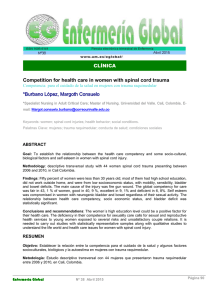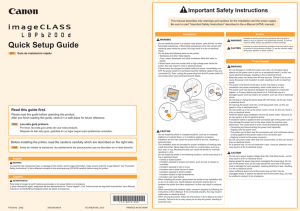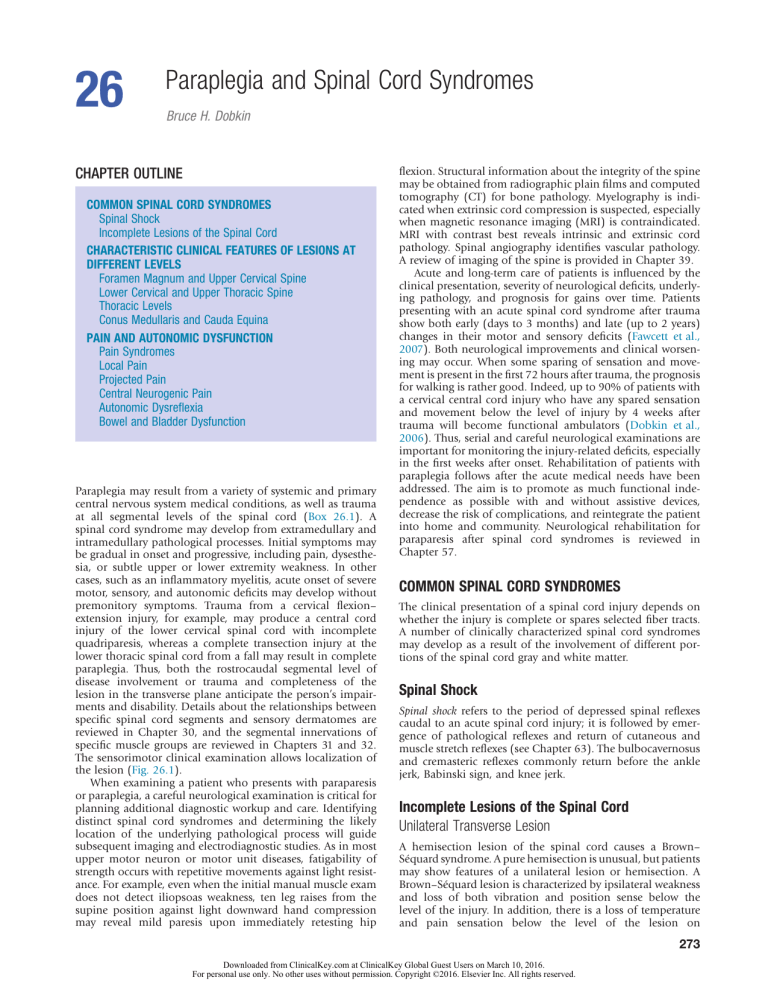
26 Paraplegia and Spinal Cord Syndromes Bruce H. Dobkin CHAPTER OUTLINE COMMON SPINAL CORD SYNDROMES Spinal Shock Incomplete Lesions of the Spinal Cord CHARACTERISTIC CLINICAL FEATURES OF LESIONS AT DIFFERENT LEVELS Foramen Magnum and Upper Cervical Spine Lower Cervical and Upper Thoracic Spine Thoracic Levels Conus Medullaris and Cauda Equina PAIN AND AUTONOMIC DYSFUNCTION Pain Syndromes Local Pain Projected Pain Central Neurogenic Pain Autonomic Dysreflexia Bowel and Bladder Dysfunction Paraplegia may result from a variety of systemic and primary central nervous system medical conditions, as well as trauma at all segmental levels of the spinal cord (Box 26.1). A spinal cord syndrome may develop from extramedullary and intramedullary pathological processes. Initial symptoms may be gradual in onset and progressive, including pain, dysesthesia, or subtle upper or lower extremity weakness. In other cases, such as an inflammatory myelitis, acute onset of severe motor, sensory, and autonomic deficits may develop without premonitory symptoms. Trauma from a cervical flexion– extension injury, for example, may produce a central cord injury of the lower cervical spinal cord with incomplete quadriparesis, whereas a complete transection injury at the lower thoracic spinal cord from a fall may result in complete paraplegia. Thus, both the rostrocaudal segmental level of disease involvement or trauma and completeness of the lesion in the transverse plane anticipate the person’s impairments and disability. Details about the relationships between specific spinal cord segments and sensory dermatomes are reviewed in Chapter 30, and the segmental innervations of specific muscle groups are reviewed in Chapters 31 and 32. The sensorimotor clinical examination allows localization of the lesion (Fig. 26.1). When examining a patient who presents with paraparesis or paraplegia, a careful neurological examination is critical for planning additional diagnostic workup and care. Identifying distinct spinal cord syndromes and determining the likely location of the underlying pathological process will guide subsequent imaging and electrodiagnostic studies. As in most upper motor neuron or motor unit diseases, fatigability of strength occurs with repetitive movements against light resistance. For example, even when the initial manual muscle exam does not detect iliopsoas weakness, ten leg raises from the supine position against light downward hand compression may reveal mild paresis upon immediately retesting hip flexion. Structural information about the integrity of the spine may be obtained from radiographic plain films and computed tomography (CT) for bone pathology. Myelography is indicated when extrinsic cord compression is suspected, especially when magnetic resonance imaging (MRI) is contraindicated. MRI with contrast best reveals intrinsic and extrinsic cord pathology. Spinal angiography identifies vascular pathology. A review of imaging of the spine is provided in Chapter 39. Acute and long-term care of patients is influenced by the clinical presentation, severity of neurological deficits, underlying pathology, and prognosis for gains over time. Patients presenting with an acute spinal cord syndrome after trauma show both early (days to 3 months) and late (up to 2 years) changes in their motor and sensory deficits (Fawcett et al., 2007). Both neurological improvements and clinical worsening may occur. When some sparing of sensation and movement is present in the first 72 hours after trauma, the prognosis for walking is rather good. Indeed, up to 90% of patients with a cervical central cord injury who have any spared sensation and movement below the level of injury by 4 weeks after trauma will become functional ambulators (Dobkin et al., 2006). Thus, serial and careful neurological examinations are important for monitoring the injury-related deficits, especially in the first weeks after onset. Rehabilitation of patients with paraplegia follows after the acute medical needs have been addressed. The aim is to promote as much functional independence as possible with and without assistive devices, decrease the risk of complications, and reintegrate the patient into home and community. Neurological rehabilitation for paraparesis after spinal cord syndromes is reviewed in Chapter 57. COMMON SPINAL CORD SYNDROMES The clinical presentation of a spinal cord injury depends on whether the injury is complete or spares selected fiber tracts. A number of clinically characterized spinal cord syndromes may develop as a result of the involvement of different portions of the spinal cord gray and white matter. Spinal Shock Spinal shock refers to the period of depressed spinal reflexes caudal to an acute spinal cord injury; it is followed by emergence of pathological reflexes and return of cutaneous and muscle stretch reflexes (see Chapter 63). The bulbocavernosus and cremasteric reflexes commonly return before the ankle jerk, Babinski sign, and knee jerk. Incomplete Lesions of the Spinal Cord Unilateral Transverse Lesion A hemisection lesion of the spinal cord causes a Brown– Séquard syndrome. A pure hemisection is unusual, but patients may show features of a unilateral lesion or hemisection. A Brown–Séquard lesion is characterized by ipsilateral weakness and loss of both vibration and position sense below the level of the injury. In addition, there is a loss of temperature and pain sensation below the level of the lesion on 273 Downloaded from ClinicalKey.com at ClinicalKey Global Guest Users on March 10, 2016. For personal use only. No other uses without permission. Copyright ©2016. Elsevier Inc. All rights reserved. 274 PART I Common Neurological Problems BOX 26.1 Differential Diagnosis of Diseases Affecting the Spinal Cord COMPRESSIVE LESIONS Non-neoplastic Trauma: Vertebral body fracture/dislocation Hyperextension injury Direct puncture, stab, or missile Spondylosis: Cervical stenosis Lumbar stenosis Intervertebral disk herniation Infectious disorders (e.g., abscess, tuberculosis) Inflammatory (e.g., rheumatoid arthritis, ankylosing spondylitis, sarcoid) Hemorrhage: Epidural hematoma Congenital disorders Arachnoid cysts Paget disease Osteoporosis Neoplastic Epidural metastasis Intradural extramedullary (e.g., meningioma, neurofibroma, leptomeningeal metastasis) Intramedullary NONCOMPRESSIVE MYELOPATHIES Demyelinating (e.g., MS, ADEM) Hereditary (e.g., spastic paraplegia) Viral myelitis (e.g., varicella-zoster, AIDS–related myelopathy, human T-lymphotropic virus type I infection) Syringomyelia Vitamin B12 deficiency and other nutritional deficiencies Infarction Ischemia and hemorrhage from vascular malformations or cavernoma Spirochetal diseases (syphilis and Lyme disease) Toxic myelopathies (e.g., radiation-induced) Autoimmune diseases (e.g., lupus, Sjögren syndrome) Paraneoplastic Neuronal degenerations Tethered cord at the cauda equina Acute and subacute transverse myelitis of unknown cause ADEM, Acute disseminated encephalomyelitis; AIDS, acquired immunodeficiency syndrome; AVM, arteriovenous malformation; MS, multiple sclerosis. the contralateral side. As pain and temperature fibers extend rostrally a few segments before crossing the midline to enter the lateral spinothalamic tract, the loss of pain and temperature sensory modalities extends rostrally on the contralateral side to a segmental level that is a few segments below the level of the lesion. In addition, at the segmental level of the hemisection injury, a limited patch of ipsilateral loss of pain and temperature in combination with a lower motor neuron weakness is often detected. A Brown–Séquard syndrome may be caused by a variety of etiologies but is commonly encountered after traumatic injuries, including bullet and stab wounds. Central Cord Syndrome Traumatic central cord syndrome is commonly characterized by the triad of (1) motor impairment that is disproportion- ately more severe in the upper than the lower extremities, (2) bladder dysfunction that usually includes urinary retention, and (3) sensory dysfunction of varying degrees. An international consensus group suggested that an upper and lower extremity difference of at least 10 motor score points, based on the Medical Research Council scale, can be considered as a quantitative addition to the commonly used qualitative criteria for making the diagnosis (van Middendorp et al., 2010). An additional clinical feature of the traumatic central cord syndrome is a dissociated sensory loss for pain and temperature, whereas vibration and position sense remain preserved. This sensory presentation may be explained by a direct injury to intramedullary decussating fibers, which normally would ascend contralaterally as part of the spinothalamic tract. As a result, a capelike sensory deficit may be encountered in patients with a cervical level injury, but sensation within more caudal dermatomes would generally be spared (Fig. 26.2). A traumatic central cord syndrome is mostly encountered in elderly patients who have suffered a relatively minor trauma in the form of a cervical hyperextension injury, commonly in the setting of an underlying cervical spondylosis. Falls and motor vehicle injuries are common etiologies. Syringomyelia or tumors may also produce a central cord syndrome. Anterior Spinal Artery Syndrome An anterior cord syndrome involves the anterior two-thirds of the spinal cord, sparing the posterior columns. The cortico­ spinal and spinothalamic tracts are both affected. The syndrome is clinically characterized by paralysis and sensory impairments below the level of the lesion, with impaired sensation of pain and temperature; vibration sense and proprioception are preserved. Fiber tracts for autonomic control are also typically compromised, resulting in bladder, bowel, and sexual dysfunction. In the acute phase after injury, a spinal shock phase with decreased muscle tone and areflexia may present, followed by a gradual return of reflexes and hypertonicity and perhaps spasms. An anterior cord syndrome may be caused by trauma from central disk compression or a bone fragment, as well as a myelitis. Vascular occlusive causes are perhaps the most common etiology. For instance, the anterior cord syndrome may present as a spinal cord stroke from atherothrombotic or embolic occlusion of the anterior spinal cord artery. Invasive vascular and thoraco-abdominal surgical procedures may be complicated by impaired blood flow to the spinal cord, especially due to obstruction or hypoperfusion of the artery of Adamkiewicz near the T6 level. This may also follow surgery at the distal aorta and proximal iliac arteries with the use of aortic counter pulsation devices and, occasionally, from retroperitoneal hematomas or abscesses. Similarly, survivors of cardiac arrest and significant hypotensive episodes may demonstrate a mid-thoracic anterior cord ischemic syndrome, as the vascular supply near the T6 segment is particularly susceptible to distal field ischemia. Anterior Horn and Pyramidal Tract Syndromes Paralysis may be encountered in the setting of motor impairments in combination with relative sparing of sensory and autonomic functions, as seen in motor neuron disease including amyotrophic lateral sclerosis (ALS). Lower motor neuron weakness with atrophy and loss of reflexes is typically seen in combination with upper motor neuron weakness, signs of spasticity, and hyper-reflexia. Different limbs may be affected to various degrees, but symptoms are progressive over the course of the disease. However, innervation of the external anal and urethral sphincters is normally preserved in ALS, with sparing of bladder and bowel functions. Downloaded from ClinicalKey.com at ClinicalKey Global Guest Users on March 10, 2016. For personal use only. No other uses without permission. Copyright ©2016. Elsevier Inc. All rights reserved. Paraplegia and Spinal Cord Syndromes 275 Analgesia Loss of vibratory and position sense Combined loss Complete transection of thoracic cord (lesion at T10) Right hemisection of thoracic cord (lesion at T3) Early intra-axial lesion of thoracic cord at T3 –T6 (syringomyelic suspended pattern) Advanced intra-axial lesion of thoracic cord at T3 –T6 (sacral sparing) Anterior spinal artery syndrome (lesion at T4) Cauda equina lesion Right S1 radiculopathy Peripheral neuropathy (glove stocking sensory loss) Fig. 26.1 Characteristic sensory disturbances found in various spinal cord lesions in comparison with peripheral neuropathy. Combined Posterior and Lateral Column Disease A clinical syndrome characterized by development of a spastic ataxic gait pattern may be caused by lesions affecting the posterior and lateral white-matter tracts. Friedreich ataxia represents a genetic etiology, and vitamin B12 deficiency may result in subacute combined degeneration with spastic paretic gait and sensory ataxia. Dorsal horn and column injury alone may result from tabes dorsalis. CHARACTERISTIC CLINICAL FEATURES OF LESIONS AT DIFFERENT LEVELS Paralysis may be caused by lesions at any segmental level of the spinal cord from both intramedullary and extramedullary disease. The characteristic symptoms and signs affecting motor and sensory functions typically depend on the segmental level of injury. Foramen Magnum and Upper Cervical Spine When structural lesions are located in or adjacent to the foramen magnum, several different neurological patterns are possible. For example, brainstem signs may occur together with symptoms from a spinal cord injury. Involvement of the lower portion of the brainstem is suggested by speech impairments, including dysarthria and dysphonia, as well as by dysphagia. In addition, facial numbness and nystagmus may be detected in association with tumors or other structural lesions in the foramen magnum. When compression of the spinal cord occurs, long-tract signs may present from injury to the corticospinal tract with, for instance, a spastic hemiparesis or quadriparesis. A lower motor neuron injury component may also be detectable from lesions at the craniocervical junction and the foramen magnum, with upper extremity weakness, muscular atrophy, and decreased muscle stretch reflexes. Several pathological processes and lesions may be present at the level of the foramen magnum and its immediate vicinity. These conditions include Arnold–Chiari malformations; traumatic injuries; rheumatoid arthritis; syringomyelia; vascular lesions such as vertebral artery thrombosis, dissection, or an arteriovenous malformation; and a variety of tumors including meningiomas. Multiple sclerosis may also cause intramedullary lesions of the brainstem and the upper cervical spinal cord and selectively affect long white-matter tracts. Imaging studies, especially MRI, help determine the nature and precise anatomical location for pathological processes in the foramen magnum and upper cervical spine region. Lesions affecting the uppermost portion of the cervical spine may be challenging to diagnose owing to a nonlocalizing symptom complex upon initial presentation. Pain is a common early symptom and may be localized to the neck or occipital region. At times, the pain may be aggravated by neck movement. When upper cervical nerve roots are compressed, a radicular pain may present in the corresponding dermatome. Irritation of the second cervical nerve root, for example, may present with a pain localized within the posterior aspect of the scalp, whereas an injury to the third and fourth nerve roots Downloaded from ClinicalKey.com at ClinicalKey Global Guest Users on March 10, 2016. For personal use only. No other uses without permission. Copyright ©2016. Elsevier Inc. All rights reserved. 26 276 PART I Common Neurological Problems disks) that compress individual segmental nerve roots or spinal nerves. Intramedullary lesions may also present with pain, but the segmental localization is commonly less precise. Extramedullary lesions typically first irritate segmental nerve roots and the spinal nerve, with radicular pain and sensory deficits typically following the corresponding dermatomal distribution. Similarly, motor deficits involve each myotome affected by the lesion. Muscle stretch reflexes may also provide helpful information with regard to the primary level of injury, as the affected segmental reflex is typically depressed or absent, and caudal reflexes are hyperactive. For instance, when a lesion is at the C4–C6 level, a radicular pattern of pain and sensory symptoms may typically involve the radial side of the arm, forearm, and hand. Motor deficits include weakness in elbow flexion. In addition, the biceps and brachioradialis muscle stretch reflexes may be depressed or absent, especially when the C5–C6 levels are involved. In contrast, lesions at the C7–T1 level usually present with pain and sensory impairments over the ulnar side of the upper extremity, including the arm, forearm, and hand. Motor deficits related to affected myotomes commonly involve elbow extension, the intrinsic hand muscles, and the triceps reflex. Lower and upper motoneuron signs may also be present in adjacent segments. If segmental nerve roots and the spinal cord are compressed by a herniated disk or space-occupying lesion at the C5–C6 level, for example, a decreased brachioradialis reflex may reflect a C6 radiculopathy, whereas a brisk and hyperactive finger flexor reflex reflects an upper motoneuron syndrome. Thoracic Levels Fig. 26.2 Magnetic resonance image of the cervical spine showing a contrast-enhancing mass. Patient presented with a capelike sensory loss for pain and temperature. Resection of the mass revealed a glioma. may induce pain that is projected to the neck or shoulder. A lower motoneuron injury presentation with upper extremity muscular weakness and atrophy may also be part of the clinical presentation. When the spinal cord is compressed by epidural or subdural space-occupying lesions, spastic weakness of upper and lower extremities typically follows. An injury or disease process affecting the upper cervical spinal cord may also compromise breathing. Normal respiration requires functional use of the diaphragm muscle, which is innervated by the phrenic nerve. Motoneurons contributing to the phrenic nerve are located within the cervical spinal cord and contribute efferent axons to the C3–C5 ventral roots. Therefore, complete injuries affecting the spinal cord above the C3 segment will compromise the function of the diaphragm, and respiratory failure may follow. Lower Cervical and Upper Thoracic Spine Injuries to the lower part of the cervical spine and upper thoracic spine may be caused by extramedullary compression of nerve roots and the spinal cord or by an intramedullary disease process. The correlation between presenting symptoms and localization of the underlying lesion is most precise for the extramedullary pathological processes (e.g., tumors, herniated Traumatic spinal cord injury at the thoracic level usually produces a complete lesion. The segmental level of injury is best determined by a careful sensory examination of dermatomes. Useful clinical landmarks are the nipple line for the T4 dermatome and the umbilicus for the T10 dermatome. Pain may follow a radicular pattern around the chest or abdomen, corresponding to the segmental levels of injury. Sensory testing of pin, temperature, pressure, and light touch appreciation may determine the most caudal dermatome of normal sensation, as well as a zone of partial preservation. The sensory testing should include evaluation of dermatomes of the left and right side of the body, with comparisons of homologous levels. In addition to a combination of at-level pain, sensory deficits, and muscular weakness, autonomic dysfunction may develop from long-tract involvement and include urinary retention, bladder–sphincter dyssynergia, and bladder hyper-reflexia. Conus Medullaris and Cauda Equina The conus medullaris of the spinal cord terminates approximately at the level of the L1 vertebra, although the precise location of the tip of the conus may show marked variability among subjects. This anatomical aspect of the spinal cord is important because spine trauma commonly takes place at the thoracolumbar junction, and the extent of such injuries is highly variable (Kingwell et al., 2008). Traumatic injuries to the conus medullaris usually result in weakness or paralysis of the lower extremities, absence of lower extremity reflexes, and saddle anesthesia (Fig. 26.3). However, some patients with conus medullaris injuries exhibit a mixed upper and lower motoneuron syndrome. In contrast, a cauda equina injury that lesions lumbosacral roots below the level of the conus medullaris is a pure lower motoneuron syndrome. Cauda equina injuries present with lower extremity weakness, areflexia and decreased muscle tone, and variable sensory deficits. At least Downloaded from ClinicalKey.com at ClinicalKey Global Guest Users on March 10, 2016. For personal use only. No other uses without permission. Copyright ©2016. Elsevier Inc. All rights reserved. Paraplegia and Spinal Cord Syndromes Post Ant 277 root distribution often is found immediately after the walk and resolves within a minute or two. PAIN AND AUTONOMIC DYSFUNCTION In addition to motor and sensory impairments, pain and dysfunction in the autonomic nervous system can aid localization of spinal cord syndromes. Pain is frequently associated with spinal cord injuries, along with autonomic impairments that may affect blood pressure and heart rate, bladder, bowel, sexual, and cardiorespiratory functions. The type and severity of autonomic dysfunction depends on the location of pathology and severity of the spinal cord injury. International spinal cord injury societies recommend a systematic approach to document remaining autonomic function after a spinal cord injury (Alexander et al., 2009). CM L2 CE Fig. 26.3 Magnetic resonance imaging demonstrating the effects of trauma to the thoracolumbar portion of the spine with a crush injury of the cauda equina (CE) and conus medullaris (CM) portion of the spinal cord. Note T12/L1-level spine fracture and dislocation. Pain Syndromes Distinct pain syndromes may develop as a result of compression, inflammation, or injury to the vertebral column, ligaments, the dura mater, nerve roots, dorsal horn, and ascending spinal cord sensory tracts. Neuropathic pain may take the form of paresthesia (abnormal but not unpleasant sensation that is either spontaneous or evoked), dysesthesia (an abnormal, unpleasant sensation that is spontaneous or evoked), allodynia (pain evoked by ordinary stimuli such as touch or rubbing), and hyperalgesia (an augmented response to a stimulus that is usually painful). Local Pain a third of these patients suffer considerable central pain. Affected limb and pelvic floor muscles develop flaccid weakness, and electromyography shows denervation after either a conus medullaris or cauda equina injury, especially following anatomically complete lesions. Both conus medullaris and cauda equina injuries are associated with bladder, bowel, and sexual dysfunction. Urodynamic evaluations typically demonstrate detrusor areflexia, and a rectal exam identifies a flaccid anal sphincter. In addition, the bulbocavernosus reflex is typically absent or diminished, and reflexogenic erection in males is commonly lost. Imaging studies (e.g., plain radiographs, CT, MRI) identify structural pathology. Burst fractures and fracture dislocations are common injuries to the spinal column that result in neurological deficits, suggesting a conus medullaris or cauda equina involvement. Following trauma to the thoracolumbar spine, imaging studies can be used to assess spinal stability and identify detailed aspects of spine fractures, including the presence and location of bone fragments, spinal canal encroachment, epidural hematomas, and herniated disks. A variety of treatment options exist (e.g., surgical stabilization of the spine, decompression of the conus medullaris and nerve roots). A lumbar spinal stenosis due to a congenitally smalldiameter spinal canal or central disk and spondylotic narrowing one or more levels below L1 may present with a subtle course. Over months to years, lower extremity numbness or pain, usually in an L3–S1 single or multiradicular pattern, accompanies standing and walking, often gradually progressing to limit walking distance. Pain is commonly accompanied by weakness, but patients may not be aware of their deficit. Clinical insight into this diagnosis and the upper level of cauda compression is gained by a manual muscle examination after a few minutes of being supine, followed by having the subject walk for about 500 feet, and then immediately retesting strength. Transient paresis or greater paresis in the affected Localized neck or back pain may result from irritation or injury to innervated spine structures including ligaments, periosteum, and dura. The pain is typically deep and aching, may vary with a change in position, and often becomes worse from increased load or weight bearing on affected structures. Percussion or palpation over the spine may in some patients worsen the local pain. When the injured or diseased spine structures are irritated, secondary symptoms may develop and include muscle spasm and a more diffusely located pain. Musculoligamentous sources of pain often persist for more than a week post spine surgery and develop with compensatory overuse of joints and muscles. Such pain must be distinguished from central neurogenic pain, but can amplify it. Projected Pain A pathological process involving the facet joints may be experienced as focal or radiating pain in an upper or lower extremity. When a nerve root is irritated or injured, the projected pain is radicular. Radicular pain commonly has a sharp, stabbing quality or causes dysesthesia. It may be exacerbated by activities that stretch the affected nerve root (e.g., straight leg raising or flexion of the neck). Straining or coughing may also increase the intensity and severity of radicular pain. Nerve root irritation may also result in sensory and motor deficits following the same dermatome and myotome distribution as the affected nerve root. This helps localize the level of spinal cord injury that is causing paraplegia. Central Neurogenic Pain Paresthesia, dysesthesia, allodynia, and hyperalgesia accompany injury to the spinal cord in at least half of patients, as well as after thalamocortical stroke. Regardless of segmental level or completeness of injury, most patients with a traumatic spinal Downloaded from ClinicalKey.com at ClinicalKey Global Guest Users on March 10, 2016. For personal use only. No other uses without permission. Copyright ©2016. Elsevier Inc. All rights reserved. 26 278 PART I Common Neurological Problems cord injury develop a clinically significant pain syndrome at some post-lesion time point (Waxman and Hains, 2006). Neuropathic pain after spinal cord injury may affect different locations. At-level pain is primarily derived from local cellular and neuroplastic changes in the dorsal horn and sensory roots at the segments of injury. Below-level pain is located in body segments receiving innervation from the spinal cord caudal to the lesioned segments. Above-level neurogenic pain is less common. Pain developing after a spinal cord injury is commonly described as burning, pricking, or aching in quality. It can be experienced as deep or superficial. Some patients develop a severe and excruciating pain syndrome after cord or cauda trauma that is at-level and below-level even in the absence of any cutaneous or proprioceptive sensation, which requires centrally acting medications to control. The most recently FDA-approved medication for spinal pain is pregabaline. The mechanisms for such painful phantom phenomena are not well understood but include structural and molecular dorsal horn, thalamic, and cortical adaptations to ordinary and noxious inputs. Autonomic Dysreflexia Injuries to the spinal cord that result in paraplegia from a lesion above T6 may also impair autonomic control and result in episodes of severe hypertension or hypotension. Autonomic dysreflexia represents an acute syndrome characterized by excessive and uncontrolled sympathetic output from the spinal cord. As a result, the blood pressure is suddenly and markedly elevated. Associated symptoms include headache; malaise; blurring of vision; flushed, sweaty skin above the level of injury; and pale, cool skin below it. An episode of autonomic dysreflexia can be triggered by any noxious stimulation below the segmental level of injury. Common triggers include bladder distension, constipation, rectal fissures, joint injury, and urinary tract infection. Autonomic dysreflexia may present soon after the initial injury but more commonly becomes symptomatic several months after the spinal cord injury. Prevention is the best approach. Treatment of acute symptoms targets removal of noxious stimuli and cautious lowering of the blood pressure (see Chapter 63). Bowel and Bladder Dysfunction Normal bladder and bowel control depend on segmental reflexes involving both autonomic and somatic motor neurons, as well as descending and ascending tracts of the spinal cord (Fowler et al., 2008). As a result, bladder and bowel function may be impaired after an injury to any segmental level of the spinal cord. Different clinical syndromes develop depending on whether the injury or disease process affects the sacral spinal cord directly or higher segmental levels. Traumatic spinal cord injuries with paraplegia taking place above the T12 vertebra will interrupt spinal cord long-tract connections between supraspinal micturition centers in the brainstem and cerebral cortex and the sacral spinal cord. An upper motoneuron syndrome follows, with detrusor–sphincter dyssynergia caused by impaired coordination of autonomic and somatic motor control of the bladder detrusor and external urethral sphincter, respectively. Incomplete bladder emptying results. In addition, the upper motoneuron syndrome also includes detrusor hyper-reflexia with increased pressure within the bladder. In contrast, injury to the T12 vertebra and below results in a direct lesion to the sacral spinal cord and associated nerve roots. A direct lesion to preganglionic parasympathetic neurons and somatic motoneurons of the Onuf nucleus located within the S2–S4 spinal cord segments results in denervation of pelvic targets. Injuries to both the conus medullaris and cauda equina present as a lower motoneuron syndrome characterized by weak or flaccid detrusor function. Urinary retention follows, with risk of overflow incontinence. The goal for all bladder care is to avoid retrograde urine flow, urinary tract infections, and renal failure. Management of both upper and lower motoneuron bladder impairment commonly includes clean intermittent bladder catheterizations. Chapter 47 discusses evaluation and treatment. REFERENCES The complete reference list is available online at https://expertconsult .inkling.com/. Downloaded from ClinicalKey.com at ClinicalKey Global Guest Users on March 10, 2016. For personal use only. No other uses without permission. Copyright ©2016. Elsevier Inc. All rights reserved. Paraplegia and Spinal Cord Syndromes REFERENCES Alexander, M.S., Biering-Sorensen, F., Bodner, D., et al., 2009. International standards to document remaining autonomic function after spinal cord injury. Spinal Cord 47, 36–43. Dobkin, B., Apple, D., Barbeau, H., et al., 2006. Weight-supported treadmill vs over-ground training for walking after acute incomplete SCI: a multicenter randomized clinical trial. Neurolo. 66, 484–493. Fawcett, J.W., Curt, A., Steeves, J.D., et al., 2007. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 45, 190–205. 278.e1 Fowler, C.J., Griffiths, D., de Groat, W.C., 2008. The neural control of micturition. Nat. Rev. Neurosci. 9, 453–466. Kingwell, S.P., Curt, A., Dvorak, M.F., 2008. Factors affecting neurological outcome in traumatic conus medullaris and cauda equina injuries. Neurosurg. Focus 25, E7. van Middendorp, J.J., Pouw, M.H., Hayes, K.C., et al., 2010. Diagnostic criteria of traumatic central cord syndrome. Part 2: A questionnaire survey among spine specialists. Spinal Cord 48, 657–663. Waxman, S.G., Hains, B.C., 2006. Fire and phantoms after spinal cord injury: Na+ channels and central pain. Trends Neurosci. 29, 207–215. Downloaded from ClinicalKey.com at ClinicalKey Global Guest Users on March 10, 2016. For personal use only. No other uses without permission. Copyright ©2016. Elsevier Inc. All rights reserved. 26