NA 100 0 0 NA 0 17 13 0 0 8 0 24 14 0 Bruce symptomlimited Bruce symptomlimited Bruce symptomlimited Variable Ramp Yes Yes Bruce 85% agepredicted heart rate No Yes No (left decubitus position) No (supine) ≤12 in 1 min ≤12 in 1 min ≤42 in 2 min ≤12 in 1 min ≤18 in 1 min ≤22 in 2 min HRR is a powerful predictor of overall mortality HRR and treadmill exercise score were independent predictors of mortality Abnormal HRR predicts death even after submaximal exercise HRR is an independent predictor of death even in the absence of a cool-down period HRR at 1 or 2 min was validated as a prognostic measurement No effect of β-blocker use Not predictive of death among patients taking β blockers β blockers excluded Enhanced risk stratification of exercise nuclear imaging when HRR and exercise capacity are considered No No prognostic effect of ischemia No effect of β-blocker use, no prognostic effect of ischemia NA=not available; PCI=percutaneous coronary intervention; CABG=coronary artery bypass graft surgery; HRR=heart rate recovery or without a cool-down period—on the prognostic value of HRR after exercise remains uncertain. AUTONOMIC CONTROL OF HRR The exact mechanisms by which attenuated HRR is associated with an increased risk of death are not yet understood. Previous studies had shown that the autonomic system plays a central role in regulating cardiovascular function in both healthy and diseased populations. Augmented reflex sympathetic activity to the heart can precipitate cardiac arrhythmia, but activation of parasympathetic reflexes may contribute to cardiac electrical stability. Patients with congestive heart failure have an activated sympathetic nervous system to compensate for the reduction in cardiac output, and plasma norepinephrine provides a sensitive index of the activity of the sympathetic nervous system and is highly predictive of subsequent mortality.8–11 It is known that beat-to-beat fluctuations in the heart rate are under autonomic control, and thus heart-rate variability (HRV) can provide insight into parasympathetic and sympathetic influences on the sinus node. HRV can be measured in the time and/or frequency domain during shortterm (10 minute) and long-term (24 hour) Holter recordings. A high degree of HRV is found in compensated hearts with good function, whereas HRV can be decreased with severe coronary artery Preventive Cardiology (ISSN 1520-037X) is published quarterly (Feb., April, June, Sept.) by Le Jacq Ltd., Three Parklands Drive, Darien, CT 06820-3652. Copyright ©2005 by Le jacq Ltd. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without permission in writing from the publishers. The opinions and ideas expressed in this publication are those of the authors and do not necessarily reflect those of the Editors or Publisher. For copies in excess of 25 or for commercial purposes, please contact Sarah Howell at showell@lejacq.com or 203.656.1711 x106. SUMMER 2005 disease, congestive heart failure, aging, and diabetic neuropathy.12 In the Framingham Heart Study, Tsuji et al.13 showed that the estimation of HRV by ambulatory monitoring offers prognostic information beyond that provided by the evaluation of traditional cardiovascular disease risk factors. Another method used to evaluate autonomic function is baroreflex sensitivity. The underlying concept is to study the reflex heart-rate response to physiologic activation or inhibition of the baroreceptors secondary to drug-induced changes in arterial pressure. Overall, baroreflex sensitivity decreases whenever the autonomic balance shifts toward sympathetic activation and increases whenever the autonomic balance shifts toward parasympathetic dominance. La Rovere et al.14 showed that markers of HRV and baroreflex sensitivity were both strong predictors of outcome in patients with myocardial infarctions. These clinical data clearly demonstrated the relationship of enhanced sympathetic activity and mortality. Numerous methods are available to assess sympathetic activity, but techniques for evaluating parasympathetic activity and its clinical implications are more limited. It has been suggested that the link between HRR and mortality may be related to vagal tone and physical fitness. Based on studies of normal individuals with and without autonomic blockade, Savin et al.15 initially postulated that “sympathetic withdrawal contributes more to HRR soon after peak exercise, with parasympathetic activation playing a greater role later in recovery at lower heart rates.” Their data, however, also showed a slower HRR after parasympathetic blockade (atropine) infusion than without it, suggesting an important role for parasympathetic reactivation in early HRR. Crouse et al.16 found initial heart-rate kinetics post-exercise to be unaffected by β blockade. These findings imply that sympathetic activity withdrawal does not contribute significantly to initial HRR after exercise termination. Thereafter, Imai et al.17 examined the physiologic characteristics of HRR after exercise in healthy adults, athletes, and patients with chronic heart failure. They found that beat-to-beat heart-rate decay for the first 30 seconds and the first 120 seconds were markedly prolonged by atropine administration in normal volunteers, indicating that both time constants are mainly regulated by vagal reactivation. Moreover, beat-tobeat heart-rate decay for the first 30 seconds was almost independent of the exercise intensity and sympathetic blockade, whereas the change at 120 seconds was affected by sympathetic nerve activity and exercise work load. These results clearly indicated that beat-to-beat heart-rate decay for the first 30 seconds is mediated primarily by vagal reactivation, independent of sympathetic withdrawal. Vagally mediated HRR after exercise was accelerated in well-trained athletes, but blunted in patients with chronic heart failure.17 Pierpont et al.18 tested PREVENTIVE CARDIOLOGY 169 the time constant obtained by fitting post-exercise HRR to a first-order exponential decay curve as an index of parasympathetic activity, and proved again that HRR immediately post-exercise was a useful index of parasympathetic activity. ENDOTHELIAL FUNCTION AND INTERACTION WITH AUTONOMIC FUNCTION The endothelium is a complex endocrine and paracrine organ that affects vascular tone, smooth muscle cell proliferation, platelet aggregation, monocyte and leukocyte adhesion, and thrombosis. Endothelial function plays a key role in determining the clinical manifestations of established atherosclerotic lesions and cardiovascular events.19 All major risk factors for atherosclerosis, such as hyperlipidemia, diabetes, hypertension, and smoking, are associated with impaired endothelial function. Clinically, endothelial function is most often assessed as a vasodilator response to pharmacologic or mechanical stimulation. Coronary endothelial vasodilator dysfunction has been shown to be related to long-term atherosclerotic disease progression and cardiovascular event rates.20 Impaired flow-mediated vasodilation (FMD) in the brachial artery has been proved to be closely correlated with endothelial dysfunction in coronary artery disease, suggesting that endothelium-dependent vasodilation impairment is a generalized atherosclerotic process.21,22 Several reports have presented data on the interaction between the sympathetic nervous system and endothelial function. Hijmering et al.23 tested the hypothesis that increased sympathetic outflow may interfere with endothelium-dependent FMD. Pathophysiologically relevant sympathetic stimulation was achieved by baroreceptor unloading, using a lower-body negative-pressure box. The investigators demonstrated that increased sympathetic activation could markedly suppress endothelium-dependent FMD in healthy adults. They mentioned a specific inhibitory effect of sympathetic activation on shear-mediated NO release. Research with animal models has also demonstrated that chronic sympathetic arousal was associated with endothelial injury, which could be prevented by β-adrenergic blocking agents.24,25 Pettersson et al.25 tested the hypothesis that sympathetic activation might lead to an increase in endothelial injury. They used chloralose anesthesia to induce sympathetic activation in normal rabbits, and found an approximate five-fold increase in the number of injured endothelial cells in unbranched and circumostial areas of the rabbits’ thoracic aortae. This injury was greatly inhibited by pretreatment with metoprolol, indicating that sympathetic activation-induced endothelial injury was mediated by β1 adrenergic receptors. Hemodynamic mechanisms— including endothelium cell injury due to intermittent or long-term increased shear stress and alteration of Preventive Cardiology (ISSN 1520-037X) is published quarterly (Feb., April, June, Sept.) by Le Jacq Ltd., Three Parklands Drive, Darien, CT 06820-3652. Copyright ©2005 by Le jacq Ltd. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without permission in writing from the publishers. The opinions and ideas expressed in this publication are those of the authors and do not necessarily reflect those of the Editors or Publisher. For copies in excess of 25 or for commercial purposes, please contact Sarah Howell at showell@lejacq.com or 203.656.1711 x106. 170 PREVENTIVE CARDIOLOGY flow pattern with impact mainly in the large arteries—may account for the typical target organ damage observed in hypertension and is involved in the development of atherosclerotic lesions.26,27 Few reports have explored the relationship between decreased vagal activity and endothelial function—especially in patients with attenuated HRR after graded exercise. Recently, we reported28 clinical data showing a significant relation between the extent of HRR and endothelial function. Sixtysix patients with suspected coronary artery disease were enrolled, and a noninvasive method of brachial ultrasound was used to measure endotheliumdependent FMD and endothelium-independent nitroglycerin-mediated vasodilation. In the study, patients with attenuated HRR were shown to have significantly lower exercise workload, lower numbers achieving 90% target heart rate, shorter exercise duration, and even lower endotheliumdependent FMD. After multivariate analysis, HRR remained an independent predictor of endothelial dysfunction after adjustment for age, sex, smoking history, exercise habits, hypertension, diabetes mellitus, medications, and lipid profiles. These findings suggested that autonomic function plays a key role in the process of atherosclerosis, and may partly explain why subjects with abnormal HRR have more cardiovascular events or increased mortality. CONCLUSIONS It is now widely recognized that both HRR and endothelial function are independent predictors of the risk of death and have usefulness in clinical application. Although the underlying mechanisms of the reduced endothelial function are multifactorial, more and more data have shown the critical role of autonomic dysfunction in the pathogenesis of atherosclerosis. Future research is needed to determine how to manage patients with abnormal HRR and make clear the true mechanism and role of the autonomic system in modulating the shear stress-mediated pathway. REFERENCES 1 Cole CR, Blackstone EH, Pashkow FJ, et al. Heart-rate recovery immediately after exercise as a predictor of mortality. N Engl J Med. 1999;341:1351–1357. 2 Nishime EO, Cole CR, Blackstone EH, et al. Heart rate recovery and treadmill exercise score as predictors of mortality in patients referred for exercise ECG. JAMA. 2000;284:1392–1398. 3 Diaz LA, Brunken RC, Blackstone EH, et al. Independent contribution of myocardial perfusion defects to exercise capacity and heart rate recovery for prediction of all-cause mortality in patients with known or suspected coronary heart disease. J Am Coll Cardiol. 2001;37:1558–1564. 4 Watanabe J, Thamilarasan M, Blackstone EH, et al. Heart rate recovery immediately after treadmill exercise and left ventricular systolic function as predictors of mortality: the case of stress echocardiography. Circulation. 2001;104:1911–1916. 5 Morshedi-Meibodi AM, Larson MG, Levy D, et al. Heart rate recovery after treadmill exercise testing and risk of cardiovascular disease events (The Framingham Heart Study). Am J Cardiol. 2002;90:848–852. SUMMER 2005 6 Shetler K, Marcus R, Froelicher VF, et al. Heart rate recovery: validation and methodologic issues. J Am Coll Cardiol. 2001;38:1980–1987. 7 Gibbons RJ. Abnormal heart-rate recovery after exercise. Lancet. 2002;359:1536–1537. 8 Cohn JN, Levine TB, Olivari MT, et al. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med. 1984;311:819–823. 9 Robertson D, Johnson GA, Robertson RM, et al. Comparative assessment of stimuli that release neuronal and adrenomedullary catecholamines in man. Circulation. 1979;59:637–643. 10 Lake CR, Ziegler MG, Kopin IJ. Use of plasma norepinephrine for evaluation of sympathetic neural function in man. Life Sci. 1976;18:1315–1326. 11 Kopin IJ, Lake CR, Ziegler MG. Plasma levels of norepinephrine. Ann Intern Med. 1978;88:671–680. 12 Kleiger RE, Miller JP, Bigger JT, et al. Decreased heart rate variability and its association with increased mortality after acute myocardial infraction. Am J Cardiol. 1987;59:256–262. 13 Tsuji H, Venditti FJ, Manders ES, et al. Reduced heart rate variability and mortality risk in an elderly cohort. The Framingham Heart Study. Circulation. 1994;90:878–883. 14 La Rovere MT, Bigger JT Jr, Marcus FI, et al. Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. Lancet. 1998;351:478–484. 15 Savin WM, Davidson DM, Haskell WL. Autonomic contribution to heart rate recovery from exercise in humans. J Appl Physiol. 1982;53:1572–1575. 16 Crouse SF, Sterling J, Tolson H, et al. The effect of betaadrenergic blockade on heart rate recovery from exercise. J Cardiopulm Rehabil. 1989;9:202–206. 17 Imai K, Sato H, Hori M, et al. Vagally mediated heart rate recovery after exercise is accelerated in athletes but blunted in patients with chronic heart failure. J Am Coll Cardiol. 1994;24:1529–1535. 18 Pierpont GL, Stolpman DR, Gornick CC. Heart rate recovery post-exercise as an index of parasympahtetic activity. J Auton Nerv Syst. 2000;80:169–174. 19 Fuster V, Badimon L, Badimon JJ, et al. The pathogenesis of coronary artery disease and the acute coronary syndrome. N Engl J Med. 1992;326:310–318. 20 Schachinger V, Britten MB, Zeiher AM. Prognostic impact of coronary vasodilator dysfunction on adverse longterm outcome of coronary heart disease. Circulation. 2000;101:1899–1906. 21 Anderson TJ, Uehata A, Gerhard MD, et al. Close relation of endothelial function in the human coronary and peripheral circulation. J Am Coll Cardiol. 1995;26:1235–1241. 22 Celermajer DS, Sorensen KE, Bull C, et al. Endotheliumdependent dilation in the systemic arteries of asymptomatic subjects related to coronary risk factors and their interaction. J Am Coll Cardiol. 1994;24:1468–1474. 23 Hijmering ML, Stroes ES, Olijhoek J, et al. Sympathetic activation markedly reduces endothelium-dependent, flow-mediated vasodilation. J Am Coll Cardiol. 2002;39:683–688. 24 Ablad B, Bjorkman JA, Gustaffson D, et al. The role of sympathetic activation in atherosclerosis: effects of betablockade. Am Heart J. 1988;116:322–327. 25 Pettersson K, Bejne B, Bjork H, et al. Experimental sympathetic activation causes endothelial injury in the rabbit thoracic aorta via beta 1-adrenoceptor activation. Circ Res. 1990;67:1027–1034. 26 Kaplan JR, Manuck SB. Antiatherogenic effects of beta-adrenergic blocking agents: theoretical, experimental, and epidemiologic considerations. Am Heart J. 1994;128:1316–1328. 27 Pauletto P, Scannapieco G, Pessina AC. Sympathetic drive and vascular damage in hypertension and atherosclerosis. Hypertension. 1991;17(4 suppl):III75–81. 28 Huang PH, Leu HB, Chen JW, et al. Usefulness of attenuated heart rate recovery immediately after exercise to predict endothelial dysfunction in patients with suspected coronary artery disease. Am J Cardiol. 2004;93:10–13. Preventive Cardiology (ISSN 1520-037X) is published quarterly (Feb., April, June, Sept.) by Le Jacq Ltd., Three Parklands Drive, Darien, CT 06820-3652. Copyright ©2005 by Le jacq Ltd. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without permission in writing from the publishers. The opinions and ideas expressed in this publication are those of the authors and do not necessarily reflect those of the Editors or Publisher. For copies in excess of 25 or for commercial purposes, please contact Sarah Howell at showell@lejacq.com or 203.656.1711 x106. PREVENTIVE CARDIOLOGY SUMMER 2005 171 CME QUESTIONS AND ANSWERS Insert your answers on the response page 1. Which of the following is true regarding postexercise heart rate recovery (HRR)? A. All studies of HRR show that it predicts allcause mortality B. HRR has been found to be a prognostic factor in women C. HRR predicts mortality in patients taking β-blocking drugs during exercise testing D. None of the above 3. Which of the following statements is/are true? A. Diabetes is the only cardiac risk factor not associated with impaired endothelial function B. Endothelium-dependent vasodilation of the brachial artery correlates poorly with coronary artery endothelium-dependent vasodilation C. Recent evidence suggests a correlation between low HRR and impaired endothelial function D. B and C 2. All of the following statements are true except: A. In current studies, HRR values between <12 and <18 bpm have been variously considered abnormal B. Elevated plasma norepinephrine predicts increased mortality in patients with heart failure C. High heart rate variability is an indicator of cardiac electrical instability D. Heart rate variability decreases with aging ACCREDITATION: The University of California, Davis, Health System is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to sponsor continuing medical education for physicians. This activity has been planned and implemented in accordance with the Essential Areas and Policies of the ACCME through the joint sponsorship of Oakstone Medical Publishing and Continuing Medical Education, UC Davis Health System. This CME activity was planned in accordance with the ACCME essentials for enduring materials. Length of time has been determined to be 1 hour. Please read the date of release and date of approval. PHYSICIAN CREDIT: Continuing Medical Education at the University of California, Davis, Health System designates this continuing medical education for 1 hour in Category 1 of the Physician’s Recognition Award of the American Medical Association and the Certification Program of the California Medical Association. No partial credit is allowed for this CME activity. FACULTY DISCLOSURE: In accordance with standards of the ACCME and the guidelines of the Association of American Medical Colleges, the authors of this material have been asked to disclose any real or apparent conflicts of interest which may have a direct bearing on the subject matter presented. Authors are expected to disclose: 1) any significant financial interests or other relationships with manufacturers of commercial products and/or providers of commercial services discussed in their presentations; and 2) any “off-label” uses for pharmaceutical or medical device products discussed in their materials. The intent of this disclosure is not to prevent authors with significant financial or other relationships from making presentations, but rather to provide participants with information with which they can make their own judgments. AUTHOR DISCLOSURE: The authors have no commercial relationships to disclose. HOW TO OBTAIN CME CREDIT: To obtain CME credit, the University of California, Davis, Health System, Continuing Medical Education requires that you complete and return the answer sheet and program evaluation form with a check for $25, or you may fax the materials with Visa/MasterCard information for payment. Checks should be made payable to Regents of the University of California and mailed to: Continuing Medical Education, UC Davis Health System, 3560 Business Drive, Suite 130, Sacramento, CA 95820. To pay by Visa/Mastercard, please complete the entire application to include credit card number, expiration date and name of cardholder. You may fax this information to (916) 736-0188. Upon completion of the above, your certificate of credit will be mailed to you within 4 weeks. All required information for enduring materials are located at the Office of Continuing Medical Education, UC Davis Health System, 3560 Business Drive, Suite 130, Sacramento, CA 95820. Any questions about this process may be directed to Pamela Stotlar-McAuliffe at (916) 734-5393; pamela.stotlar-mcauliffe@ucdmc. ucdavis.edu. FACULTY ADVISOR: Ezra A. Amsterdam, MD, Professor of Medicine, Division of Cardiovascular Medicine, University of California, Davis, School of Medicine, and Director, Cardiac Care Unit, University of California, Davis, Medical Center, Sacramento, CA OBJECTIVE AND TARGET AUDIENCE: All primary care physicians and cardiologists are eligible to receive credit. At the conclusion of this activity, participants should be able to: 1) summarize the important points discussed in the paper reviewed; 2) identify patients to whom the paper is relevant; 3) modify management practices as new information is learned; and 4) identify deficiencies in their knowledge base. CME Answers are available on the Preventive Cardiology page at www.lejacq.com Preventive Cardiology (ISSN 1520-037X) is published quarterly (Feb., April, June, Sept.) by Le Jacq Ltd., Three Parklands Drive, Darien, CT 06820-3652. Copyright ©2005 by Le jacq Ltd. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without permission in writing from the publishers. The opinions and ideas expressed in this publication are those of the authors and do not necessarily reflect those of the Editors or Publisher. For copies in excess of 25 or for commercial purposes, please contact Sarah Howell at showell@lejacq.com or 203.656.1711 x106. 172 SUMMER 2005 PREVENTIVE CARDIOLOGY INSTRUCTIONS: In order to complete this educational activity successfully, you must: o Complete the post-test. o Complete the program evaluation form. o Enclose a check for $25 payable to: Regents of the University of California or o Submit Visa/MasterCard information. o Mail or fax your completed answer sheet and check to: Continuing Medical Education, UC Davis Health System, 3560 Business Drive, Suite 130, Sacramento, CA 95820; fax: 916-736-0188 In order to receive CME credit, the answer sheet must be received by June 2007. Thank you PROGRAM EVALUATION 1. Did the material presented in this educational activity 4. Please describe any changes you plan to make in your meet the stated learning objectives? o Yes clinical practice based on the information presented in this program. _________________________________ o No ______________________________________________________ 2. Please rate the contents of this activity using the follow- 5. Did you detect any commercial bias in this activity? ing scale: o Yes o No If yes, please describe: __________________________________ _____________________________________________________ _____________________________________________________ 1=Poor; 2=Fair; 3=Good; 4=Very Good; 5=Excellent (circle the response for each question) Poor Excellent Timely and up-to-date? 1 2 3 4 5 1 2 3 4 5 Practical? Relevant to your practice? 1 2 3 4 5 6. Any other comments/suggestions for future educational activities relating to preventive cardiology? 3. Are there any other topics you would like to have seen _____________________________________________________ _____________________________________________________ _____________________________________________________ addressed in this activity? o Yes (please specify): _____________________________ o No POST-TEST RESPONSES (Please check the single BEST answer) 1. 2. 3. A___ A___ A___ B___ B___ B___ C___ C___ C___ D___ D___ D___ Please type or print clearly: Re: Huang P-H, Leu H-B, Chen J-W, et al. Heart rate recovery after exercise and endothelial function—two important factors to predict cardiovascular events. Prev Cardiol. 2005;8:167–170. Name: First Last Specialty Degree Street address City State ZIP code Office phone with area code Signature Please check your payment method: Account Number Social Security # (for transcript purposes only) Date o Check payable to: Regents of the University of California o Visa o MasterCard Expiration date Authorized signature Preventive Cardiology (ISSN 1520-037X) is published quarterly (Feb., April, June, Sept.) by Le Jacq Ltd., Three Parklands Drive, Darien, CT 06820-3652. Copyright ©2005 by Le jacq Ltd. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without permission in writing from the publishers. The opinions and ideas expressed in this publication are those of the authors and do not necessarily reflect those of the Editors or Publisher. For copies in excess of 25 or for commercial purposes, please contact Sarah Howell at showell@lejacq.com or 203.656.1711 x106.