The Aging Male
ISSN: 1368-5538 (Print) 1473-0790 (Online) Journal homepage: https://www.tandfonline.com/loi/itam20
Predictors of low bone mineral density in elderly
males with chronic obstructive pulmonary disease:
the role of body mass index
Alessandra Coin, Giuseppe Sergi, Sara Marin, Andrea Vianello, Egle
Perissinotto, Silvia Sarti, Giulia Rinaldi, Marco Mosele, Emine M Inelmen,
Giuliano Enzi & Enzo Manzato
To cite this article: Alessandra Coin, Giuseppe Sergi, Sara Marin, Andrea Vianello, Egle
Perissinotto, Silvia Sarti, Giulia Rinaldi, Marco Mosele, Emine M Inelmen, Giuliano Enzi &
Enzo Manzato (2010) Predictors of low bone mineral density in elderly males with chronic
obstructive pulmonary disease: the role of body mass index, The Aging Male, 13:2, 142-147, DOI:
10.3109/13685531003657784
To link to this article: https://doi.org/10.3109/13685531003657784
Published online: 29 Apr 2010.
Submit your article to this journal
Article views: 210
View related articles
Citing articles: 3 View citing articles
Full Terms & Conditions of access and use can be found at
https://www.tandfonline.com/action/journalInformation?journalCode=itam20
The Aging Male, June 2010; 13(2): 142–147
Predictors of low bone mineral density in elderly males with chronic
obstructive pulmonary disease: the role of body mass index
ALESSANDRA COIN1, GIUSEPPE SERGI1, SARA MARIN1, ANDREA VIANELLO2,
EGLE PERISSINOTTO3, SILVIA SARTI1, GIULIA RINALDI1, MARCO MOSELE1,
EMINE MERAL INELMEN1, GIULIANO ENZI1, & ENZO MANZATO1
1
Geriatrics Division, Department of Medical and Surgical Sciences, University of Padova, Padova, Italy, 2Respiratory
Pathophysiology Department, City Hospital of Padova, Padova, Italy, and 3Department of Environmental Medicine and
Public Health, University of Padova, Padova, Italy
(Received 28 August 2009; revised 7 December 2009; accepted 12 January 2010)
Abstract
Objective. The aim of this study was to investigate the relationships between nutritional indices (Body mass index (BMI),
serum albumin), sarcopenia, bone mineral density (BMD) and the severity of their pulmonary obstruction in elderly patients
with chronic obstructive pulmonary disease (COPD).
Methods. The method involved was a prospective transversal study; 82 males >65 years old, 41 stable patients with COPD
and 41 healthy elderly individuals (controls). All subjects underwent spirometry, biochemical analyses and dual energy X-ray
absorptiometry. The significance of the differences between mean values and prevalence rates was tested. The relationships
between BMD and independent predictors were analysed by multiple linear regressions. Logistic regression models were
applied on dichotomised variables.
Results. In patients with COPD, the prevalence of osteoporosis was higher in subjects with sarcopenia (46% vs. 0%;
p 5 0.05) and with BMI 5 25.1 kg/m2 (58% vs. 15%; p 5 0.02). Multiple regression analysis indicated that BMI,
appendicular skeletal muscle mass (ASMM), albumin, and forced expiration volume after 1 s (FEV1) explained the 70% of
BMD variability at the hip and 56% at the spine. Logistic regression showed that a BMI 5 25.1 kg/m2 was independently
associated with osteoporosis risk (OR ¼ 10.0; 95%CI 1.3–76); no independent effect emerged for FEV1% (5and 50%).
Conclusion. In elderly males with COPD, the BMI values 25 kg/m2 are more strongly related to low BMD levels than
albumin values. Among those patients, BMI values within the normal range for younger adults might point out a higher risk
of osteoporosis.
Keywords: Body mass index, albumin, sarcopenia, airflow obstruction, osteoporosis
Introduction
Bone loss has been recognised as one of the systemic
effects of chronic obstructive pulmonary disease
(COPD) [1]. Many factors are involved in this
process, including airflow obstruction, but nutritional
disorders may have a key role [2–4]. It is known, in
fact, that malnutrition and underweight are common
among individuals suffering from COPD, supported
by a negative energy balance due to a low dietary
intake and a higher than normal resting energy
expenditure [5,6]. Also muscle mass depletion
(sarcopenia), which occurs physiologically with ageing and is exacerbated by COPD, may have an
additional role -in combination with malnutrition- in
bone frailty [7].
Body mass index (BMI) is widely used for nutritional assessment and several studies have shown that
a low BMI is associated with bone loss in elderly men
and women [8,9].
In our hypothesis, in patients with COPD the
presence of a chronic inflammatory condition and
the airflow obstruction per sè might cause bone loss
even when nutritional indices suggest a normal
nutritional status and muscle mass is not much
depleted. It could be reasonable to assume that COPD
might lead to bone loss and the onset of osteoporosis
even at normal BMI values. It could be also likely that
hypoalbuminemia and sarcopenia (measured by the
appendicular skeletal muscle mass: ASMM) might
represent useful indices for the early identification of
Correspondence: Dr. Alessandra Coin, Clinica Geriatrica – Ospedale Giustinianeo (28 piano), via Giustiniani 2, 35128, Padova, Italy.
Tel: þ0039-049-8218949. Fax: þ0039-049-8211218. E-mail: alessandra.coin@unipd.it
ISSN 1368-5538 print/ISSN 1473-0790 online Ó 2010 Informa UK Ltd.
DOI: 10.3109/13685531003657784
BMI and BMD in elderly COPD
patients with COPD at risk of bone mass loss,
irrespective of their BMI.
The aims of this study were to investigate the
relationship between some nutritional indices (BMI,
serum albumin), sarcopenia (ASMM) and bone
mineral density (BMD) at different sites in elderly
patients with COPD, also in relation to the severity of
their pulmonary obstruction.
Methods
Study subjects
This survey was conducted at the Geriatrics Department of Padua University on 82 males over 65 years of
age, 41 of whom had COPD, diagnosed according to
the European Respiratory Society criteria [10], (age
range 66–85 years). The patients with COPD were
recruited consecutively from among the outpatients
attending the Respiratory Pathophysiology Department in Padua for routine check-ups. Only patients
with COPD in stable clinical conditions were considered. Patients with fever, worsening respiratory
symptoms, leukocytosis (WC > 11.00 6 109/l), an
increased erythrocyte sedimentation rate (ESR)
(>34 mm/h), changes to their medication in the
previous 30 days, or hospital admissions in the
previous 6 weeks were considered clinically unstable
and ruled out. A history of oral or systemic corticosteroid use for more than 3 months consecutively was
also reason for exclusion from the study. The allowable
drugs were beta 2 agonists (taken by 64% of the
patients recruited), inhaled corticosteroids (56%) and
anticholinergic agents (41%).
Forty-one healthy elderly people were considered as
a control group, recruited on a voluntary basis from
among the elderly people attending the Geriatrics
Department for a check-up (age range 66–87 years).
Their healthy condition was established from their
clinical history, clinical examination, normal biochemical tests and normal lung function (forced
expiration volume after 1 s: FEV1% > 80).
Other exclusion criteria common to all participants
were: BMI 5 22 or 30 and cognitive or physical
impairments severe enough to prevent them from
taking the tests. The choice of the common exclusion
criteria was finalised to the creation of two groups
comparable for all variables potentially associated
with BMD.
The study design complied with the provisions of
the Helsinki Declaration of 1995. Participants were
fully informed as to the nature and purpose of the
study and gave their informed consent.
All subjects took several tests on the same
morning, as follows:
Physical function and smoking habits
The Rosow and Breslau [11] and NAGI [12] scales
were applied to patients and controls. The NAGI
143
scale investigates nine items (able in bending,
stooping or crouching, pushing or pulling a great
load like a chair, lifting loads inferior or superior to
4.5 kg, reaching shoulders, writing or using small
objects, standing during 15 min, sitting during
30 min) and scores from 0 (totally able in the
investigated physical functions) and 9 (totally unable). The Rosow and Breslau scale assesses three
gross mobility items (doing heavy works at home or
outdoor, climbing stairs, walking 800 m) and scores
from 0 (totally able) or 3 (totally unable). Information on smoking habits was obtained from the
patients, who were classified as non-smokers, exsmokers and current smokers. For smokers, the
number of cigarettes/day and of years of smoking
habit was also recorded.
Anthropometry
Body weight was measured to the nearest 0.1 kg and
height was measured to the nearest 0.1 cm with
subjects wearing light clothing and no shoes. BMI
was calculated as the weight in kilograms divided by
the height in meters squared.
Pulmonary function tests
Lung function was assessed using a computerised
water-sealed Stead-Wells spirometer (BAIRES System, Biomedin, Padua, Italy), which meets the 1994
ATS recommendations for diagnostic spirometry. An
arterial blood sample was drawn from the radial
artery for blood gas analysis of PaO2 and PaCO2.
Biochemical analyses
Blood samples were obtained in the morning after a
12-h overnight fast. Besides normal routine biochemical parameters, analyses were performed for
principal nutritional indices as well as albumin, prealbumin and retinol-binding protein (RBP). Among
skeletal markers 25-OH D3, total calcium and
phosphate were collected, while it was not possible
to investigate the parathyroid hormone, the alkaline
phosphatase, osteocalcin or other products of bone
turnover.
Bone and body composition
Bone parameters, fat-free mass (FFM) and fat mass
(FM) were measured using a dual-energy X-ray fan
beam densitometer (Hologic QDR 4500 W) and
dedicated software, rel 8.2. BMD, T-score and Zscore of the lumbar spine and the hip (neck,
trochanter and total hip) were measured using
standard protocols. The definition of osteoporosis
and osteopenia was conventionally based on the
number of standard deviations (T-score) below the
mean BMD of a gender-specific, young adult
reference population [13]: a T-score between 71.5
144
A. Coin et al.
and 72.5 indicates osteopenia, a T-score 5 72.5
indicates osteoporosis.
ASMM was also measured as the sum of the fatfree soft tissue masses of the arms and legs [14]. The
ASMM index (ASMMI) was calculated as the
ASMM divided by height squared. As a cut-off for
a definition of sarcopenia, we used 7.26 kg/m2, as
proposed by Baugmartner for males, which represents the sex-specific ASMMI value two standard
deviations below the ASMMI mean value for young
adults [15]. We also identified a pre-sarcopenic
condition in subjects whose ASMMI was between
two and one standard deviations below the reference
group’s mean, i.e. with an ASMMI in the range of
7.26–8.40 kg/m2.
Statistical analysis
Data were analysed using the Systat statistical software, rel. 9.1 for Windows (SPSS, Chicago). Results
were expressed as means + standard deviations.
Differences between means in COPD and healthy
individuals were evaluated using Student’s unpaired
two-sided t-test. The prevalence of specific conditions
was expressed as a percentage, and differences
between groups were evaluated using the w-squared
test, exact Fisher’s test or the Cochran-Armitage test
for trend, as appropriate. Analysis of variance or the
Kruskal–Wallis test were applied, as appropriate, to
compare two or more mean values among patients
with COPD. Pearson’s product-moment correlation
coefficient (r) was used to measure simple linear
associations between total hip, trochanter, neck of hip
and lumbar BMD, and age, ASMM, BMI, serum
albumin, FEV1%, FM, FFM, in each group. Stepwise multiple linear regression was used to assess the
independent association between BMD at different
sites and the significantly associated factors emerging
from the previous simple linear analysis (i.e. BMI,
serum albumin, ASMM, FEV1%), adjusted for
confounding factors (age, smoking habit and use of
medication), where necessary. The interaction between covariates was assessed using first- and secondorder interaction terms in the regression models.
Partial and multiple R2 coefficients were estimated
and R2 was used as a criterion of fit. To test for multicollinearity, a variance inflation factor was calculated
for each independent variable in the model. Values
above 2 were used to indicate a multi-collinearity
problem in the model.
A confirmatory analysis was performed by applying
a multivariate logistic model entering dichotomised
predictors. The outcome binary variable was the
presence or absence of osteoporosis.
The explanatory variables were categorised as
follows: BMI on the first tertile of distribution
(BMI 5 25.1 kg/m2) and FEV1% on the 50%
cut-off, indicating severity of obstruction [16].
The model was adjusted for use of inhaled corticosteroids.
The odds ratio (OR) and 95% confidence interval
(CI) for each independently-associated condition
were assessed. The level of significance was set at
0.05 for all tests.
Results
The mean age was similar in patients with COPD
and control subjects (75.7 + 5.3 years vs. 76.0 + 5.8
years; p ¼ 0.38). The Rosow–Breslau and NAGI
scales indicated no differences in physical function
between the two groups (2.0 + 1.1 vs. 1.1 + 1.4;
p ¼ 0.13 and 2.2 + 2.1 vs. 1.4 + 2.1; p ¼ 0.32). Also,
smoking habits did not differ significantly between
groups. Anthropometric data, pulmonary indices,
nutritional, body composition and bone parameters
for the patients with COPD and healthy subjects are
shown in Table I. As expected, no significant
differences emerged between the anthropometric
parameters of the two groups. The spirometric values
were significantly lower in the COPD cases than in
controls, the former being more hypoxemic and
hypercapnic. Mean albumin was significantly lower
in patients with COPD, while no significant difference emerged between COPD cases and controls for
pre-albumin, RBP, 25-OH D3, total calcium or
phosphate. Patients with COPD had significantly
lower FFM and ASMM, both in kg and after
correction for height squared. BMD was significantly
lower in the lumbar region of patients with COPD
(0.95 + 0.17 vs. 1.08 + 0.16, p 5 0.001) and in the
neck of the hip (0.73 + 0.14 vs. 0.80 + 0.13,
p 5 0.05), while no significant differences were seen
for the other sites considered (Table II). The
prevalence of osteoporosis was 29.7% in the COPD
group and 5.0% among the healthy elderly individuals (p 5 0.01).
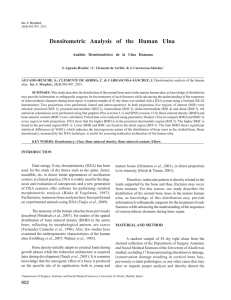
In patients with COPD, the prevalence of osteoporosis increased significantly from 0% in the nonsarcopenic group to 46% in the sarcopenic one
(Figure 1). According to BMI (cut off: 25.1 kg/m2),
the prevalence of osteoporosis in COPD subjects,
rose significantly (to 58%) in the lower BMI group
(Figure 1) (p 5 0.02). In patients with COPD,
osteopenia and osteoporosis were not related to
PaO2, PaCO2, age or smoking habits (data not
shown). Only the lumbar BMD value and T-score
were statistically associated with inhaled corticosteroids (p 5 0.01), their values being lower in steroid
users (data not shown).
Simple correlation analysis (Table II) on the
patients with COPD indicated that BMI, ASMM,
serum albumin and FEV1 were significantly associated with BMD in the hip (total, trochanter and
neck) and lumbar spine.
In the multiple linear regression (Table II), the
model explained 70% of total hip BMD variability
(54% in the trochanter and 47% in the neck) and
56% of the spine BMD. At all hip sites, BMI and
FEV1 retained their independent role in explaining
BMI and BMD in elderly COPD
145
Table I. Anthropometry, blood gas and spirometric parameters, nutritional, body composition and bone indices, in patients with COPD
and controls.
COPD (41), mean + SD
Controls (41), mean + SD
75.7 + 5.3
167.8 + 6.8
71.8 + 12.1
25.4 + 3.5
75.0 + 13.1**
41.6 + 5.2*
1.4 + 0.5**
53.1 + 17.6**
48.9 + 9.8**
38.3 + 5.4**
277.0 + 63.0
47.6 + 12.8
53.1 + 41.0
9.5 + 0.4
2.3 + 1.0
18.0 + 6.1
50.7 + 6.2**
20.9 + 3.2*
7.4 + 0.9*
0.95 + 0.17**
71.47 + 1.53**
70.26 + 1.48**
0.85 + 0.18
71.18 + 1.22
70.11 + 1.07
0.73 + 0.14*
71.54 + 1.18*
0.01 + 1.07*
0.661 + 0.146
70.95 + 1.23
70.18 + 1.09
76.0 + 5.8
169.3 + 6.4
73.9 + 9.1
25.7 + 2.6
98.38 + 15.8
36.8 + 3.9
2.9 + 0.6
110.9 + 22.5
73.3 + 8.3
43.0 + 4.7
301.8 + 72.2
53.6 + 13.9
42.6 + 37.6
9.2 + 0.5
2.7 + 0.4
17.8 + 4.8
55.3 + 6.2
22.6 + 3.2
7.8 + 0.8
1.08 + 0.16
70.23 + 1.46
0.89 + 1.78
0.93 + 0.14
70.67 + 1.11
0.35 + 1.26
0.80 + 0.13
70.92 + 1.17
0.64 + 1.31
0.715 + 0.128
70.45 + 1.16
0.34 + 1.29
Age
Height (cm)
Weight (kg)
BMI (kg/m2)
PaO2 (mmHg)
PaCO2 (mmHg)
FEV1 (l)
FEV1 (% predicted)
FEV1/VC (%)
Albumin (g/l) (n.v. 35–52)
Prealbumin (mg/l) (n.v. 200–400)
RBP (mg/l) (n.v. 30–60)
25-OH D3 (nmol/l) (n.v. > 80)
Total calcium (mg/dl) (n.v. 8.1–10.4)
Phosphate (mg/dl) (n.v. 2.5–4.8)
FM (kg)
FFM (kg)
ASMM (kg)
ASMMI (kg/m2)
BMD lumbar (g/cm2)
T-score lumbar
Z-score lumbar
BMD total hip (g/cm2)
T-score total hip
Z-score total hip
BMD neck (g/cm2)
T-score neck
Z-score neck
BMD trochanteris (g/cm2)
T-score trochanteris
Z-score trochanteris
BMI, body mass index (weight 7 height squared); FEV1, forced expiration volume after 1 s; VC, vital capacity; FFM, fat-free mass; FM, fat
mass; ASMM, appendicular skeletal muscle mass; FFMI, FFM index; FMI, FM index; ASMMI, ASMM index; RBP, retinol-binding
protein; BMD, bone mineral density; n.v., normal values.
COPD vs. controls (*p 5 0.05,**p 5 0.01).
Table II. Simple and multiple partial R2 for linear relationships between hip and lumbar spine BMD and BMI, albumin, ASMM and FEV1.
Lumbar BMD{
Total hip BMD
Simple linear, R2
BMI
ASMM (kg)
Albumin(g/l)
FEV1 (l)
0.60**
0.45**
0.26**
0.14*
Multiple partial, R2
0.62***
0.01
0.00
0.08**
Total multiple, R2 ¼ 0.70
Simple linear, R2
0.17**
0.20**
0.15**
0.18*
0.00
0.00
0.12*
0.04
Total multiple, R2 ¼ 0.56
Trochanteris BMD
Simple linear, R
BMI
ASMM (kg)
Albumin (g/l)
FEV1 (l)
0.41**
0.39**
0.28**
0.11*
2
Neck BMD
Multiple partial, R
0.42***
0.01
0.03
0.08*
Total multiple, R2 ¼ 0.54
Multiple partial, R2
2
Simple linear, R
0.33**
0.35**
0.28**
0.28*
2
Multiple partial, R2
0.32***
0.01
0.05*
0.09*
Total multiple, R2 ¼ 0.47
{
Regression model adjusted for inhaled corticosteroids (partial R2 ¼ 0.40; p 5 0.001).
BMD, bone mineral density; BMI, body mass index; ASMM, appendicular skeletal muscle mass; FEV1, forced expiration volume after 1 s.
*p 5 0.05; **p 5 0.01;***p 5 0.001.
BMD, while ASMM failed to reach significance.
Among the femoral sites, albumin significantly
entered the models only for the neck of the hip. At
spinal level, only albumin had an independent role in
the model, where the inhaled corticosteroids explained 40% of the total variability of the BMD. No
146
A. Coin et al.
Figure 1. Prevalence of normal BMD (open columns), osteopenia
(gray columns), osteoporosis (black columns) in patients with
COPD by ASMMI class (normal: ASMMI 8.4; pre-sarcopenic:
7.26 5 ASMMI 5 8.4; sarcopenic: ASMMI 5 7.26)*, and BMI
dichotomised on first tertile of distribution (25.1 kg/m2)x. *The
statistical analysis was performed comparing the prevalence of
osteoporosis between groups: Cochran-Armitage test for trend:
p 5 0.05; xExact Fisher’s test: p 5 0.02.
collinearity effects emerged with a variance inflating
factor greater than 1.7.
In the logistic regression model, a BMI 5 25.1 kg/
m2 was independently associated with the risk of
osteoporosis (OR ¼ 10.0; 95%CI: 1.3–76.9). COPD
severity resulted not an independent predictor of
osteoporosis (p ¼ 0.98).
Discussion
The groups of healthy elderly individuals and
patients with COPD did not differ statistically in
terms of age, weight, height and BMI, so any
differences between their nutritional and bone
variables would be attributable to the COPD. These
patients, in fact, had significantly lower values for
FFM, ASMM, ASMMI and a 14% greater prevalence of sarcopenia than controls. A reduced FFM
is a known feature of patients with COPD [17],
particularly involving the peripheral skeletal muscles.
Age-related muscle loss is accelerated by COPD,
especially in the acute phase, when higher levels of
circulating pro-inflammatory cytokines cause a higher protein turnover, hypoxemia and acidosis, further
restricting physical activity [18]. Similar factors may
be responsible for the loss of bone mass observed in
patients with COPD [19,20]: as in these previous
studies, there was a significantly higher prevalence of
osteopenia and osteoporosis in our sarcopenic group
of COPD cases. The role of pro-inflammatory
cytokines may be crucial to osteoporosis in association with inflammatory disease [21]. Unfortunately,
more specific markers of inflammation, such as highsensitivity CRP, IL1, IL6, etc., were not measured in
our patients, who were selected for their normal ESR
and leukocyte values as a clinical expression of stable
COPD.
Mean BMD, T-scores and Z-scores were lower in
our patients with COPD than in controls at all sites,
though the differences were only significant for the
neck of the hip and the spine. These two sites consist
mainly of trabecular bone and have a higher
metabolic turnover, making them more sensitive to
the catabolic effect of pro-inflammatory cytokines.
BMI has an important role among the numerous
factors affecting bone mass in healthy elderly people,
as demonstrated in a number of large epidemiological studies [8]. This association has been attributed
to biomechanical forces [22] and to a greater
aromatisation of androgens at subcutaneous adipose
tissue level [23]. In our patients with COPD, BMI
explained 60% of the variability in total hip BMD
and, in the logistic regression model, the risk of
osteoporosis increased 10-fold in the BMI
class 5 25.1 kg/m2. In the older generally, BMI
values below 22 (considered normal in younger
adults) are already associated with a greater risk of
malnutrition, osteoporosis and mortality [9,24]. In
men with COPD, BMI values within the normal
range (22–25 kg/m2) may already suffice to increase
the risk of osteoporosis by comparison with the
overweight (BMI > 25.1 kg/m2), the former probably
being more sensitive to the effect of weight load on
bone, despite their normal nutritional status. A
BMI 5 25 kg/m2 in a patient with COPD should
alert the clinician to the possibility of osteoporosis.
In the present study the severity of bronchial
obstruction expressed by FEV1 resulted linearly
associated with BMD values, although the risk of
osteoporosis proved independent of the dichotomised severity of bronchial obstruction. This apparent discrepancy may be due partly to the fact that
continuous variables were treated as categorical
variables, resulting in the loss of some information.
Actually, the severity of lung disease was found
inversely correlated with BMD in several previous
studies on the general population. The clinical
distinction between moderate and severe lung
disease, anyway, appears to be useless in distinguishing between patients with COPD with and without a
low bone density.
Unlike BMI and FEV1%, sarcopenia no longer
correlated significantly with femoral BMD after
adjusting for BMI and the other investigated
variables. This is probably partly due to the strength
of the BMI variable, which also includes muscle
mass. In fact, BMI expresses nutritional status and
both adipose and muscle mass deficiencies, whereas
the parameter used for sarcopenia (ASMM) only
considers limb muscle mass, not total muscle mass.
Further studies are needed here, using different
indicators of sarcopenia, such as strength and muscle
function.
Albumin was significantly lower in patients with
COPD than in controls and significantly associated
with BMD, even in multiple regression for lumbar
and neck of hip BMD. The lower mean albumin
values may be due to malnutrition and/or chronic
inflammation. However, conflicting results have been
reported on the relationship between serum albumin
BMI and BMD in elderly COPD
and BMD. In our earlier study, underweight
hypoalbuminemic subjects had a lower T-score than
underweight cases with normal serum albumin levels
[25]. Two large cross-sectional studies, nevertheless,
failed to confirm this correlation between albumin
and BMD [26,27].
The present study has some shortcomings. The
first is the lack of specific markers of inflammation, as
already discussed above. The second is the absence
of women in the study: this is due to the limited
number of elderly women among the outpatients
attending the Respiratory Pathophysiology Department in Padua for routine check-ups during the time
of the study. Another limit could be the restricted
number of patients due to severe inclusion criteria.
More general selection criteria would bring in a
number of factors very likely to interfere with the
relationships between BMD and the variables studied, and adjusting these factors in the analysis would
demand a much larger sample size.
In conclusion, our findings suggest that BMI
expresses the relationship between nutritional status
and BMD in elderly COPD males better than other
nutritional indices, and that age-related sarcopenia
seems not involved in bone mass loss. Severity of
bronchial obstruction seems associated to BMD even
if not related to a higher risk of osteoporosis, while
BMI values 5 25 kg/m2, though still within the
normal range for younger adults, carry a higher risk
of osteoporosis in elderly men with COPD.
Declaration of interest: The authors report no
conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
1. Ionescu AA, Schoon E. Osteoporosis in chronic obstructive
pulmonary disease. Eur Respir J 2003;22:64S–75S.
2. Ilich JZ, Brownbill RA, Tamborlini L. Bone and nutrition in
elderly women: protein, energy, and calcium as main
determinants of bone mineral density. Eur J Clin Nutr
1003;57:554–565.
3. Sin DD, Man JP, Man SFP. The risk of osteoporosis in
Caucasian men and women with obstructive airway disease. J
Med 2003;114:10–14.
4. De Vries F, Van Staa TP, Bracke MSGM, et al. Severity of
obstructive airway disease and risk of osteoporotic fracture.
Eur R J 2005;25:879–884.
5. Cochrane WJ, Afolabi OA. Investigation into the nutritional
status, dietary intake and smoking habits of patients with
chronic obstructive pulmonary disease. J Hum Nutr Diet
2004;17:3–11.
6. Sergi G, Coin A, Marin S, et al. Body composition and resting
energy expenditure in elderly male patients with chronic
obstructive pulmonary disease. Respir Med 2006;100:1918–
1924.
7. Walsh MC, Hunter GR, Livingstone MB. Sarcopenia in
premenopausal and postmenopausal women with osteopenia,
osteoporosis and normal bone mineral density. Osteoporos Int
2006;17:61–67.
147
8. Felson DT, Zhang Y, Hannan MT, Anderson JJ. Effects of
weight and body mass index on bone mineral density in men
and women: the Framingham study. J Bone Miner Res
1993;8:567–573.
9. Coin A, Perissinotto E, Enzi G, et al. Predictors of low bone
mineral density in the elderly: the role of dietary intake,
nutritional status and sarcopenia. Eur J Clin Nutr 2008;62:
802–809.
10. Siafakas NM, Vermeire P, Pride NB, Paoletti P, Gibson J,
et al. Optimal assessment and management of chronic
obstructive pulmonary disease (COPD). ERS consensus
statement. Eur Respir J 1995;8:1398–1420.
11. Rosow I, Braslau N. A Guttman health scale for the aged. J
Gerontol 1966;21:556–559.
12. Nagi SZ. An epidemiology of disability among adults in the
United States. Milbank Mem Fund Q 1976;54:439–468.
13. WHO (1994). Study group on assessment of fracture risk and
its application to screening and postmenopausal oseteoporosis. Publication No. 843, Geneva: World Health Organisation.
14. Heymsfield SB, Smith R, Aulet M, Bensen B, Lichtman S, et al.
Appendicular skeletal muscle mass: measurement by dualphoton absorptiometry. Am J Clin Nutr 1990;52:214–218.
15. Baumgartner RN, Koehler KM, Gallagher D, Romero L,
Heymsfield SB, et al. Epidemiology of sarcopenia among
the elderly in New Mexico. Am J Epidemiol 1998;147:755–
763.
16. GOLD (Global initiative for chronic Obstructive Lung
Disease). Global strategy for diagnosis, management and
prevention of chronic obstructive pulmonary disease. 2008
Medical Communications Resources, Inc. Pages 3–4.
17. Schols AM, Slangen J, Volovics L, Wouters EF. Weight loss is
a reversible factor in the prognosis of chronic obstructive
pulmonary disease. Am J Respir Crit Care Med 1998;157:
1791–1797.
18. Jagoe RT, Engelen MP. Muscle wasting and changes in
muscle protein metabolism in chronic obstructive pulmonary
disease. Eur Respir J Suppl 2003;46:52s–63s.
19. Dimai HP, Domej W, Leb G, Lau KH. Bone loss in patients
with untreated chronic obstructive pulmonary disease is
mediated by an increase in bone resorption associated with
hypercapnia. J Bone Mineral Res 2001;16:2132–2141.
20. Fujimoto H. Hypoxemia is a risk factor for bone mass loss. J
Bone Miner Metab 1999;17:211–216.
21. Kudo O, Sabokbar A, Pocock A, Itonaga I, Fujicawa Y, et al.
Interleukin-6 and interleukin-11 support human osteoclast
formation by a RANKL-independent mechanism. Bone
2003;32:1–7.
22. Glynn NW, Meilahn EN, Charron M, Anderson SJ, Kuller
LH, et al. Determinants of bone mineral density in older men.
J Bone Miner Res 1995;10:1769–1777.
23. Murphy S, Khaw KT, Cassidy A, Compston JE. Sex
hormones and bone mineral density in elderly men. Bone
Miner 1993;20:133–140.
24. Sergi G, Perissinotto E, Pisent C, Buja A, Maggi S, et al.
(ILSA Working Group). An adequate threshold for body mass
index to detect underweight condition in elderly persons: the
Italian Longitudinal Study on Aging (ILSA). J Gerontol A
Biol Sci Med Sci 2005;60:866–871.
25. Coin A, Sergi G, Benincà P, Lupoli L, Cinti G, et al. Bone
mineral density and body composition in underweight and
normal elderly subjects. Osteoporos Int 2000;11:1043–1050.
26. Lunde AV, Barrett-Connor E, Morton DJ. Serum albumin
and bone mineral density in healthy older men and women:
the Rancho Bernardo Study. Osteoporos Int 1998;8:547–551.
27. D’Erasmo E, Pisani D, Ragno A, Raejntroph N, Letizia C,
et al. Relationship between serum albumin and bone mineral
density in postmenopausal women and in patients with
hypoalbuminemia. Horm Metab Res 1999;31:385–388.