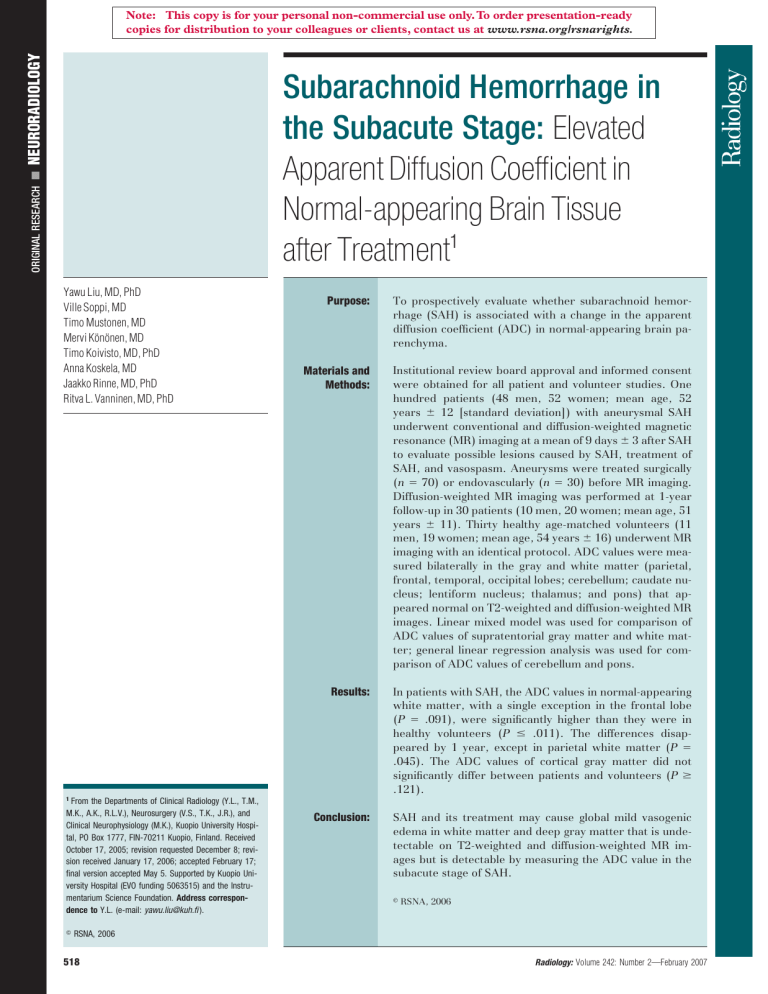
䡲 NEURORADIOLOGY Note: This copy is for your personal non-commercial use only. To order presentation-ready copies for distribution to your colleagues or clients, contact us at www.rsna.org/rsnarights. ORIGINAL RESEARCH Subarachnoid Hemorrhage in the Subacute Stage: Elevated Apparent Diffusion Coefficient in Normal-appearing Brain Tissue after Treatment1 Yawu Liu, MD, PhD Ville Soppi, MD Timo Mustonen, MD Mervi Könönen, MD Timo Koivisto, MD, PhD Anna Koskela, MD Jaakko Rinne, MD, PhD Ritva L. Vanninen, MD, PhD Purpose: To prospectively evaluate whether subarachnoid hemorrhage (SAH) is associated with a change in the apparent diffusion coefficient (ADC) in normal-appearing brain parenchyma. Materials and Methods: Institutional review board approval and informed consent were obtained for all patient and volunteer studies. One hundred patients (48 men, 52 women; mean age, 52 years ⫾ 12 [standard deviation]) with aneurysmal SAH underwent conventional and diffusion-weighted magnetic resonance (MR) imaging at a mean of 9 days ⫾ 3 after SAH to evaluate possible lesions caused by SAH, treatment of SAH, and vasospasm. Aneurysms were treated surgically (n ⫽ 70) or endovascularly (n ⫽ 30) before MR imaging. Diffusion-weighted MR imaging was performed at 1-year follow-up in 30 patients (10 men, 20 women; mean age, 51 years ⫾ 11). Thirty healthy age-matched volunteers (11 men, 19 women; mean age, 54 years ⫾ 16) underwent MR imaging with an identical protocol. ADC values were measured bilaterally in the gray and white matter (parietal, frontal, temporal, occipital lobes; cerebellum; caudate nucleus; lentiform nucleus; thalamus; and pons) that appeared normal on T2-weighted and diffusion-weighted MR images. Linear mixed model was used for comparison of ADC values of supratentorial gray matter and white matter; general linear regression analysis was used for comparison of ADC values of cerebellum and pons. Results: In patients with SAH, the ADC values in normal-appearing white matter, with a single exception in the frontal lobe (P ⫽ .091), were significantly higher than they were in healthy volunteers (P ⱕ .011). The differences disappeared by 1 year, except in parietal white matter (P ⫽ .045). The ADC values of cortical gray matter did not significantly differ between patients and volunteers (P ⱖ .121). Conclusion: SAH and its treatment may cause global mild vasogenic edema in white matter and deep gray matter that is undetectable on T2-weighted and diffusion-weighted MR images but is detectable by measuring the ADC value in the subacute stage of SAH. 1 From the Departments of Clinical Radiology (Y.L., T.M., M.K., A.K., R.L.V.), Neurosurgery (V.S., T.K., J.R.), and Clinical Neurophysiology (M.K.), Kuopio University Hospital, PO Box 1777, FIN-70211 Kuopio, Finland. Received October 17, 2005; revision requested December 8; revision received January 17, 2006; accepted February 17; final version accepted May 5. Supported by Kuopio University Hospital (EVO funding 5063515) and the Instrumentarium Science Foundation. Address correspondence to Y.L. (e-mail: yawu.liu@kuh.fi ). 娀 RSNA, 2006 姝 RSNA, 2006 518 Radiology: Volume 242: Number 2—February 2007 NEURORADIOLOGY: Subarachnoid Hemorrhage: ADC in Brain after Treatment D iffusion-weighted magnetic resonance (MR) imaging has been used extensively in the evaluation of ischemic stroke. In ischemic brain tissue, water mobility is restricted because of the loss of ionic gradients and translocation of water from the extracellular to the intracellular compartment (cytotoxic edema). Consequently, the apparent diffusion coefficient (ADC), a quantitative value that is calculated with raw data from diffusion-weighted imaging and that represents water diffusivity, is decreased. On the other hand, in vasogenic edema, the ADC value is increased because of a net increase in the extracellular space. Although diffusion-weighted imaging has been used frequently in patients with ischemic stroke, the technique has not been used as much in patients with subarachnoid hemorrhage (SAH). Some primary studies (1–4) with a limited number of patients have shown the usefulness of diffusion-weighted imaging in the detection of acute ischemia in patients with symptomatic vasospasm after SAH. Quantitative measurements of ADC are more sensitive than diffusion-weighted imaging for detection of even mild changes in water diffusivity. Thus, the purpose of our study was to prospectively evaluate whether SAH is associ- Advances in Knowledge 䡲 In patients with subarachnoid hemorrhage, the apparent diffusion coefficient values in normalappearing white matter and deep gray matter, with a single exception in frontal white matter (P ⫽ .091), were significantly increased (P ⱕ .011) in the subacute stage compared with values in healthy volunteers, but they returned to a normal level at 1-year follow-up MR imaging. 䡲 This finding indicates the presence of mild diffuse vasogenic edema in the subacute stage, and the edema is not detectable on conventional T2-weighted MR images. Radiology: Volume 242: Number 2—February 2007 ated with a change in the ADC in normal-appearing brain parenchyma. Materials and Methods Institutional review board approval and informed consent were obtained for all patient and volunteer studies. Study Design During the study period, all patients with aneurysmal SAH and eligibility (as mentioned later) were prospectively scheduled to undergo conventional MR imaging and diffusion-weighted imaging approximately 1 week after SAH to evaluate possible ischemic lesions or other lesions caused by SAH, treatment of SAH, and vasospasm. One-year follow-up conventional MR images and diffusionweighted images were obtained from a randomly selected subgroup. An agematched group of healthy volunteers was used as a control group. The number of patients in the follow-up group and the number of volunteers in the control group were determined with a power analysis. Patients During the study period from January 2002 to July 2004, 245 patients with aneurysmal SAH were admitted to our institution. Of these 245 patients with acute SAH, 92 consecutive patients were prospectively scheduled to undergo conventional MR imaging and diffusion-weighted imaging 5–19 days after initial bleeding. Before that, a pilot study that included eight patients with SAH was conducted with the same MR imaging protocol. Thus, a total of 100 patients (48 men, 52 women; mean age, 52 years ⫾ 12 [standard deviation]; range, 19 – 81 years) were enrolled in our study. Patients were eligible for the present MR imaging study protocol if subarachnoid blood was detected at computed tomography (CT) and a ruptured cerebral aneurysm was verified at three-dimensional rotational angiography. The mean interval from the bleeding to MR imaging examination was 9 days, with a range of 5–19 days. The reasons that MR imaging was not performed in the other 153 patients were Liu et al the following: lack of informed consent, ongoing intensive care unit treatment with a Swan-Ganz catheter (considered to be a contraindication for MR imaging), the patient died soon after admission, the patient was in extremely poor condition so that transfer to the Department of Clinical Radiology was considered too risky, temporary lack of resources of the Department Clinical of Radiology, or treatment delay beyond the study time range. Hunt and Hess grade (5) was assessed by four resident neurosurgeons (with 2– 6 years of experience) and was confirmed by two senior neurosurgeons (T.K., with 13 years of experience; J.R., with 19 years of experience). In Hunt and Hess grades I and II, the patient is asymptomatic or has minimal headache and slight nuchal rigidity; in grade III, the patient is confused and drowsy; in grade IV, the patient is unconscious with or without a localizing neurologic deficit; and in grade V, the patient is in a deep coma with a moribund appearance. The modified Fisher grade (6) was assessed by the same two senior neurosurgeons who conducted the Hunt and Hess assessment to evaluate the amount and distribution of subarachnoid blood. Fisher grade I indicates that no clot is seen on the CT scan, grade II indicates moderate bleeding is observed predominantly in the basal cisterns, grade III indicates more diffuse severe bleeding, Published online before print 10.1148/radiol.2422051698 Radiology 2007; 242:518 –525 Abbreviations: ADC ⫽ apparent diffusion coefficient ROI ⫽ region of interest SAH ⫽ subarachnoid hemorrhage Author contributions: Guarantors of integrity of entire study, Y.L., R.L.V.; study concepts/study design or data acquisition or data analysis/interpretation, all authors; manuscript drafting or manuscript revision for important intellectual content, all authors; manuscript final version approval, all authors; literature research, Y.L., V.S., T.M., T.K.; clinical studies, Y.L., V.S., T.M., T.K., A.K., J.R., R.L.V.; statistical analysis, Y.L., M.K., T.K., R.L.V.; and manuscript editing, Y.L., T.K., R.L.V. Authors stated no financial relationship to disclose. 519 NEURORADIOLOGY: Subarachnoid Hemorrhage: ADC in Brain after Treatment and grade IV indicates an intracerebral or intraventricular clot with diffuse or no subarachnoid clot. The patients’ demographics, Hunt and Hess grades, Fisher grades, locations of aneurysms, and treatment modalities are shown in Table 1. On the basis of data from our previous study (7), a power analysis (1 ⫽ [0.80 ⫾ 0.05] ⫻ 10⫺3 mm2/sec, n1 ⫽ 100, 5% difference, ␣ ⫽ .05,  ⫽ .05, where 1 is the mean ADC value of sample 1 in our previous study [7] and n1 is the number in sample 1) showed that the minimal sample size was 26 for both patients in the follow-up group and healthy volunteers in the control group. MR images and diffusion-weighted images at 1-year follow-up were obtained from 30 patients (10 men, 20 women; mean age, 51 years ⫾ 11; range, 28 – 80 years) who were randomly selected from the 100 patients enrolled in this study. There were no significant differences in sex (P ⫽ .156, 2 test) and age (P ⫽ .290, Mann-Whitney U test) between the 30 patients who were selected and the 100 patients who were enrolled. Volunteers Thirty healthy age-matched volunteers (11 men, 19 women; mean age, 54 years ⫾ 16; range, 22–79 years) also underwent MR imaging with the same diffusion-weighted imaging sequence and imaging parameters and with the same MR imager. The volunteers were imaged within the same time frame during which the patients with subacute stage SAH were imaged. Volunteers were asked about their medical history, especially any neurologic or cardiovascular disturbances, cranial trauma, or permanent medication they were receiving. Any individual who was suspected of having any pathologic medical condition or who was taking permanent medication was excluded. There were no significant differences in sex (P ⱖ .274, 2 test) and age (P ⱖ .426, Mann-Whitney U test) between the group of volunteers and the group of 100 patients with SAH or the 30 patients who had undergone 1-year follow-up MR imaging and diffusionweighted imaging. 520 Treatment According to our current practice, ruptured aneurysms should be treated either surgically or endovascularly within 72 hours from initial bleeding. In our study of 100 patients, this was achieved in 89 (89%) patients, and 96 (96%) patients were treated within 7 days. The other four patients were treated surgically after 11–14 days from onset because of delays before admission to the hospital. All aneurysms, however, were treated surgically (n ⫽ 70) or endovascularly (n ⫽ 30) before MR imaging. All patients with SAH were routinely treated both pre- and postoperatively in the intensive care unit, and they all received nimodipine (Nimotop; Bayer Pharma, Paris, France) and corticosteroid medication (betamethasone, Betapred; Swedish Orphan, Stockholm, Sweden). Symptomatic hydrocephalus was treated with ventriculostomy in the acute stage and later with permanent shunt placement if needed. The Glasgow Coma Scale was recorded daily by the same resident and senior neurosurgeons. Patients who developed symptomatic vasospasm were treated in the intensive care unit with HHH (hypertension, hypervolemia, hemodilution) therapy (8–11) used at many institutions and, if necessary, with angioplasty or intraarterial nimodipine infusion. The clinical criterion for symptomatic vasospasm was a decrease in the Glasgow Coma Scale of two or more scores or the appearance of new localizing symptoms (dysphasia, hemiparesis), with other reasons for deterioration (eg, hydrocephalus, metabolic disorders, postoperative bleeding, and infections) first ruled out. MR Imaging and Evaluation All MR imaging studies were performed with a 1.5-T whole-body imager capable of echo-planar imaging (Magnetom Vision; Siemens Medical Systems, Erlangen, Germany) by using a head coil. The patient’s head was fixed with standard restraints used in routine clinical MR imaging. Diffusion-weighted imaging was performed with a single-shot echo-planar spin-echo sequence (repetition time Liu et al msec/echo time msec, 6000/100). Other imaging parameters were as follows: section thickness, 5 mm; intersection gap, 1.5 mm; field of view, 240 mm; and matrix size, 96 ⫻ 200. Nineteen transverse sections parallel to the orbitomeatal line, which included whole supratentorial and infratentorial brain tissue, were imaged. Four images per same section position were obtained: one T2-weighted image without diffusion weighting (b value, 0 sec/mm2) and three diffusion-weighted images with orthogonally applied diffusion gradients (b value, 1000 sec/mm2). To prevent the effects of diffusion anisotropy, isotropic diffusion-weighted imTable 1 Clinical and Imaging Characteristics of 100 Patients with SAH Characteristic Sex Male Female Age (y)* 19 to ⬍60 ⱕ60 to 81 Location of ruptured aneurysm at digital subtraction angiography Internal carotid artery Middle cerebral artery Anterior cerebral artery Vertebrobasilar arteries Hunt and Hess grade I II III IV Fisher grade at CT II III IV Hydrocephalus at CT Present Absent Symptomatic vasospasm before MR imaging Present Absent Treatment Endovascular coil Surgical clip No. of Patients 48 52 74 26 20 38 29 13 14 49 26 11 26 48 26 23 77 14 86 30 70 * The mean age was 52 years ⫾ 12. Radiology: Volume 242: Number 2—February 2007 NEURORADIOLOGY: Subarachnoid Hemorrhage: ADC in Brain after Treatment ages were reconstructed by calculating the geometric mean of the three images obtained with a b value of 1000 sec/mm2. The ADC maps were generated off-line. The ADC was calculated on a pixel-by-pixel basis as the negative slope of the line fitting the two points for b versus ln(SI), where SI is the signal intensity. The ADC values were measured from bilateral regions in the normal-appearing gray and white matter (parietal, frontal, temporal, and occipital lobes and cerebellum), caudate nucleus, putamen, thalamus, pons, and the body of the lateral ventricle by one radiologist (Y.L.), who had 6 years of experience in interpretation of diffusion-weighted images. In all regions of interest (ROIs), the isotropic diffusion-weighted and conventional MR images were carefully visually reviewed to avoid areas that were affected by susceptibility artifact or focal lesions. If any of the locations were affected by metal susceptibility artifact, leukoencephalopathy, intracranial hematoma, edema, or infarction, the corresponding areas were excluded from the measurements. If possible, identical mirrored regions were used (Figure). The mean size of the ROIs was 35 mm3 ⫾ 22, with a range of 2–164 mm3. Liu et al Statistical Analysis All statistical analyses were performed with software (SPSS, version 11.5.1, November 16, 2002; SPSS, Chicago, Ill). After proving no significant difference between the ADC values of the mirrored ROIs in the right and left hemispheres with the Wilcoxon signed rank test, the values of two sides were averaged and analyzed separately for each anatomic location. If no ROI could be analyzed in a certain anatomic location because of an artifact or a focal lesion, however, only the ADC value of the ROI on the contralateral unaffected hemisphere was used in the analysis instead of an averaged value. The general linear regression was used to compare the difference between the ADC values of patients and those of healthy volunteers and to analyze the association between ADC and factors that were dichotomized with relevant clinical data (age, presence of hydrocephalus, Hunt and Hess grade, Fisher grade, location of aneurysm, presence of symptomatic vasospasm, and treatment) in cerebellar gray matter, cerebellar white matter, the pons, and cerebrospinal fluid. Because the ADC values in cortical gray or white matter (parietal, frontal, temporal, and occipital lobes) or deep gray matter (caudate nucleus, lentiform nucleus, and thalamus) may not be independent of each other, the linear mixed model was used to compare the differences in ADC values between patients and volunteers and to analyze the association between ADC and factors that were dichotomized with relevant clinical data. A difference with P ⬍ .05 was considered statistically significant. Results Transverse ADC maps show ROIs that were drawn bilaterally in brain parenchyma with a normal appearance and include cortical gray matter and supratentorial white matter. Top left: ROIs in parietal and frontal lobes. Bottom left: ROIs in temporal and occipital lobes. Top right: ROIs in caudate nucleus, lentiform nucleus, and thalamus. Bottom right: ROIs in pons and cerebellar gray and white matter. Radiology: Volume 242: Number 2—February 2007 MR Imaging Findings In patients with subacute stage SAH, findings at MR imaging were normal in 26 patients, a single ischemic lesion was observed in 48 patients, and multiple ischemic lesions were observed in 26 patients. In volunteers, MR imaging findings were normal. 521 NEURORADIOLOGY: Subarachnoid Hemorrhage: ADC in Brain after Treatment ADC Values ADC measurements were successfully performed in every area in each volunteer; thus, a total of 840 ROIs were drawn. Among the 100 patients, ROIs could be drawn bilaterally on parietal gray matter in 68 patients, on parietal white matter in 67 patients, on frontal gray matter in 52 patients, on frontal white matter in 51 patients, on the caudate nucleus in 31 patients, on the lentiform nucleus in 41 patients, on the thalamus in 57 patients, on temporal gray matter or white matter in 52 patients, on occipital gray matter in 95 patients, on occipital white matter in 94 patients, on the pons in 100 patients, and on cerebellar gray matter or white matter in 98 patients. A total of 2460 ROIs were thus drawn at normal-appearing areas in patients with the subacute stage of SAH; in the 30 patients who underwent follow-up MR imaging, a total of 747 ROIs were drawn 1 year after SAH. In the patients with SAH, there was no significant difference in ADC of the normal-appearing brain parenchyma between the side of the ruptured aneurysm and the contralateral side in the measured areas (P ⫽ .056 –.907, Wilcoxon signed rank test). In the subacute stage, the ADC values in normal-appearing white matter and deep gray matter, with a single exception in the frontal lobe of supratentorial white matter, were significantly higher in patients with SAH than they were in healthy volunteers (P ⱕ .091) (Table 2). The values in cortical gray matter did not significantly differ between patients and volunteers (Table 2). On average, the ADC value was 4% higher in both normal-appearing white matter and deep gray matter in patients with SAH than it was in healthy volunteers. In the 30 patients who underwent follow-up diffusion-weighted imaging, the elevated ADC values had decreased to a normal level after 1 year from onset, compared with the values in the volunteers. The single exception to this finding was the value in the parietal lobe of supratentorial white matter (P ⫽ .045, comparison of patients at 1-year 522 Liu et al Table 2 ADC Values of Normal-appearing Brain Parenchyma in 100 Patients with Aneurysmal SAH in Subacute Stage and 30 Volunteers Location of Measurements Supratentorial cortical gray matter Parietal lobe Frontal lobe Temporal lobe Occipital lobe Supratentorial white matter Parietal lobe Frontal lobe Temporal lobe Occipital lobe Deep gray matter Caudate nucleus Lentiform nucleus Thalamus Cerebellar gray matter Cerebellar white matter Pons Patients Volunteers P Value 0.73 ⫾ 0.007 0.77 ⫾ 0.01 0.79 ⫾ 0.006 0.76 ⫾ 0.005 0.71 ⫾ 0.01 0.76 ⫾ 0.01 0.78 ⫾ 0.01 0.74 ⫾ 0.01 .141 .391 .533 .121 0.77 ⫾ 0.004 0.80 ⫾ 0.006 0.81 ⫾ 0.007 0.78 ⫾ 0.004 0.75 ⫾ 0.01 0.78 ⫾ 0.01 0.77 ⫾ 0.01 0.75 ⫾ 0.01 .004 .091 .006 ⬍.001 0.78 ⫾ 0.01 0.78 ⫾ 0.01 0.81 ⫾ 0.004 0.74 ⫾ 0.005 0.69 ⫾ 0.004 0.72 ⫾ 0.01 0.75 ⫾ 0.01 0.74 ⫾ 0.01 0.78 ⫾ 0.01 0.72 ⫾ 0.01 0.66 ⫾ 0.004 0.68 ⫾ 0.01 .011 .008 .012 .120 .004 .008 Note.—The values represent estimated marginal means and standard errors of the averaged ADC values (⫻10⫺3 mm2/sec) of the left and right hemispheres. Pairwise comparisons of patients and volunteers were based on estimated marginal means obtained from the linear mixed model for the supratentorial areas and deep gray matter and on data obtained from the general linear regression for the cerebellum and the pons. follow-up vs volunteers) (Table 3). The mean ADC value of cerebrospinal fluid in the body of the lateral ventricle did not significantly differ between volunteers and patients with SAH in the subacute stage ([3.46 ⫾ 0.03] ⫻ 10⫺3 mm2/ sec vs [3.51 ⫾ 0.04] ⫻ 10⫺3 mm2/sec, P ⫽ .232) and between volunteers and patients 1 year later ([3.46 ⫾ 0.03] ⫻ 10⫺3 mm2/sec vs [3.43 ⫾ 0.05] ⫻ 10⫺3 mm2/sec, P ⫽ .284). ADC Values and Clinical Comparisons Associations between age and the measured ADC values were statistically significant; the elderly patients (ⱖ60 years old) with SAH had higher ADC values than did the younger patients (Table 4). The presence of hydrocephalus, Hunt and Hess grade, severity of bleeding (Fisher grade), location of aneurysm, presence of symptomatic vasospasm before MR imaging, and modality of treatment were not significantly associated with ADC in the normal-appearing brain parenchyma. In the control population, the ADC values did not significantly differ between the elderly individuals (ⱖ60 years old) and the younger individuals (⬍60 years old) in any area (P ⱖ .074), with the single exception of the temporal gray matter (P ⫽ .032). Discussion We evaluated the ADC values of white matter and deep and cortical gray matter that had a normal appearance on diffusion-weighted images and T2-weighted MR images in patients with SAH. In the subacute stage of SAH, the ADC values were increased in the white matter and deep gray matter, with a single exception in the frontal white matter, in patients with SAH compared with healthy volunteers. This finding suggested the existence of mild global vasogenic edema, rather than cytotoxic edema; cytotoxic edema indicates ischemia or other irreversible damage of the brain tissue. Cytotoxic edema is characterized by a reduced ADC, whereas vasogenic edema is characterized by an elevated ADC, even if both entities may appear similar on T2-weighted images and diffusion trace images. To complicate the situation, in ischemic stroke with cytotoxic edema, the areas show reduced ADC Radiology: Volume 242: Number 2—February 2007 NEURORADIOLOGY: Subarachnoid Hemorrhage: ADC in Brain after Treatment in the acute stage but show so-called pseudonormalization with elevated ADC approximately 1 week after ictus. Our patients were imaged 5–19 days after hemorrhage, but the pseudonormalization effect in an infarcted area can be ruled out because there was no high T2 signal intensity in the measured areas. Our results suggest that mild global edema of the brain tissue is relatively common after SAH. Previously, the frequency of occurrence of global edema had been reported to be less than 12% in patients with SAH at CT (12). In animal models, an increase in the water content in the brain after rupture of an aneurysm has been shown by calculating the weight difference between wet and dried brain tissue and by comparing this difference with the corresponding value in control animals (13). To our knowledge, global vasogenic edema after aneurysmal SAH in the brain areas with a normal appearance on T2-weighted MR images and diffusion-weighted images, however, has not been previously reported. A number of mechanisms have been Liu et al proposed to explain global edema after SAH. Those mechanisms include diffuse ischemic injury due to transient ictal cerebral circulation arrest (14), diffuse inflammatory or neurotoxic effects of widespread subarachnoid blood and its degradation products on brain tissue (15), or abnormal autoregulation (16). Vasogenic edema with an increased ADC has been described in hypertensive encephalopathy (17), hyperperfusion after carotid endarterectomy (18), venous thrombosis (18), reversible posterior leukoencephalopathy (18), and eclampsia (19). Furthermore, ADC has been found to be increased in cerebral edema during acute ketoacidosis (20). Researchers have speculated that lesions in basal ganglia occur because of increased permeability of small perforating vessels, which in turn is caused by endothelial damage and breakdown in cerebrovascular autoregulation from hypertension (17). In our population of patients with SAH, the cause of elevated ADC values is probably multifactorial and in part may be explained by hyper- tensive periods, altered cerebral autoregulation, neurotoxic effects, and treatment in the intensive care unit with hypervolemia and hemodilution. Vasogenic edema after SAH also can be considered a direct consequence of increased permeability of the bloodbrain barrier. In animal models, the blood-brain barrier permeability changes after experimental SAH reveal a reversible pattern with time (13). In the clinical setting, an impairment of the bloodbrain barrier has been found in nearly two-fifths of patients within 5 days of SAH. The majority of these patients developed vasospasm and ischemic complications in the later stage of SAH and had a poor prognosis (21). In our study, the patients underwent initial MR imaging at approximately 9 days after ictus, and there were no significant differences in ADC in cortical areas between patients and volunteers. One explanation might be that the possible blood-brain barrier dysfunction in cortical gray matter had already returned to normal by the time of initial MR imaging. Increased ADC values, however, were still ob- Table 3 ADC Values of Volunteers and Patients with Aneurysmal SAH Who Participated in 1-year Follow-up Location of Measurements Supratentorial cortical gray matter Parietal lobe Frontal lobe Temporal lobe Occipital lobe Supratentorial white matter Parietal lobe Frontal lobe Temporal lobe Occipital lobe Deep gray matter Caudate nucleus Lentiform nucleus Thalamus Cerebellar gray matter Cerebellar white matter Pons Volunteers (n ⫽ 30) Patients (n ⫽ 30) Subacute SAH Follow-up 0.71 ⫾ 0.01 0.76 ⫾ 0.01 0.78 ⫾ 0.01 0.74 ⫾ 0.01 0.75 ⫾ 0.01 0.78 ⫾ 0.01 0.79 ⫾ 0.01 0.75 ⫾ 0.01 0.71 ⫾ 0.01 0.76 ⫾ 0.01 0.79 ⫾ 0.01 0.75 ⫾ 0.01 0.75 ⫾ 0.01 0.78 ⫾ 0.01 0.77 ⫾ 0.01 0.75 ⫾ 0.01 0.78 ⫾ 0.01 0.81 ⫾ 0.01 0.84 ⫾ 0.01 0.79 ⫾ 0.01 0.74 ⫾ 0.01 0.75 ⫾ 0.01 0.78 ⫾ 0.01 0.72 ⫾ 0.01 0.66 ⫾ 0.01 0.68 ⫾ 0.01 0.78 ⫾ 0.01 0.78 ⫾ 0.01 0.81 ⫾ 0.01 0.74 ⫾ 0.01 0.69 ⫾ 0.01 0.72 ⫾ 0.01 P Value Follow-up vs Volunteer Subacute SAH vs Follow-up .025 .161 .227 .440 .912 .860 .371 .553 .025 .142 .906 .968 0.78 ⫾ 0.01 0.79 ⫾ 0.01 0.79 ⫾ 0.01 0.77 ⫾ 0.01 .013 .062 ⬍.001 .001 .045 .757 .172 .140 .859 .230 .051 .447 0.74 ⫾ 0.01 0.77 ⫾ 0.01 0.78 ⫾ 0.01 0.72 ⫾ 0.01 0.68 ⫾ 0.01 0.71 ⫾ 0.01 .002 .014 .005 .107 .004 .009 .939 .075 .993 .591 .079 .151 .029 .643 .017 .065 .228 .441 Subacute SAH vs Volunteer Note.—The values represent estimated marginal means and standard errors of the averaged ADC values (⫻10⫺3 mm2/sec) of the left and right hemispheres. Pairwise comparisons were based on estimated marginal means obtained from the linear mixed model for the supratentorial areas and deep gray matter and on data obtained from the general linear regression for the cerebellum and the pons. Radiology: Volume 242: Number 2—February 2007 523 NEURORADIOLOGY: Subarachnoid Hemorrhage: ADC in Brain after Treatment Liu et al Table 4 ADC versus Clinical Data in 100 Patients Clinical Data Age (y) ⬍60 ⱖ60 Hydrocephalus Absent Present Hunt and Hess grade II III and IV Fisher grade I and II III and IV Aneurysm location Anterior circulation Vertebrobasilar artery Symptomatic vasospasm before MR imaging Absent Present Treatment Surgical clip Endovascular coil Cerebellar White Supratentorial Supratentorial White Cerebellar Gray Matter† Cortical Gray Matter* Matter* Deep Gray Matter* Matter† No. of P P P P P Patients ADC Value ADC Value ADC Value ADC Value ADC Value ADC Pons† P Value 74 26 0.76 ⫾ 0.01 .198 0.77 ⫾ 0.01 0.77 ⫾ 0.01 .001 0.80 ⫾ 0.01 0.80 ⫾ 0.01 .01 0.82 ⫾ 0.01 0.74 ⫾ 0.01 .719 0.74 ⫾ 0.01 0.69 ⫾ 0.01 .208 0.71 ⫾ 0.01 0.70 ⫾ 0.01 .001 0.75 ⫾ 0.02 77 23 0.77 ⫾ 0.01 .516 0.76 ⫾ 0.01 0.79 ⫾ 0.01 .512 0.78 ⫾ 0.01 0.80 ⫾ 0.01 .448 0.81 ⫾ 0.01 0.74 ⫾ 0.01 .609 0.75 ⫾ 0.01 0.69 ⫾ 0.01 .102 0.71 ⫾ 0.01 0.71 ⫾ 0.01 .058 0.74 ⫾ 0.02 63 37 0.77 ⫾ 0.01 .702 0.76 ⫾ 0.01 0.79 ⫾ 0.01 .106 0.78 ⫾ 0.01 0.81 ⫾ 0.01 .67 0.81 ⫾ 0.01 0.74 ⫾ 0.01 .664 0.74 ⫾ 0.01 0.70 ⫾ 0.01 .87 0.70 ⫾ 0.01 0.73 ⫾ 0.01 .743 0.72 ⫾ 0.01 26 74 0.76 ⫾ 0.01 .33 0.77 ⫾ 0.01 0.78 ⫾ 0.09 .456 0.79 ⫾ 0.07 0.81 ⫾ 0.01 .89 0.81 ⫾ 0.01 0.74 ⫾ 0.01 .262 0.75 ⫾ 0.01 0.70 ⫾ 0.01 .782 0.70 ⫾ 0.01 0.72 ⫾ 0.02 .245 0.73 ⫾ 0.01 87 13 0.76 ⫾ 0.01 .962 0.76 ⫾ 0.01 0.79 ⫾ 0.01 .585 0.78 ⫾ 0.01 0.81 ⫾ 0.01 .967 0.81 ⫾ 0.01 0.74 ⫾ 0.01 .893 0.74 ⫾ 0.02 0.70 ⫾ 0.01 .799 0.70 ⫾ 0.01 0.73 ⫾ 0.01 .916 0.72 ⫾ 0.02 86 14 0.76 ⫾ 0.01 .125 0.77 ⫾ 0.01 0.79 ⫾ 0.01 .777 0.78 ⫾ 0.01 0.80 ⫾ 0.01 .298 0.82 ⫾ 0.01 0.74 ⫾ 0.01 .597 0.75 ⫾ 0.02 0.70 ⫾ 0.01 .406 0.71 ⫾ 0.01 0.73 ⫾ 0.01 .615 0.72 ⫾ 0.02 70 30 0.77 ⫾ 0.01 .588 0.76 ⫾ 0.01 0.78 ⫾ 0.01 .279 0.79 ⫾ 0.01 0.81 ⫾ 0.01 .533 0.81 ⫾ 0.01 0.74 ⫾ 0.01 .524 0.75 ⫾ 0.01 0.70 ⫾ 0.01 .749 0.70 ⫾ 0.01 0.73 ⫾ 0.02 .363 0.72 ⫾ 0.01 Note.—The values represent estimated marginal means and standard errors of the averaged ADC values of left and right hemispheres. * Linear mixed model was used. † General linear regression was used. served in cerebral and cerebellar white matter, the pons, and deep gray matter in the subacute stage. The brain seems to be more vulnerable to damage in elderly patients with SAH. In our study, the ADC values were significantly higher in white matter and deep gray matter in elderly patients (ⱖ60 years old) than in younger patients (⬍60 years old). This finding indicates that the blood-brain barrier was more severely impaired in elderly patients. This result seems to agree with findings in previous studies (12,22) in which older age was related to higher morbidity and poorer neurologic outcome after SAH. Our study results suggest that diffuse vasogenic edema is associated with neither the patients⬘ clinical neurologic condition nor the location of the ruptured aneurysm. Severe global edema detectable at CT is associated with loss 524 of consciousness at ictus (12,23,24), but no corresponding association was found in our study. The ADC measurement is much more sensitive than is CT in the detection of even mild edema. In our study, there was no significant difference in ADC values between patients with a good clinical condition versus those with a poorer clinical condition (Hunt and Hess grades I and II vs grades III and IV) nor between patients with symptomatic vasospasm versus patients without symptomatic vasospasm before MR imaging. The most likely explanation for that finding might be the fact that only normal-appearing brain tissue was examined, and the areas with more severe edema that showed hyperintensity on T2-weighted MR images were excluded. Moreover, patients who currently were receiving hypertension, hypervolemia, hemodilution (HHH) treatment because of clinical vasospasm did not undergo MR imaging because of the use of the Swan-Ganz catheter. Thus, we were unable to investigate the possible changes in ADC values related to coexistent vasospasm. Patients who had minor symptoms indicative of vasospasm at the time of MR imaging did not receive active HHH therapy in the intensive care unit. Rupture of an aneurysm in the posterior circulation was a predictor of vasospasm in a recent study (25). Our results indicate that the location of the ruptured aneurysm does not have an important role in the existence of mild vasogenic edema. The ADC in cortical gray matter did not significantly differ between the volunteers and the patients on ADC maps at both the subacute stage and 1-year follow-up. Performance of the ROI analysis only in the cortical gray matter, however, is demanding. The layer of the gray matter is relatively thin, and beRadiology: Volume 242: Number 2—February 2007 NEURORADIOLOGY: Subarachnoid Hemorrhage: ADC in Brain after Treatment cause of the partial volume effect, the voxel in the 5-mm-thick section often also contains subcortical white matter. It is also important to avoid the cerebrospinal fluid in the sulci to prevent falsely high ADC values. The ADC values in the white matter and deep gray matter measured in our study were comparable with those reported in the literature. There exists variation in the published values in cortical gray matter, however, and our results tended to be low (26,27). This finding may be related to the different selection and size of ROIs, and, probably, our results reflect values that are for a combination of cortical gray and subcortical white matter. There were limitations of our study. First, although the ADC values in patients with SAH in the subacute stage were significantly higher in normal-appearing white matter and deep gray matter than in healthy volunteers, with a single exception in frontal white matter, it is difficult to apply a universal cutoff value in the daily clinical practice to detect global edema. Second, all the patients in our study received nimodipine and corticosteroids. The medication might affect the ADC values. The effects of these medications could not be evaluated in this study, and it was not possible to define the mechanism of vasogenic edema, nor its potential effect on neurologic and psychological outcome, merely with the findings of our study. Third, the metal artifact from clips might potentially affect the ADC; however, the areas with a metal artifact were excluded from the ADC measurements. Furthermore, results of the 1-year follow-up study suggested that the ADC values had returned to normal levels while the surgical clips and endovascular coils remained in place. In addition, only 13 of 100 patients had aneurysms in the posterior circulation. In the majority of the patients, the clips were far from the cerebellum, but the ADC values of cerebellar white matter were still higher than they were in the control population. To conclude, in the subacute stage of SAH after treatment, ADC values in the normal-appearing white matter and deep gray matter, with a single exception in the frontal white matter, are Radiology: Volume 242: Number 2—February 2007 higher in patients than they are in a healthy control population. The possible explanations for this observation include hypertensive periods, altered autoregulation, neurotoxic effects, and prophylactic treatment with hypervolemia and hemodilution. Clinical and neuropsychological outcome after SAH depends on many different factors that often are interrelated. The possible predictive value for outcome of elevated ADC values in the subacute stage needs further study. Acknowledgment: We express our gratitude to Vesa Kiviniemi, PhLic, for statistical consultation. Liu et al bral vasospasm after aneurysmal subarachnoid hemorrhage. Stroke 1995;26:1620 –1626. 12. Claassen J, Carhuapoma JR, Kreiter KT, Du EY, Connolly ES, Mayer SA. Global cerebral edema after subarachnoid hemorrhage: frequency, predictors, and impact on outcome. Stroke 2002;33: 1225–1232. 13. Germano A, d’Avella D, Imperatore C, Caruso G, Tomasello F. Time-course of blood-brain barrier permeability changes after experimental subarachnoid haemorrhage. Acta Neurochir (Wien) 2000;142:575–580. 14. Shigeno T, Fritschka E, Brock M, Schramm J, Shigeno S, Cervos-Navarro J. Cerebral edema following experimental subarachnoid hemorrhage. Stroke 1982;13:368 –379. 15. Germano AF, Dixon CE, d’Avella D, Hayes RL, Tomasello F. Behavioral deficits following experimental subarachnoid hemorrhage in the rat. J Neurotrauma 1994;11:345–353. 1. Rordorf G, Koroshetz WJ, Copen WA, et al. Diffusion- and perfusion-weighted imaging in vasospasm after subarachnoid hemorrhage. Stroke 1999;30:599 – 605. 16. Handa Y, Hayashi M, Takeuchi H, Kubota T, Kobayashi H, Kawano H. Time course of the impairment of cerebral autoregulation during chronic cerebral vasospasm after subarachnoid hemorrhage in primates. J Neurosurg 1992;76: 493–501. 2. Condette-Auliac S, Bracard S, Anxionnat R, et al. Vasospasm after subarachnoid hemorrhage: interest in diffusion-weighted MR imaging. Stroke 2001;32:1818 –1824. 17. Schwartz RB, Mulkern RV, Gudbjartsson H, Jolesz F. Diffusion-weighted MR imaging in hypertensive encephalopathy: clues to pathogenesis. AJNR Am J Neuroradiol 1998;19:859 – 862. 3. Leclerc X, Fichten A, Gauvrit JY, et al. Symptomatic vasospasm after subarachnoid haemorrhage: assessment of brain damage by diffusion and perfusion-weighted MRI and single-photon emission computed tomography. Neuroradiology 2002;44: 610 – 616. 18. Schaefer PW, Gonzalez RG, Hunter G, Wang B, Koroshetz WJ, Schwamm LH. Diagnostic value of apparent diffusion coefficient hyperintensity in selected patients with acute neurologic deficits. J Neuroimaging 2001;11:369 –380. References 4. Phan TG, Huston J 3rd, Campeau NG, Wijdicks EF, Atkinson JL, Fulgham JR. Value of diffusionweighted imaging in patients with a nonlocalizing examination and vasospasm from subarachnoid hemorrhage. Cerebrovasc Dis 2003;15:177–181. 5. Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg 1968;28:14 –20. 6. Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 1980;6:1–9. 7. Liu Y, Karonen JO, Vanninen RL, et al. Detecting the subregion proceeding to infarction in hypoperfused cerebral tissue: a study with diffusion and perfusion weighted MRI. Neuroradiology 2003;45:345–351. 8. American Heart Association. International cardiovascular disease statistics. Dallas, Tex: American Heart Association, 2003. 9. Bederson JB, Awad IA, Wiebers DO, et al. Recommendations for the management of patients with unruptured intracranial aneurysms: a statement for healthcare professionals from the Stroke Council of the American Heart Association. Circulation 2000;102:2300 –2308. 10. Awad IA, Carter LP, Spetzler RF, Medina M, Williams FC Jr. Clinical vasospasm after subarachnoid hemorrhage: response to hypervolemic hemodilution and arterial hypertension. Stroke 1987;18:365–372. 11. Mori K, Arai H, Nakajima K, Tajima A, Maeda M. Hemorheological and hemodynamic analysis of hypervolemic hemodilution therapy for cere- 19. Engelter ST, Provenzale JM, Petrella JR. Assessment of vasogenic edema in eclampsia using diffusion imaging. Neuroradiology 2000;42:818 – 820. 20. Glaser NS, Wootton-Gorges SL, Marcin JP, et al. Mechanism of cerebral edema in children with diabetic ketoacidosis. J Pediatr 2004;145:164 – 171. 21. Doczi T. The pathogenetic and prognostic significance of blood-brain barrier damage at the acute stage of aneurysmal subarachnoid haemorrhage: clinical and experimental studies. Acta Neurochir (Wien) 1985;77:110 –132. 22. Ogilvy CS, Carter BS. A proposed comprehensive grading system to predict outcome for surgical management of intracranial aneurysms. Neurosurgery 1998;42:959 –968. 23. Lagares A, Gomez PA, Alen JF, Lobato RD, Campollo J. Global cerebral edema after subarachnoid hemorrhage [letter]. Stroke 2002;33:2153– 2154. 24. Claasen J, Mayer SA. Reply. Stroke 2002;33: 2154. 25. McGirt MJ, Mavropoulos JC, McGirt LY, et al. Leukocytosis as an independent risk factor for cerebral vasospasm following aneurysmal subarachnoid hemorrhage. J Neurosurg 2003;98: 1222–1226. 26. Ulug AM, Beauchamp N Jr, Bryan RN, van Zijl PC. Absolute quantitation of diffusion constants in human stroke. Stroke 1997;28:483– 490. 27. Helenius J, Soinne L, Perkiö J, et al. Diffusionweighted MR imaging in normal human brains in various age groups. AJNR Am J Neuroradiol 2002;23:194 –199. 525