Forearm Strap vs. Wrist Splint for Lateral Epicondylitis
Anuncio

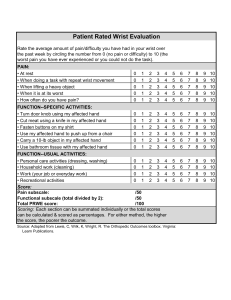
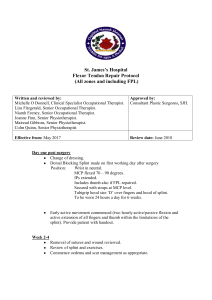
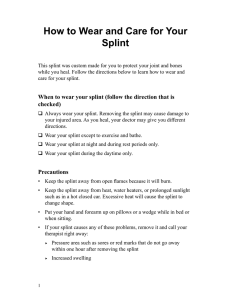
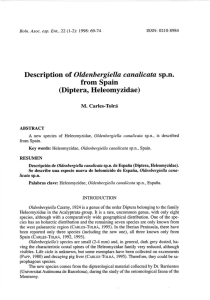
J Shoulder Elbow Surg (2010) 19, 508-512 www.elsevier.com/locate/ymse A prospective randomized study comparing a forearm strap brace versus a wrist splint for the treatment of lateral epicondylitis Rishi Garg, MDa, Gregory J. Adamson, MDb,*, Patrick A. Dawson, MDb, James A. Shankwiler, MDb, Marilyn M. Pink, PhDb a b West Coast Orthopaedics, Arcadia, CA Congress Medical Associates, Pasadena, CA Background: The outcome is unknown for 2 common bracing treatments utilized for patients with lateral epicondylitis. The purpose of this study was to compare the clinical outcomes of a wrist splint with that of a counterforce forearm strap for the management of acute lateral epicondylitis. Materials and methods: Forty-two patients (44 elbows) received either a wrist extension splint (Group I24 elbows) or a counterforce forearm strap (Group II-20 elbows). Measures on the Mayo Elbow Performance (MEP) and American Shoulder and Elbow Society (ASES) Elbow Assessment Form were collected prior to treatment and at 6 weeks. A total score was derived, utilizing the ASES Elbow Assessment, as was a score utilizing the standard scoring system for the MEP. Results: Group I’s score derived from the ASES form improved 16 points and Group II’s score improved 13 points. Group I’s score on the MEP improved 13 points and Group II’s score improved 12 points. There was no significant difference measured between the Groups with the ASES (P ¼ .60) nor MEP (P ¼ .63) scores. However, within the ASES derived score, pain relief was significantly better with the extension splint group (P ¼ .027). No other variables were statistically significantly different. Discussion: Significant pain relief with the wrist extension splint may be due to improved immobilization of the wrist extensor muscles in a resting position. Conclusion: The wrist extension splint allows a greater degree of pain relief than does the forearm strap brace for patients with lateral epicondylitis. Level of evidence: Level II, Randomized Control Study, Lesser Follow-Up, Treatment Study. Ó 2010 Journal of Shoulder and Elbow Surgery Board of Trustees. Keywords: Elbow; lateral epicondylitis; forearm strap brace; wrist splint With a reported annual incidence of 1% to 3% in the general population, lateral epicondylitis, or ‘‘tennis elbow,’’ is the most common cause of lateral elbow pain.5 The authors received IRB approval #HMH04-37 at our institution Huntington Memorial Hospital. *Reprint requests: Gregory J. Adamson, MD, Congress Medical Associates, 800 S Raymond Ave., 2nd Floor, Pasadena, CA 91105. E-mail address: cagjamd@aol.com (G.J. Adamson). Somewhat of a misnomer, ‘‘tennis elbow’’ actually occurs in fewer than 5% to 10% of tennis players.2,6 Lateral epicondylitis, like most other tendinopathies, typically occurs during the 4th and 5th decades of life. It is caused by inflammation of the common extensor origin on the lateral epicondyle of the humerus, with resultant microtears and histologic changes of angiofibroblastic hyperplasia.15 The extensor carpi radialis brevis (ECRB) and the extensor 1058-2746/2010/$36.00 - see front matter Ó 2010 Journal of Shoulder and Elbow Surgery Board of Trustees. doi:10.1016/j.jse.2009.12.015 Lateral epicondylitis: brace vs splint digitorum communis (EDC) have been implicated as the most commonly affected tendons. Symptoms of lateral elbow pain, aggravated by active wrist extension, supination, and power grip are common. Conservative treatment strategies have been directed at relieving inflammation through rest, icing, activity modifications, NSAIDs, splints, injections, and, more recently, extracorporeal shock wave therapy. Nonoperative treatment of lateral epicondylitis is successful in 70-80% of cases at 1 year.4 Two popular methods of bracing include a forearm counterforce strap and a wrist extension splint. The forearm counterforce strap is placed around the muscle bellies of the wrist extensors just distal to the elbow, while an extension splint is placed on the wrist. The orthopaedic literature is lacking in studies directly comparing the efficacy of wrist splinting with forearm counterforce strap bracing for this condition. The purpose of our study was to compare the clinical outcome of a wrist splint with a forearm counterforce strap brace for the management of acute lateral epicondylitis. 509 Figure 1 Hely and Weber wrist extension splint. Materials and methods This prospective randomized investigation was approved by the Institutional Review Board at our institution prior to enrollment of patients. Between 2005 and 2008, 509 consecutive patients presenting to our office with symptoms of acute lateral epicondylitis were evaluated for inclusion in the study. Patients were included if they met the diagnostic criteria of lateral sided elbow pain, tenderness to palpation over the lateral extensor origin, and pain with resisted wrist and long finger extension. Those who had received prior treatments such as physical therapy, bracing, or steroid injections within the last 6 months were excluded. Additionally, patients with cervical radiculitis or compressive neuropathies in the involved extremity were excluded. Standard anteroposterior and lateral radiographs were obtained to further assure that patients did not have alternate causes of elbow pain. Patients were excluded if radiographs were positive for arthritis or other pathology. A minimum 6-week follow-up was required. A total of 70 patients (74 elbows) met the criteria; however, 25 patients were lost to follow-up and 3 did not complete outcome measurement forms. Thus 42 patients (44 elbows) were randomized into 1 of 2 treatment groups. Group I received the Hely & Weber (Santa Paula, CA) Velcro wrist extension splint (Figure 1). This group consisted of 24 patients (24 elbows), of which 15 were female and 9 were male, with an average age of 51.8 years 7.9. The majority of patients were right-hand dominant (83%), and the dominant elbow was involved 79% of the time. Group II received the Hely & Weber forearm counterforce strap brace (Figure 2). This group consisted of 18 patients (20 elbows), of which 7 were female and 11 were male, with an average age of 53.1 years 11. The majority of patients were right-hand dominant (89%), and the dominant elbow was involved 55% of the time. Upon assignment of the brace, patients were sent to a single certified orthotist for brace application. Patients were instructed to wear the brace during all daytime hours for a period of 6 weeks. In addition to bracing, patients were given standardized instructions in icing and home stretching exercises. Brace removal was allowed Figure 2 Hely and Weber forearm strap brace. only for bathing, sleeping, and during performance of stretching exercises. Analgesics and anti-inflammatory medications were not formally prescribed for the patients during the study period; however, patients were allowed to take occasional over the counter nonsteroidal anti-inflammatory drugs (NSAIDs) as needed. In addition to a history and physical examination, clinical outcomes were measured using the American Shoulder and Elbow Society (ASES) Elbow Assessment Form10 and the Mayo Elbow Performance (MEP).14 Clinical outcomes were measured at the time of enrollment, as well as at the 6-week follow-up. A 3-week interval visit was also scheduled to track patient progress and check for compliance with the treatment protocol. The score derived from the ASES Elbow Assessment form (henceforward called the ASES derived score) was calculated using a formula based on the variables that did not produce a ceiling effect.13 These variables included pain at its worst, ability to carry a heavy object, and ability to perform heavy household chores. The derived score formula was conceptually similar to that of the ASES Shoulder Score Index.16 The maximum total score is 100 points, with half the points derived from pain and half the points from function. The pain scale is a 10-point analogue pain scale. Each functional variable outcome consists of 4 choices in an ordinal scale. 510 The MEP score was calculated as per prior publication.14 The maximum total score is 100 points. Pain is weighted as 45% of the score, ROM as 20%, stability as 10%, and ADL as 25%. The pain variable outcome consists of a 4-choice ordinal scale, ROM and stability are each a 3-choice ordinal scale, and the 5 functional activities are a dichotomous (can do/cannot do) scale. A change score for each variable and each total score was calculated by subtracting the pre-treatment scores from the 6week follow-up scores. A post-hoc power analysis was performed to determine if sufficient sample size was obtained to achieve 80% power to detect a 20% difference in mean. The data were treated as parametric for the analog pain scale within the ASES Elbow Assessment and as non-parametric for any variable with 4 or less ordinal outcome choices. Likewise, the derived ASES Score and the MEP Score were treated as nonparametric, as at least half the score consisted of nonparametric components. Independent t tests compared the change scores of each outcome variable and the derived scores for the 2 splint conditions (P < .05). R. Garg et al. Figure 3 American Shoulder and Elbow Society score before and 6 weeks after treatment. Results Power, in each group, was minimally 80%. In Group I, the mean ASES score prior to treatment was 35.2 16.9, and at 6 weeks post-treatment was 51.1 19.0 (Figure 3). In Group II, the mean ASES score prior to treatment was 40.7 25.2, and at 6 weeks post-treatment was 54.3 16.6. Although both groups improved, the difference between the 2 groups was not significant (P ¼ .60). In evaluating the individual components of the ASES score, patients in Group I reduced their pain at worst score from 7.5 1.8 to 5.8 2.0 at 6 weeks, while patients in Group II reduced this score from 6.7 2.7 to 6.4 2.6 (Figure 4). This difference was significant (P ¼ .027), demonstrating the wrist extension splint group had better pain relief. The score for carrying heavy objects in Group I increased from 1.4 0.7 to 1.7 0.7 at 6 weeks, while for Group II the score increased from 1.3 0.9 to 2.1 0.6 (Figure 5). This difference was not significant (P ¼ .06). The score for ability to perform heavy chores increased from 1.4 0.8 to 1.9 0.8 in Group I at 6 weeks and increased from 1.6 0.8 to 2.3 0.6 in Group II (Figure 6). This difference was not significant (P ¼ .59). Both groups improved their MEP Scores, with Group I increasing from 70.8 7.9 to 83.5 9.8 at 6 weeks and Group II increasing from 69.8 10.9 to 81.3 9.6 (Figure 7). The difference between the 2 groups’ improvement was not significant (P ¼ .63). All patients in both groups had full range of motion and stability before and after treatment. Discussion There are several reasons why the extension splint group had significantly better pain relief. One possible theory explaining this finding is that the wrist splint allows Figure 4 Pain at worst score before and 6 weeks after treatment as part of the ASES score with low numbers ¼ less pain. improved immobilization of the wrist extensors in the resting position. Jansen et al9 investigated the amount of electrical activity in the wrist extensors by electromyography during activity with and without the wrist splint. The authors discovered a significant decrease in electrical activity using the splint during lifting activities compared to no splint and, therefore, assumed there was decreased tension on the tendon. Additionally, the wrist extension splint is generally visible and serves as a constant reminder to avoid using that arm, possibly allowing better pain relief than the forearm strap. Furthermore, the wrist splint prevents passive stretching of the extensor tendons, thus contributing to pain relief, while the forearm strap does not. Counterforce strap bracing was introduced by Ilfeld in 1965, but Nirschl coined the term ‘‘counterforce’’ in reference to a nonelastic strap to prevent full muscular expansion of the proximal forearm.8,15 The therapeutic effect of this brace lies in the compressive force applied just distal to the origin of the ECRB, which acts to reduce force transmission across the inflamed portion of the muscle tendon unit. Meyer et al12 performed a combined cadaveric and clinical study showing a 13-15% force reduction of the ECRB origin. Snyder-Mackler and Epler18 demonstrated a statistically significant decrease in ECRB and EDC Lateral epicondylitis: brace vs splint Figure 5 Ability to carry heavy objects score before and 6 weeks after treatment as part of the ASES score. Figure 6 Ability to perform heavy chores score before and 6 weeks after treatment as part of the ASES score. muscle force recruitment with the counterforce strap, when compared to no strap, as measured by electromyography. By inhibiting muscle expansion, the strap decreases the magnitude of muscle contraction and, therefore, reduces tension at the musculotendinous junction proximal to the band. Furthermore, the direct compression provided by the strap creates a secondary origin of the extensor tendons; therefore, unloading the true origin at the lateral epicondyle. Although better pain relief was discovered in the wrist splint group, there was no functional difference between the 2 groups. This explains why the total ASES and MEP scores were not significantly different. The high functioning level diluted the pain to an almost undetectable difference. Altan and Kanat1 performed a similar randomized prospective study and concluded there was no significant difference between the 2 brace groups at 6 weeks. The extension splint did not provide improved pain relief over the strap. However, the authors used different outcome measurements than this study. For example, pain was measured during rest and movement rather than specifying pain at worst. In addition, ability to perform daily activities was not evaluated. Their patient population differed from this study as well, possibly explaining the difference in 511 Figure 7 Mayo Elbow Performance score before and 6 weeks after treatment. results. In another similar study, Van de Streek et al21 also concluded there was no difference between the 2 groups at 6 weeks. Their primary outcome measurement was grip strength and pain with grip, as opposed to activities of daily living and pain at worst, therefore explaining the difference in results from this study. Although braces are commonly prescribed for lateral epicondylitis, there is some question regarding their effectiveness. Wuori et al22 compared a counterforce strap with a simple elbow support sleeve, placebo brace, and no brace, and found no significant difference in both grip strength and pain between the groups. However, pain was measured during gripping activities and not subjectively by questionnaire; thus average pain scores were between 1 and 3 on a visual analog scale, while, in this study, pain scores were much higher. Derebery et al7 performed a retrospective study on injured workers with epicondylitis to compare patients who received extension splints to those who did not. Significant findings included patients with splints had higher rates of limited duty, more medical visits and charges, higher total charges, and longer treatment durations than patients without splints. However, the authors included medial epicondylitis in the study group and did not control for concurrent treatments, such as medication or therapy due to the retrospective study design. Additionally, there were several baseline differences between the groups that received the brace from the group that did not. Patients with higher pain severity ratings were more likely to receive the brace. Several studies have compared bracing to other treatment modalities, and there is a lack of evidence for the long-term benefit of physical interventions in general.3 In a randomized controlled trial, Struijs et al19 evaluated the clinical outcome and cost-effectiveness of 180 patients receiving either therapy, elbow strap bracing, or a combination of both for the treatment of lateral epicondylitis at a minimum 1-year follow-up. No clinically relevant or statistically significant differences were found between the groups in regard to pain and function. Success rate at 12 months was 89% in the physical therapy group, 86% in the brace group, and 87% in 512 the combination group. The same authors performed a metaanalysis that included all randomized clinical trials describing individuals with diagnosed lateral epicondylitis and comparing the use of an orthotic device as a treatment strategy.20 Only 5 studies met their inclusion criteria; therefore, there were few outcome measures, large heterogeneity, and limited long-term results. They stated no definitive conclusions could be drawn concerning the effectiveness of orthotic devices and that more well-designed randomized clinical trials of sufficient power are warranted. Labelle et al11 performed a systematic review to assess the scientific evidence for methods of treatment for lateral epicondylitis. The authors concluded that there was insufficient evidence to support any of the current conservative treatment options, secondary to lack of scientific validity. Several limitations to this study existed, including the lack of a control group whom received no treatment. Smidt et al17 showed patients who did not receive any treatment had similar success rates at 1 year compared to other treatment modalities, although they did significantly worse in the short term. The study reported herein did not focus on whether the brace groups improved individually versus no treatment, but rather compared the differences in clinical outcome between the 2 types of braces. Another limitation of this study is that occasional NSAID use was allowed if pain was intolerable. This potentially adds a confounding variable, although it was assumed each group had equal amounts of NSAID usage. The last limitation is the lack of long-term follow-up. The follow-up interval was purposefully chosen to determine the acute clinical outcome differences between the 2 brace groups at 6 weeks rather than long-term differences. Conclusion There was no difference in total clinical outcome scores between the forearm counterforce strap and the extension wrist splint groups for the treatment of lateral epicondylitis of the elbow at 6 weeks. However, the extension splint group had significantly better pain relief and thus is recommended over the forearm strap brace. Disclaimer The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article. R. Garg et al. References 1. Altan L, Kanat E. Conservative treatment of lateral epicondylitis: comparison of two different orthotic devices. Clin Rheum 2008;27: 1015-9. 2. Assendelft WJ, Hay EM, Adshead R, Bouter LM. Corticosteroid injections for lateral epicondylitis: a systematic overview. Br J Gen Pract 1996;46:209-16. 3. Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med 2005;39:411-22. 4. Boyer MI, Hasting H II. Lateral tennis elbow: ‘‘Is there any science out there?’’ J Shoulder Elbow Surg 1999;8:481-91. 5. Coonrad RW. Tennis elbow. Instr Course Lect 1986;35:94-101. 6. Coonrad RW, Hooper WR. Tennis elbow: its course, natural history, conservative and surgical management. J Bone Joint Surg Am 1973; 55:1177-82. 7. Derebery VJ, Devenport JN, Giang GM, Fogarty WT. The effects of splinting on outcomes for epicondylitis. Arch Phys Med Rehab 2005; 86:1081-8. 8. Ilfeld FW, Field SM. Treatment of tennis elbow. Use of a special brace. J Am Med Assoc 1966;195:67-70. 9. Jansen CW, Olson SL, Hasson SM. The effect of use of a wrist orthosis during functional activities on surface electromyography of the wrist extensors in normal subjects. J Hand Ther 1997;10:283-9. 10. King GJW, Richards RR, Zuckerman JD, Blasier R, Dillman C, Friedman RJ, et al. A standardized method for assessment of elbow function. J Shoulder Elbow Surg 1999;8:351-4. 11. Labelle H, Guibert R, Joncas J, Newman N, Fallaha M, Rivard CH. Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow. An attempted meta-analysis. J Bone Joint Surg Br 1992;74:646-51. 12. Meyer NJ, Walter F, Haines B, Orton D, Daley RA. Modeled evidence of force reduction at the extensor carpi radialis brevis origin with the forearm support band. J Hand Surg [Am] 2003;28:279-87. 13. Michlitsch M, Adamson GJ, Pink MM, Koganti A. Outcome assessment in patients with lateral epicondylitis. J Shoulder Elbow Surg. Submitted for Publication. 14. Morrey BF, An KN. Functional evaluation of the elbow. In: The elbow and its disorders. 3rd ed. Philadelphia: Saunders; 2000. p. 74-83. 15. Nirschl RP. Tennis elbow. Orthop Clin North Am 1973;4:787-800. 16. Richards RR, An KN, Bigliani LU, Freidman RJ, Gartsman GM, Gristina AG, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg 1994;3:347-52. 17. Smidt N, Van Der Windt DA, Assendelft WJ. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomized controlled trial. Lancet 2002;359:657-62. 18. Snyder-Mackler L, Epler M. Effect of standard and Aircast tennis elbow bands on integrated electromyography of forearm extensor musculature proximal to the bands. Am J Sports Med 1989;17:278-81. 19. Struijs PAA, Korthals-de Bos IBC, Van Tulder MW, Van Dijk CN, Bouter LM, Assendelft WJJ. Cost-effectiveness of brace, physical therapy or both, for treatment of tennis elbow. Br J Sports Med 2006;40:637-43. 20. Struijs PA, Smidt N, Arola H, Dijk CN, Buchbinder R, Assendelft WJ. Orthotic devices for the treatment of tennis elbow. Cochrane Database Syst Rev 2002. CD001821. 21. Van De Streek MD, Van Der Schans CP, De Greef MH, Postema K. The effect of a forearm/hand splint compared with an elbow band as a treatment for lateral epicondylitis. Prosthet Orthot Int 2004;28:183-9. 22. Wuori JL, Overend TJ, Kramer JF, MacDermid J. Strength and pain measures associated with lateral epicondylitis bracing. Arch Phys Med Rehabil 1998;79:832-7.