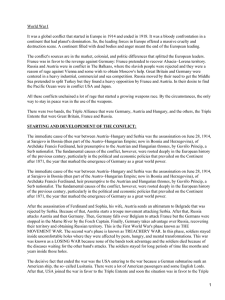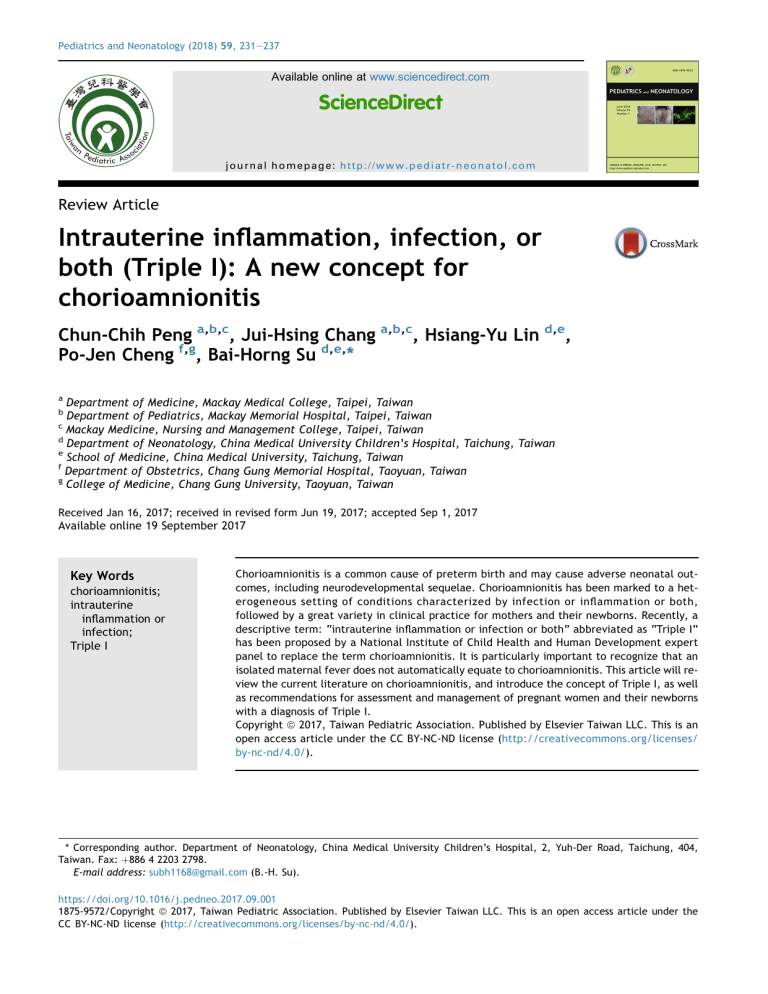
Pediatrics and Neonatology (2018) 59, 231e237 Available online at www.sciencedirect.com ScienceDirect journal homepage: http://www.pediatr-neonatol.com Review Article Intrauterine inflammation, infection, or both (Triple I): A new concept for chorioamnionitis Chun-Chih Peng a,b,c, Jui-Hsing Chang a,b,c, Hsiang-Yu Lin d,e, Po-Jen Cheng f,g, Bai-Horng Su d,e,* a Department of Medicine, Mackay Medical College, Taipei, Taiwan Department of Pediatrics, Mackay Memorial Hospital, Taipei, Taiwan c Mackay Medicine, Nursing and Management College, Taipei, Taiwan d Department of Neonatology, China Medical University Children’s Hospital, Taichung, Taiwan e School of Medicine, China Medical University, Taichung, Taiwan f Department of Obstetrics, Chang Gung Memorial Hospital, Taoyuan, Taiwan g College of Medicine, Chang Gung University, Taoyuan, Taiwan b Received Jan 16, 2017; received in revised form Jun 19, 2017; accepted Sep 1, 2017 Available online 19 September 2017 Key Words chorioamnionitis; intrauterine inflammation or infection; Triple I Chorioamnionitis is a common cause of preterm birth and may cause adverse neonatal outcomes, including neurodevelopmental sequelae. Chorioamnionitis has been marked to a heterogeneous setting of conditions characterized by infection or inflammation or both, followed by a great variety in clinical practice for mothers and their newborns. Recently, a descriptive term: “intrauterine inflammation or infection or both” abbreviated as “Triple I” has been proposed by a National Institute of Child Health and Human Development expert panel to replace the term chorioamnionitis. It is particularly important to recognize that an isolated maternal fever does not automatically equate to chorioamnionitis. This article will review the current literature on chorioamnionitis, and introduce the concept of Triple I, as well as recommendations for assessment and management of pregnant women and their newborns with a diagnosis of Triple I. Copyright ª 2017, Taiwan Pediatric Association. Published by Elsevier Taiwan LLC. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/ by-nc-nd/4.0/). * Corresponding author. Department of Neonatology, China Medical University Children’s Hospital, 2, Yuh-Der Road, Taichung, 404, Taiwan. Fax: þ886 4 2203 2798. E-mail address: subh1168@gmail.com (B.-H. Su). https://doi.org/10.1016/j.pedneo.2017.09.001 1875-9572/Copyright ª 2017, Taiwan Pediatric Association. Published by Elsevier Taiwan LLC. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/). 232 1. Introduction Chorioamnionitis is a common cause of preterm birth and may causes adverse neonatal outcomes, including neurodevelopmental sequelae.1e3 Clinically, chorioamnionitis has been marked to a heterogeneous setting of conditions characterized by infection or inflammation or both, followed by a great variety in clinical practice for mothers and their newborns. Recently, the term “intrauterine inflammation or infection or both” abbreviated as “Triple I” has been suggested by a National Institute of Child Health and Human Development (NICHD) expert panel including maternal and neonatal experts in a workshop to replace the term chorioamnionitis.4 This article will review the current literature on chorioamnionitis, and introduce the concept of Triple I, as well as recommendations for assessment and management of pregnant women and their newborns with a diagnosis of Triple I. 2. Current understanding of chorioamnionitis Preterm birth is a major cause of perinatal mortality and long-term morbidity. Chorioamnionitis is a common cause of preterm birth. A recent prospective study of 871 pregnancies found that those with histologic chorioamnionitis, premature delivery occurred nearly twice as often as those without chorioamnionitis.3 Chorioamnionitis may induce preterm delivery by a maternal inflammatory response.1,2 Bacterial infection, via the release of endotoxins and exotoxins, stimulates the release of cytokines from the decidua and fetal membranes, which induce uterine contractions and/or rupture of fetal membranes. According to the presence or absence of clinical signs and laboratory evidence, chorioamnionitis may be categorized as clinical chorioamnionitis and subclinical/histologic chorioamnionitis.1,2,5e7 Clinical chorioamnionitis is characterized by maternal fever, leukocytosis, maternal and/or fetal tachycardia, uterine tenderness, and preterm rupture of membranes (PROM). Subclinical/histologic chorioamnionitis is asymptomatic and defined by inflammation of the chorion, amnion, and placenta, which is more common than clinical chorioamnionitis.1,2 The inflammation of the chorioamnion (histologic chorioamnionitis) and umbilical cord (funisitis) are the manifestations of the maternal and fetal immune responses in condition of intra-amniotic infection.6,7 Histological and microbiological evidence of inflammation or infection may not always accompany one another. And maternal clinical signs may not be present. The frequency of histologic chorioamnionitis is higher than that of clinical chorioamnionitis with positive bacterial cultures. The treatment with antibiotics and the difficulty of growing fastidious organisms may lead to negative cultures even in the presence of histological evidence of placental inflammation.6 Therefore, pathological evaluation of the placenta is essential for definite diagnosis. Different authors have shown higher positive cultures rates of amniotic fluid in women with preterm labor at earlier gestational ages,8 higher interleukin (IL)-6 levels in the amniotic fluid in women with spontaneous labor in pregnancies less than 34 weeks,9 and higher IL-6 levels in cord blood in preterm compared with term newborns born C.-C. Peng et al after microbial invasion of the amniotic cavity.10 The fetal inflammatory response syndrome (FIRS) is a condition characterized by systemic activation of the fetal immune system. FIRS was originally defined as an elevation of the fetal plasma IL-6 concentration in fetuses of mothers with preterm labor and PROM.11 PROM refers to rupture of membranes (ROM) prior to the onset of labor but beyond 37 weeks’ gestation. ROM prior to 37 weeks’ gestation is called preterm PROM (PPROM). PPROM is responsible for one-third of preterm deliveries.12 Prolonged ROM is any ROM that persists for more than 24 h and prior to the onset of labor; it increases incidence of neonatal sepsis 2e10 times because of the facilitated ascending infection to the uterine cavity, and this risk becomes 4 times higher when ROM is accompanied by chorioamnionitis.13 The incidence of histological chorioamnionitis increases up to 50% with PPROM6,7 and is inversely related to gestational age.14e16 Histological chorioamnionitis is most commonly associated with intrauterine bacterial infection, and may coexist with umbilical infiltration (funisitis).17 It is believed that FIRS, as a result of infection pathways and increasing cytokines activate an inflammatory response that potentially lead to fetal vasculitis, congenital anomalies, fetal death, fetal hydrops, spontaneous abortion, preterm labor, or preterm rupture of the membranes.18,19 Chorioamnionitis has been suggested to affect neonatal outcome adversely by increasing the risk of bronchopulmonary dysplasia, necrotizing enterocolitis, intraventricular hemorrhage, patent ductus arteriosus, neonatal sepsis, and neurodevelopmental sequelae.16,20e23 3. Current management of chorioamnionitis Chorioamnionitis is an acute condition requiring a high index of suspicion, and the threshold for antibiotics treatment is low in the pregnant woman and their neonates because both are severely affected by the organisms leading to infection.24 Clinical chorioamnionitis is diagnosed when following clinical signs are present: maternal fever, maternal and/or fetal tachycardia, maternal leukocytosis, uterine tenderness, and foul-smelling or purulent amniotic fluid.25 However, these subjective findings are generally neither sensitive nor specific. Maternal fever complicates up to one-third of labors and has diverse causes including infection, epidural anesthesia, and inflammation. Because not every maternal fever is caused by infection, to treat all fevers with antibiotics will result in overtreatment of mothers.24e26 Many intrauterine or extrauterine factors may cause maternal fever. Intrauterine infection can result in preterm birth, increased risk of operative delivery, maternal bacteremia and sepsis, postcesarean wound infection, need for hysterectomy, postpartum hemorrhage, admission to intensive care unit, and rarely maternal mortality.25 However, a clear differentiation between infectious and noninfectious fever during labor is difficult; therefore, intrapartum fever frequently results in evaluation and treatment of neonates for possible sepsis.27,28 The clinical signs and laboratory data usually used to diagnose chorioamnionitis have poor predictive value, may be Triple I: A new concept for chorioamnionitis absent or appear late, and are unreliable for identification of acute chorioamnionitis. In addition, the term “rule out chorioamnionitis” and maternal antibiotic treatment itself often results in evaluation and antibiotic treatment of neonates for possible sepsis for varying duration.29e31 3.1. Guidelines for neonates born to women with suspected chorioamnionitis The effects of intrauterine infection on the fetus and the newborn depend on the duration and timing of the inflammatory process. Acute infection is a risk factor for early-onset neonatal sepsis. However, chronic infection usually is subclinical and has been associated with a wide variety of neonatal organ injury, including brain, lung, eye, intestine, and thymus.26 Once maternal chorioamnionitis is diagnosed, in spite of the duration of intrapartum antibiotics, the current recommendation from the Centers for Disease Control and Prevention (CDC),32 and the Committee on Fetus and Newborn of the American Academy of Pediatrics (AAP)33 required a full sepsis workup and initiation of antibiotics treatment even in well-appearing infants. The actual intrauterine transmission of microorganisms to the fetus is very low and limited to high virulent bacteria such as gramnegative bacilli, aerobic streptococci, and Listeria.34 These guidelines significantly increase the neonatal exposure to antibiotics in an attempt to treat rare possibility of earlyonset sepsis. It is worth to emphasize that maternal fever or suspected chorioamnionitis without evidence of fetal infection is unlikely to cause fetal or neonatal injury.35 Therefore, it is important to reevaluate the policy for this group of women and newborns.4 4. Intrauterine inflammation, infection, or both (Triple I) On January 26e27, 2015, the Eunice Kennedy Shriver NICHD, the Society for Maternal-Fetal Medicine, the American College of Obstetricians and Gynecologists, and the American Academy of Pediatrics invited a group of maternal and neonatal experts to a workshop to address numerous knowledge gaps and to provide evidence-based guidelines for the diagnosis and management of pregnant women with chorioamnionitis and their neonates. The expert panel agreed that isolated maternal fever should not lead to a diagnosis of infection (or chorioamnionitis) and to antibiotics therapy.4 The expert panel recommended to use the term “intrauterine inflammation or infection or both” or “Triple I” as shown in Table 1 to replace the term chorioamnionitis. 4.1. Diagnosis of Triple I According to the recommendation, Triple I is diagnosed when maternal fever is present with one or more of the following4: 1. Fetal tachycardia (>160 beats/min for 10 min or longer)36 233 Table 1 Features of isolated maternal fever and Triple I with classification. Terminology Features and comments Isolated maternal fever (“documented” fever) Maternal oral temperature 39.0 C or greater (102.2 F) on any one occasion is documented fever. If the oral temperature is between 38.0 C (100.4 F) and 39.0 C (102.0 F), repeat the measurement in 30 min; if the repeat value remains at least 38.0 C (100.4 F), it is documented fever Fever without a clear source plus any of the following: 1) baseline fetal tachycardia (greater that 160 beats per min for 10 min or longer, excluding accelerations, decelerations, and periods of marked variability) 2) maternal white blood cell count greater than 15,000 per mm3 in the absence of corticosteroids 3) definite purulent fluid from the cervical os All the above plus: 1) amniocentesis-proven infection through a positive Gram stain 2) low glucose or positive amniotic fluid culture 3) placental pathology revealing diagnostic features of infection Suspected Triple I Confirmed Triple I *Discontinue the use of the term “Chorioamnionitis.” See the text for discussion. Copyright 2016, The American College of Obstetricians and Gynecologists and Wolters Kluwer Health, Inc. Reproduced from Higgins RD et al.4 with permission. 2. Maternal WBC count >15,000 cells/mm3 without using corticosteroids 3. Purulent discharge from the cervical os confirmed visually on speculum examination 4. Biochemical or microbiologic evidence in amniotic fluid consistent with amniotic infection (see subsequently). 4.2. Clinical category of Triple I (Table 1) 1. Isolated maternal fever (not Triple I) 2. Suspected Triple I 3. Confirmed Triple I. 4.2.1. Isolated maternal fever Fever without any criteria (listed in Section 4.1.) should be defined as “isolated maternal fever.” The criteria of maternal fever were defined as follows: maternal temperature 39.0 C or 102.2 F on one reading. If the temperature is 38.0 C or 100.4 F but <39.0 C or 234 102.2 F, the temperature should be rechecked in 30 min. A repeat temperature 38.0 C or 100.4 F constitutes a documented fever.25,37 Oral temperature measurement was recommended.38 In labor accompanied with fever and unknown GBS status at gestation 37 weeks, intrapartum prophylaxis should be given according to CDC guidelines.32 4.2.2. Suspected Triple I Without confirmation, Triple I should be qualified with the term “suspected.” 4.2.3. Confirmed Triple I To diagnose a confirmed Triple I, infection in amniotic fluid (AF) or histopathologic evidence of infection or inflammation or both in the placenta, fetal membranes, or the umbilical cord vessels (funisitis) should be proved by laboratory findings. These findings include positive Gram stain for bacteria in AF, low AF glucose, high WBC count in the absence of a bloody tap, or positive AF culture results.34,40,41 4.3. Biomarkers Objective biomarkers that can precisely assess the risk for early-onset neonatal sepsis is very important. Potential biomarkers to guide neonatal management can either be antenatal or postnatal. 4.3.1. Antenatal markers Antenatal markers accompanied with gestational age and clinical manifestations can be used to guide the management for mother.4 Antenatal markers confirmation of chorioamnionitis is not routinely necessary in women at term who are progressing to delivery. However, in women with preterm labor being evaluated for tocolysis or using corticosteroid, biomarks assessment may be of value in establishing the diagnosis of chorioamnionitis. The different biomarkers that have been evaluated are far from ideal, either because the accuracy is not sufficient to define a specific threshold or because of the invasiveness of an amniocentesis. Investigational studies have noted IL-6 has promise as a marker of intrauterine inflammation.34,39 However, current data remain controversial. A recent Cochrane review revealed that using AF analysis to exclude Triple I in women with PPROM has low quality of evidence.42 In contrast, some recent studies recommend to rule out Triple I using AF analysis before doing cervical cerclage.43e45 4.3.2. Postnatal markers Postnatal markers should have the role to guide the postnatal care of the newborn in 1) to objectively confirm the presence of neonatal sepsis, 2) to help to decide whether admission to NICU and antibiotics therapy is necessary or not, and to guide the duration of antibiotics therapy, and 3) to facilitate maternal and family counseling about the probable cause of preterm birth and future pregnancies.4 Umbilical cord blood and neonatal blood taken within 72 h of birth are the most often used for biomarkers examination for early-onset sepsis. The cord blood has advantage because it can obtain a relatively large amount C.-C. Peng et al immediately on delivery. The disadvantage is that some biomarkers of placental origin may be higher than neonatal blood. CRP, procalcitonin, IL-6, IL-8, haptoglobin and haptoglobin-related protein in cord blood have been widely studied and used in association with hematologic indices to predict early-onset neonatal sepsis.46e50 The amount of blood that can be safely obtained for biomarkers examination is limited, especially in very low birth weight infants. Some biomarkers such as CRP and IL-6 are affected by postnatal physiologic changes that reduce their specificity.51,52 Blood cultures are known as the gold standard for early-onset sepsis, however, their use is limited by false negative or false-positive results.53 In additions, currently there is no established consensus definition for neonatal sepsis. New biomarkers should be developed and evaluated on the basis of neonatal outcomes. 4.4. Maternal management The management for mother includes 1) to consider admission or transfer to facilities with maternalefetal care and grade 3 or 4 NICU if indicated by clinical evaluation, 2) to decide whether to take expectant management or to expeditious delivery, 3) to decide whether to perform a cervical cerclage or not, 4) to decide whether to initiate tocolytic treatment or not, 5) to decide whether antibiotics treatment should be given or not, and 6) when to give steroid.4,32,54 4.5. Neonatal management Neonatal management should be guided by the clinical category of isolated fever, suspected Triple I or confirmed Triple I, gestational age at birth, and neonatal conditions (Fig. 1, Algorithm).4 Communication between obstetric and neonatal teams is essential for the appropriate neonatal treatment. Clinical management is different for term and late preterm neonates as compared with preterm neonates with gestational age <34 weeks. 4.5.1. Term and late preterm neonates4 1. When isolated maternal fever, treatment is not beneficial for well-appearing term and late preterm neonates according to current evidence 2. When suspected Triple I, care should be decided by clinical conditions. The majority of well-appearing term and late preterm neonates can be observed without receiving antibiotics treatment if remain asymptomatic 3. When confirmed Triple I, these neonates should be treated according to current guidelines32,33 All neonates born to women with suspected or confirmed Triple I who are not treated require close observations. 4.5.2. Neonates born at <34 0/7 weeks of gestation4 1. When isolated maternal fever, well-appearing preterm neonates with gestational age <34 weeks might be Triple I: A new concept for chorioamnionitis 235 Figure 1 Proposed algorism for neonatal management. Copyright 2016, The American College of Obstetricians and Gynecologists and Wolters Kluwer Health, Inc. Reproduced from Higgins RD et al.4 with permission. observed if laboratory data is not favor of sepsis, but this recommendation is not evidence-based 2. When suspected or confirmed Triple I, neonates with gestational age <34 weeks should be given antibiotics treatment as soon as cultures are done 3. The more the prematurity is, the more likely the preterm neonates will be symptomatic and should not be treating as “well-appearing”. 4.6. Duration of neonatal antimicrobial therapy In most well-appearing neonates, there is no evidence that antibiotics treatment should be continued more than 48 h when blood cultures are negative. However, there are concerns about the validity of blood cultures in neonates when their mother received broad-spectrum antibiotics before delivery. It is a common reason for newborns being treated with antibiotics for more than 5 days. To develop more rigorous diagnostic criteria may better identify those women and their neonates most likely to benefit from antibiotics treatment and reduce unnecessary antibiotic exposure.35 4.7. Communication between neonatal team and obstetric team Close communication between neonatal team and obstetric team can ensure appropriate maternal and neonatal management. Box 1 provides items that could be included on a checklist for every shift change to ensure continuity of care.4 The education of obstetric and pediatric or neonatal staff is important for the communication, identification, and appropriate treatment of women at risk for Triple I and their newborns. Box 1. Checklist of items to include in communication between the obstetric and neonatal teams. Gestational age Maternal tachycardia Fetal tachycardia Maternal white blood cell count greater than 15,000 Maternal group B streptococci status Duration of rupture of membranes Duration of labor Purulent fluid Amniotic fluid evaluation Highest maternal temperature Epidural anesthesia use Prostaglandin use Antimicrobial agent(s) used Antipyretic used Spontaneous preterm birth Prior spontaneous preterm birth Copyright 2016, The American College of Obstetricians and Gynecologists and Wolters Kluwer Health, Inc. Reproduced from Higgins RD et al.4 with permission. 5. Conclusion In clinical practice, the term chorioamnionitis has been used excessively and implies the presence of infectious and inflammatory conditions affecting the mother, fetus and newborn. In order to achieve better fetal, maternal and neonatal care, the NICHD expert panel has recommended the new concept “Triple I” to indicate intrauterine 236 inflammation or infection or both while restricting the term chorioamnionitis to a pathologic diagnosis. Chorioamnionitis is usually diagnosed based on subjective findings or by histopathologic examination of the placenta and the umbilical cord. To develop more rigorous diagnostic criteria may better identify those women and their neonates most likely to benefit from antibiotics treatment and reduce unnecessary antibiotic exposure. A prospective study to determine whether clinical parameters combined with biomarkers accurately predict the presence of Triple I would be beneficial to improve maternal and neonatal health care. Conflict of interest None. References 1. Su BH. Histologic chorioamnionitis and neonatal outcome in preterm infants. Pediatr Neonatol 2014;55:154e5. 2. Galinsky R, Polglase GR, Hooper SB, Black MJ, Moss TJ. The consequences of chorioamnionitis: preterm birth and effects on development. J Pregnancy 2013;2013:412831. 3. Bastek JA, Weber AL, McShea MA, Ryan ME, Elovitz MA. Prenatal inflammation is associated with adverse neonatal outcomes. Am J Obstet Gynecol 2014;210. 450.e1e10. 4. Higgins RD, Saade G, Polin RA, Grobman WA, Buhimschi IA, Watterberg K, et al. Evaluation and management of women and newborns with a maternal diagnosis of chorioamnionitis: summary of a workshop. Obstet Gynecol 2016;127:426e36. 5. Erdemir G, Kultursay N, Calkavur S, Zekioglu O, Koroglu OA, Cakmak B, et al. Histological chorioamnionitis: effects on premature delivery and neonatal prognosis. Pediatr Neonatol 2013;54:267e74. 6. Smulian JC, Shen-Schwarz S, Vintzileos AM, Lake MF, Ananth CV. Clinical chorioamnionitis and histologic placental inflammation. Obstet Gynecol 1999;94:1000e5. 7. Steel JH, O’donoghue K, Kennea NL, Sullivan MH, Edwards AD. Maternal origin of inflammatory leukocytes in preterm fetal membranes, shown by fluorescence in situ hybridisation. Placenta 2005;26:672e7. 8. Watts DH, Krohn MA, Hillier SL, Eschenbach DA. The association of occult amniotic fluid infection with gestational age and neonatal outcome among women in preterm labor. Obstet Gynecol 1992;79:351e7. 9. Andrews WW, Hauth JC, Goldenberg RL, Gomez R, Romero R, Cassell GH. Amniotic fluid interleukin-6: correlation with upper genital tract microbial colonization and gestational age in women delivered after spontaneous labor versus indicated delivery. Am J Obstet Gynecol 1995;173:606e12. 10. Yoon BH, Romero R, Moon J, Chaiworapongsa T, Espinoza J, Kim YM, et al. Differences in the fetal interleukin-6 response to microbial invasion of the amniotic cavity between term and preterm gestation. J Matern Fetal Neonatal Med 2003;13: 32e8. 11. Gomez R, Romero R, Ghezzi F, Yoon BH, Mazor M, Berry SM. The fetal inflammatory response syndrome. Am J Obstet Gynecol 1998;179:194e202. 12. Parry S, Strauss 3rd JF. Premature rupture of the fetal membranes. N Engl J Med 1998;338:663e70. 13. Edwards MS. Postnatal bacterial infections. In: Martin RJ, Fanaroff AA, Walsh MC, editors. Fanaroff and Martin’s neonatal perinatal medicine disease of the fetus and ınfant. 8th ed., vol. 2. Philadelphia: Mosby Elsevier; 2006. p. 791e804. C.-C. Peng et al 14. Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD neonatal research network. Pediatrics 2010;126:443e56. 15. Lahra MM, Jeffery HE. A fetal response to chorioamnionitis is associated with early survival after preterm birth. Am J Obstet Gynecol 2004;190:147e51. 16. Dammann O, Allred EN, Leviton A, Shen-Schwarz S, Heller D, Genest DR, et al. Fetal vasculitis in preterm newborns: interrelationships, modifiers, and antecedents. Placenta 2004; 25:788e96. 17. Redline RW. Inflammatory responses in the placenta and umbilical cord. Semin Fetal Neonatal Med 2006;11:296e301. 18. Pacora P, Chaiworapongsa T, Maymon E, Kim YM, Gomez R, Yoon BH, et al. Funisitis and chorionic vasculitis: the histological counterpart of the fetal inflammatory response syndrome. J Matern Fetal Neonatal Med 2002;11:18e25. 19. Yoon BH, Romero R, Park JS, Kim M, Oh SY, Kim CJ, et al. The relationship among inflammatory lesions of the umbilical cord (funisitis), umbilical cord plasma interleukin 6 concentration, amniotic fluid infection, and neonatal sepsis. Am J Obstet Gynecol 2000;183:1124e9. 20. Ogunyemi D, Murillo M, Jackson U, Hunter N, Alperson B. The relationship between placental histopathology findings and perinatal outcome in preterm infants. J Matern Fetal Neonatal Med 2003;13:102e9. 21. Dexter SC, Malee MP, Pinar H, Hogan JW, Carpenter MW, Vohr BR. Influence of chorioamnionitis on developmental outcome in very low birth weight infants. Obstet Gynecol 1999; 94:267e73. 22. Salas AA, Faye-Petersen OM, Sims B, Peralta-Carcelen M, Reilly SD, McGwin Jr G, et al. Histological characteristics of the fetal inflammatory response associated with neurodevelopmental impairment and death in extremely preterm infants. J Pediatr 2013;163:652e7. 23. Malaeb S, Dammann O. Fetal inflammatory response and brain injury in the preterm newborn. J Child Neurol 2009;24: 1119e26. 24. Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med 2014;370:2211e8. 25. Tita AT, Andrews WW. Diagnosis and management of clinical chorioamnionitis. Clin Perinatol 2010;37:339e54. 26. Lieberman E, Lang J, Richardson DK, Frigoletto FD, Heffner LJ, Cohen A. Intrapartum maternal fever and neonatal outcome. Pediatrics 2000;105:8e13. 27. Evers AC, Nijhuis L, Koster MP, Bont LJ, Visser GH. Intrapartum fever at term: diagnostic markers to individualize the risk of fetal infection: a review. Obstet Gynecol Surv 2012;67: 187e200. 28. Impey LW, Greenwood CE, Black RS, Yeh PS, Sheil O, Doyle P. The relationship between intrapartum maternal fever and neonatal acidosis as risk factors for neonatal encephalopathy. Am J Obstet Gynecol 2008;198:49. 29. Mukhopadhyay S, Dukhovny D, Mao W, Eichenwald EC, Puopolo KM. 2010 perinatal GBS prevention guideline and resource utilization. Pediatrics 2014;133:196e203. 30. Kiser C, Nawab U, McKenna K, Aghai ZH. Role of guidelines on length of therapy in chorioamnionitis and neonatal sepsis. Pediatrics 2014;133:992e8. 31. Mukherjee A, Davidson L, Anguvaa L, Duffy DA, Kennea N. NICE neonatal early onset sepsis guidance: greater consistency, but more investigations, and greater length of stay. Arch Dis Child Fetal Neonatal Ed 2015;100:F248e9. 32. Verani JR, McGee L, Schrag SJ. Division of bacterial diseases, national center for immunization and respiratory diseases, centers for disease control and prevention (CDC). Prevention of perinatal group B streptococcal diseasedrevised guidelines from CDC, 2010. MMWR Recomm Rep 2010;59:1e36. Triple I: A new concept for chorioamnionitis 33. Polin RA, Committee on fetus and newborn. Management of neonates with suspected or proven early-onset bacterial sepsis. Pediatrics 2012;129:1006e15. 34. Redline RW. Inflammatory response in acute chorioamnionitis. Semin Fetal Neonatal Med 2012;17:20e5. 35. Polin RA, Randis TM. Chorioamnionitis. In: Martin RJ, Fanaroff AA, Walsh MC, editors. Fanaroff and Martin’s neonatal-perinatal medicine. 10th ed. Philadelphia, PA: Elsevier; 2015. p. 355e64. 36. Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. J Obstet Gynecol Neonatal Nurs 2008;37:510e5. 37. Avila C, Willins JL, Jackson M, Mathai J, Jabsky M, Kong A, et al. Usefulness of two clinical chorioamnionitis definitions in predicting neonatal infectious outcomes: a systematic review. Am J Perinatol 2015;32:1001e9. 38. Banerjee S, Cashman P, Yentis SM, Steer PJ. Maternal temperature monitoring during labor: concordance and variability among monitoring sites. Obstet Gynecol 2004;103:287e93. 39. Genc MR, Ford CE. The clinical use of inflammatory markers during pregnancy. Curr Opin Obstet Gynecol 2010;22:116e21. 40. Buhimschi CS, Bhandari V, Hamar BD, Bahtiyar MO, Zhao G, Sfakianaki AK, et al. Proteomic profiling of the amniotic fluid to detect inflammation, infection, and neonatal sepsis. PLoS Med 2007;4:e18. 41. Abdel-Razeq SS, Buhimschi IA, Bahtiyar MO, Rosenberg VA, Dulay AT, Han CS, et al. Interpretation of amniotic fluid white blood cell count in “bloody tap” amniocenteses in women with symptoms of preterm labor. Obstet Gynecol 2010;116:344e54. 42. Sharp GC, Stock SJ, Norman JE. Fetal assessment methods for improving neonatal and maternal outcomes in preterm prelabour rupture of membranes. Cochrane Database Syst Rev 2014;(10):CD010209. 43. Aguin E, Aguin T, Cordoba M, Aguin V, Roberts R, Albayrak S, et al. Amniotic fluid inflammation with negative culture and outcome after cervical cerclage. J Matern Fetal Neonatal Med 2012;25:1990e4. 44. Vaisbuch E, Hassan SS, Mazaki-Tovi S, Nhan-Chang CL, Kusanovic JP, Chaiworapongsa T, et al. Patients with an 237 45. 46. 47. 48. 49. 50. 51. 52. 53. 54. asymptomatic short cervix (15 mm) have a high rate of subclinical intraamniotic inflammation: implications for patient counseling. Am J Obstet Gynecol 2010;202:433. Lisonkova S, Sabr Y, Joseph KS. Diagnosis of subclinical amniotic fluid infection prior to rescue cerclage using gram stain and glucose tests: an individual patient meta-analysis. J Obstet Gynaecol Can 2014;36:116e22. Steinberger E, Hofer N, Resch B. Cord blood procalcitonin and Interleukin-6 are highly sensitive and specific in the prediction of early-onset sepsis in preterm infants. Scand J Clin Lab Investig 2014;74:432e6. Cobo T, Kacerovsky M, Andrys C, Drahosova M, Musilova I, Hornychova H, et al. Umbilical cord blood IL-6 as predictor of early-onset neonatal sepsis in women with preterm prelabour rupture of membranes. PLoS One 2013;8:e69341. Howman RA, Charles AK, Jacques A, Doherty DA, Simmer K, Strunk T, et al. Inflammatory and haematological markers in the maternal, umbilical cord and infant circulation in histological chorioamnionitis. PLoS One 2012;7:e51836. Fan Y, Yu JL. Umbilical blood biomarkers for predicting earlyonset neonatal sepsis. World J Pediatr 2012;8:101e8. Buhimschi CS, Bhandari V, Dulay AT, Nayeri UA, AbdelRazeq SS, Pettker CM, et al. Proteomics mapping of cord blood identifies haptoglobin “switch-on” pattern as biomarker of early-onset neonatal sepsis in preterm newborns. PLoS One 2011;6:e26111. Chiesa C, Signore F, Assumma M, Buffone E, Tramontozzi P, Osborn JF, et al. Serial measurements of C-reactive protein and interleukin-6 in the immediate postnatal period: reference intervals and analysis of maternal and perinatal confounders. Clin Chem 2001;47:1016e22. Chiesa C, Pellegrini G, Panero A, Osborn JF, Signore F, Assumma M, et al. C-reactive protein, interleukin-6, and procalcitonin in the immediate postnatal period: influence of illness severity, risk status, antenatal and perinatal complications, and infection. Clin Chem 2003;49:60e8. Wynn JL, Wong HR, Shanley TP, Bizzarro MJ, Saiman L, Polin RA. Time for a neonatal-specific consensus definition for sepsis. Pediatr Crit Care Med 2014;15:523e8. Goldenberg RL, Hauth JC, Andrews WW. Intrauterine infection and preterm delivery. N Engl J Med 2000;342:1500e7.