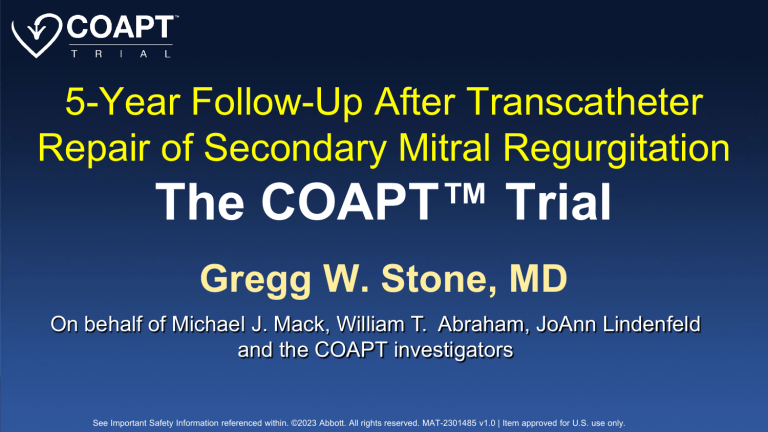
5-Year Follow-Up After Transcatheter Repair of Secondary Mitral Regurgitation The COAPT™ Trial Gregg W. Stone, MD On behalf of Michael J. Mack, William T. Abraham, JoAnn Lindenfeld and the COAPT investigators See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. The COAPT™ Trial Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation A parallel-controlled, open-label, multicenter trial in 614 patients with heart failure and moderate-to-severe (3+) or severe (4+) secondary MR who remained symptomatic despite maximally-tolerated GDMT Randomize 1:1* MitraClip + GDMT N=302 GDMT alone N=312 *Stratified by cardiomyopathy etiology (ischemic vs. non-ischemic) and site Stone GW et al. N Engl J Med. 2018;379:2307-18 See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Background • In the COAPT trial, treatment of symptomatic patients with heart failure (HF) and severe secondary MR with the MitraClip safely improved survival through 24 months, reduced HF hospitalizations (HFH), and improved qualityof-life compared with maximally-tolerated guidelinedirected medical therapy (GDMT) alone • Per protocol, subjects randomized to GDMT were not allowed to “crossover” to the MitraClip prior to 24 months, but were permitted to do so after 24 months See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Objectives The present study sought to: 1) Describe the final 5-year clinical outcomes of patients enrolled in the COAPT trial 2) Analyze the impact of MitraClip treatment in patients assigned to GDMT alone See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Key Inclusion Criteria 1. Moderate-to-severe (3+) or severe (4+) secondary MR confirmed by an echo core laboratory (US ASE criteria) 2. LVEF 20%-50% and LVESD ≤70 mm 3. NYHA class II-IVa despite a stable maximally-tolerated GDMT regimen and CRT (if appropriate) per societal guidelines 4. HFH within 12 months and/or weight-adjusted BNP ≥300 pg/ml* or NT-proBNP ≥1500 pg/ml* See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Key Exclusion Criteria 1. ACC/AHA stage D HF, hemodynamic instability or shock 2. CAD requiring revascularization 3. COPD requiring continuous home O2 or chronic oral steroid use 4. Severe PHTN or mod/sev RV dysfunction 5. AV or TV disease requiring surgery or transcatheter intervention 6. MV orifice area <4.0 cm2 by site-assessed TTE See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. N=614 at 78 sites in the US and Canada MitraClip + GDMT N=302 N=293 N=9 Randomized Initial treatment MitraClip GDMT alone Withdrew 4 1 Lost to follow-up N=297/302 (98.3%) 30-day follow-up 1-year follow-up 2-year follow-up 3-year follow-up N=269/312 (86.2%) Withdrew 3 1 Lost to follow-up 4-year follow-up Withdrew 4 1 Lost to follow-up N=270/302 (89.4%) N=277/312 (88.8%) Withdrew 7 1 Lost to follow-up Withdrew 6 1 Lost to follow-up N=275/302 (91.1%) N=291/312 (93.3%) Withdrew 11 3 Lost to follow-up Withdrew 3 1 Lost to follow-up N=282/302 (93.4%) N=307/312 (98.4%) Withdrew 16 0 Lost to follow-up Withdrew 5 3 Lost to follow-up N=286/302 (94.7%) N=1 N=311 Withdrew 5 0 Lost to follow-up Withdrew 3 0 Lost to follow-up N=294/302 (97.4%) GDMT alone N=312 N=265/312 (84.9%) Withdrew 1 0 Lost to follow-up 5-year follow-up N=264/312 (84.6%) See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Baseline Characteristics (i) MitraClip + GDMT (N=302) GDMT alone (N=312) MitraClip + GDMT (N=302) GDMT alone (N=312) 71.7 ± 11.8 72.8 ± 10.5 BMI (kg/m2) 27.0 ± 5.8 27.1 ± 5.9 Male 66.6% 61.5% CrCl (ml/min) 50.9 ± 28.5 47.8 ± 25.0 Diabetes 35.1% 39.4% - ≤60 ml/min 71.6% 75.2% Hypertension 80.5% 80.4% Anemia (WHO) 59.8% 62.7% Hyperchol. 55.0% 52.2% BNP (pg/mL) 1015 ± 1086 1017 ± 1219 Prior MI 51.7% 51.3% NT-proBNP (pg/mL) 5174 ± 6567 5944 ± 8438 Prior PCI 43.0% 49.0% STS replacement sc 7.8 ± 5.5 8.5 ± 6.2 Prior CABG 40.1% 40.4% 41.7% 43.6% Prior stroke or TIA 18.5% 15.7% PVD 17.2% 18.3% - High* 68.6% 69.9% COPD 23.5% 23.1% - Not-high 31.4% 30.1% H/o atrial fibr 57.3% 53.2% Age (years) - ≥8 Surgical risk (central eligibility committee) * STS repl score ≥8% or one or more factors present predicting extremely high surgical risk See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Baseline Characteristics (ii) HF parameters MitraClip + GDMT (N=302) GDMT alone (N=312) Etiology of HF Echo core lab MitraClip + GDMT (N=302) GDMT alone (N=312) MR severity - Ischemic 60.9% 60.6% - Mod-to-sev (3+) 49.0% 55.3% - Non-ischemic 39.1% 39.4% - Severe (4+) 51.0% 44.7% EROA, cm2 0.41 ± 0.15 0.40 ± 0.15 NYHA class -I 0.3% 0% LVESD, cm 5.3 ± 0.9 5.3 ± 0.9 - II 42.7% 35.4% LVEDD, cm 6.2 ± 0.7 6.2 ± 0.8 - III 51.0% 54.0% LVESV, mL 135.5 ± 56.1 134.3 ± 60.3 - IV 6.0% 10.6% LVEDV, mL 194.4 ± 69.2 191.0 ± 72.9 HF hosp w/i 1 year 58.3% 56.1% LVEF, % 31.3 ± 9.1 31.3 ± 9.6 Prior CRT 38.1% 34.9% - ≤40% 82.2% 82.0% Prior defibrillator 30.1% 32.4% 44.0 ± 13.4 44.6 ± 14.0 RVSP, mmHg See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Primary Effectiveness: All Heart Failure Hospitalizations Through 5-Year Follow-up Cumulative HF Hospitalizations (n) 500 MitraClip + GDMT GDMT alone 450 400 350 300 HR [95% CI] = 0.51 [0.39, 0.66] 250 200 150 100 50 0 0 6 18 24 30 36 42 48 54 60 124 79 Time After Randomization (Months) No. at Risk: MitraClip 12 302 269 238 219 205 186 167 151 138 GDMT 312 272 224 188 156 120 94 84 59 133 106 See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Analyzed using a joint frailty model to account for correlated events and the competing risk of death Primary Effectiveness: All Heart Failure Hospitalizations Through 5-Year Follow-up Cumulative HF Hospitalizations (n) 500 MitraClip + GDMT GDMT alone 450 400 447 in 208 pts 350 314 300 in 151 pts 250 200 33.1%/yr in the device group vs. 57.2%/yr in the control group HR [95% CI] = 0.53 [0.41-0.68] 150 100 50 0 0 6 18 24 30 36 42 48 54 60 124 79 Time After Randomization (Months) No. at Risk: MitraClip 12 302 269 238 219 205 186 167 151 138 GDMT 312 272 224 188 156 120 94 84 59 133 106 See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Analyzed using a joint frailty model to account for correlated events and the competing risk of death Primary Safety: Outcomes Through 5 Years MitraClip implant attempts (n=293) 30 Days 12 Months All safety events 4 (1.4) 9 (3.3) Device-specific events 4 (1.4) 4 (1.4) - SLDA 2 (0.7) 2 (0.7) - Device embolization 1 (0.3) 1 (0.3) - Endocarditis requiring surgery 0 (0.0) 0 (0.0) - Mitral stenosis* requiring surgery 0 (0.0) 0 (0.0) - Any device-related complication requiring non-elective CV surgery 1 (0.3) 1 (0.3) 0 (0.0) 5 (2.0) - LVAD 0 (0.0) 3 (1.2) - Heart transplantation 0 (0.0) 2 (0.8) Progressive HF unrelated to device complications 24 Months 36 Months 48 Months 60 Months Primary safety endpoint SLDA = single leaflet device attachment. LVAD = left ventricular assist device. *Mitral valve area <1.5 cm2 by echo core laboratory measurement. See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Primary Safety: Outcomes Through 5 Years MitraClip implant attempts (n=293) 30 Days 12 Months 24 Months 36 Months 48 Months 60 Months All safety events 4 (1.4) 9 (3.3) 13 (5.2) 20 (8.8) 22 (10.1) 23 (10.8) Device-specific events 4 (1.4) 4 (1.4) 4 (1.4) 4 (1.4) 4 (1.4) 4 (1.4) - SLDA 2 (0.7) 2 (0.7) 2 (0.7) 2 (0.7) 2 (0.7) 2 (0.7) - Device embolization 1 (0.3) 1 (0.3) 1 (0.3) 1 (0.3) 1 (0.3) 1 (0.3) - Endocarditis requiring surgery 0 (0.0) 0 (0.0) 0 (0.0) 0 (0.0) 0 (0.0) 0 (0.0) - Mitral stenosis* requiring surgery 0 (0.0) 0 (0.0) 0 (0.0) 0 (0.0) 0 (0.0) 0 (0.0) - Any device-related complication requiring non-elective CV surgery 1 (0.3) 1 (0.3) 1 (0.3) 1 (0.3) 1 (0.3) 1 (0.3) 0 (0.0) 5 (2.0) 9 (3.8) 16 (7.5) 18 (8.8) 19 (9.5) - LVAD 0 (0.0) 3 (1.2) 6 (2.6) 11 (5.1) 12 (5.8) 13 (6.5) - Heart transplantation 0 (0.0) 2 (0.8) 3 (1.3) 7 (3.4) 9 (4.7) 9 (4.7) Progressive HF unrelated to device complications SLDA = single leaflet device attachment. LVAD = left ventricular assist device. *Mitral valve area <1.5 cm2 by echo core laboratory measurement. See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Death or HF Hospitalization Death or HFH (%) 100% MitraClip + GDMT GDMT alone 80% 91.5% 73.6% 60% 40% HR [95% CI] = 0.53 [0.44-0.64] 20% 0% 0 6 12 18 24 30 36 42 48 54 60 Time After Randomization (Months) No. at Risk: MitraClip 302 236 194 174 158 141 118 105 93 81 52 GDMT 312 206 157 122 95 58 43 37 33 26 17 See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. 5-Year Death or HFH Subgroup analysis See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. First Heart Failure Hospitalization First Heart Failure Hospitalization (%) 100% MitraClip + GDMT GDMT alone 80% 83.0% 61.0% 60% 40% HR [95% CI] = 0.49 [0.40-0.61] 20% 0% 0 6 12 18 24 30 36 42 48 54 60 Time After Randomization (Months) No. at Risk: MitraClip 302 236 194 174 158 141 118 105 93 81 52 GDMT 312 206 157 122 95 58 43 37 33 26 17 See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. First Heart Failure Hospitalization First Heart Failure Hospitalization (%) 100% MitraClip + GDMT GDMT alone 80% 76.4% 60% 46.8% 40% 34.3% 30.7% HR [95% CI] = 0.46 [0.36–0.57] 20% 0% HR [95% CI] = 0.85 [0.55–1.33] 0 6 12 18 24 30 36 42 48 54 60 Time After Randomization (Months) No. at Risk: MitraClip 302 194 158 167 119 63 GDMT 312 157 95 119 82 43 See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. All-cause Mortality All-cause Mortality (%) 100% MitraClip + GDMT GDMT alone 80% 67.2% 60% 57.3% 40% HR [95% CI] = 0.72 [0.58-0.89] 20% 0% 0 6 12 18 24 30 36 42 48 54 60 Time After Randomization (Months) No. at Risk: MitraClip 302 269 238 219 205 186 167 151 138 124 79 GDMT 312 272 224 189 157 135 122 107 94 84 59 See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. All-cause Mortality All-cause Mortality (%) 100% MitraClip + GDMT GDMT alone 80% HR [95% CI] = 0.62 [0.47–0.82] 60% HR [95% CI] = 0.88 [0.64–1.23] 42.8% 40.6% 42.7% 40% 28.1% 20% 0% 0 6 12 18 24 30 36 42 48 54 60 Time After Randomization (Months) No. at Risk: MitraClip 302 238 205 167 138 79 GDMT 312 224 157 122 94 59 See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Crossover Treatment in the Control Arm Randomized to GDMT alone (N = 312) Not eligible for crossover at 2 years (N = 169) Death: 124 LVAD: 16 Transplant: 9 Withdrawals: 26 Lost to follow-up: 3 Other: 2 No MitraClip treatment (N = 76) No MitraClip treatment before 2 years (N = 138) MitraClip treatment before 2 years (N = 5) MitraClip treatment after 2 years* (N = 62 of 138; 44.9%) Total crossovers (N = 67 of 312; 21.5%) See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Death or HFH After Crossovers Death or HFH (%) 100% MitraClip + GDMT GDMT alone without MitraClip GDMT alone after MitraClip 80% 60% 40% Multivariable analysis in GDMT alone group Adjusted HR [95% CI] after MitraClip = 0.53 [0.36, 0.78] 20% 0% 0 6 12 18 24 30 36 42 48 54 60 Time After Randomization (Months) No. at Risk: MitraClip 302 236 194 158 118 93 52 GDMT without MitraClip 312 205 156 93 40 32 16 GDMT after MitraClip 67 56 42 30 9 See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. For crossover patients, follow-up duration is from the crossover procedure date NYHA Class Throughout Follow-up I II III IV Died 100% NYHA class (%) 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Device Control Device Control Device Control Device Control Device Control Device Control Device Control Device Control Device Control (n=302) (n=311) (n=291) (n=288) (n=286) (n=278) (n=278) (n=266) (n=270) (n=258) (n=260) (n=263) (n=263) (n=255) (n=266) (n=247) (n=257) (n=249) Baseline Class I or II Diff (95% CI) 43.0% 35.4% 7.7% [-0.1, 15.3] 30 days 74.2% 46.5% 6 months 66.4% 47.1% 1 year 61.5% 43.2% 27.7% [19.9, 35.1] 19.3% [11.2, 27.1] 18.3% [9.9, 26.3] 18 months 56.7% 39.5% 17.1% [8.6, 25.3] 2 years 47.3% 37.8% 16.5% [8.2, 24.5] 3 years 42.2% 25.1% 17.1% [9.0, 24.9] 4 years 34.2% 18.6% 15.6% [8.0, 22.9] See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. 5 years 24.1% 15.7% 8.5% [1.5, 15.3] MR Severity (Core Lab) None 1+ 2+ 3+ 4+ 100% 90% MR grade (%) 80% 70% 60% 50% 40% 30% 20% 10% 0% Device Control Device Control Device Control Device Control Device Control Device Control Device (n=302) (n=311) (n=273) (n=257) (n=240) (n=218) (n=210) (n=175) (n=177) (n=141) (n=167) (n=126) (n=120) Baseline MR ≤2+ Diff (95% CI) 0% 0% - 30 days 92.7% 34.2% 6 months 93.8% 38.1% 1 year 94.8% 46.9% 18 months 94.9% 45.4% 2 years 99.4% 46.8% Control (n=74) 3 years 98.3% 85.1% Device (n=80) Control (n=49) 4 years 97.5% 79.6% 58.4% [51.4, 64.5] 55.7% [48.1, 62.3] 47.9% [39.6, 55.5] 49.5% [40.2, 57.9] 52.6% [43.5, 61.1] 13.2% [5.9, 23.1] 17.9% [7.1, 31.3] See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Device (n=57) Control (n=46) 5 years 94.7% 91.3% 3.4% [-7.1, 15.6] Limitations • Device treatment was unblinded, and withdrawals during follow-up were more frequent in the control group. All-cause death, the endpoint least prone to bias, was reduced, and the results were consistent after multiple imputation to account for missing data. • The present results reflect treatment with the first generation MitraClip. MitraClip NTR/XTR and G4 may be more effective at reducing MR to ≤1+, and outcomes with other mitral TEER and non-TEER systems are unknown. • Angiotensin receptor-neprilysin inhibitors were used in < one-third of pts, and only 3 pts were treated with SGLT2 inhibitors (all during the last year of FU). More frequent use of these agents may have decreased the pool of pts eligible for enrollment but would likely not have decreased the effects of TEER. • Whether correction of MR would safely improve outcomes in more or less critically ill pts or in those with moderate MR is unknown. See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Conclusions and Implications (1) • In pts with heart failure and severe secondary MR who remained symptomatic despite optimal medical therapy, TEER with the MitraClip was safe, reduced the rate of HFHs and improved survival during 5-year follow-up. • These outcomes were consistent across all pre-specified subgroups, regardless of patient age, sex, MR severity, left ventricular function and volume, cardiomyopathy etiology, and surgical risk. • Symptomatic status (NYHA class) was also improved throughout 5-year follow-up, and MitraClip treatment provided durable repair of mitral regurgitation. See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Conclusions and Implications (2) • Treatment effects were reduced after 2-3 years, in large part due to MitraClip treatment in 44.9% of control group pts surviving to 2 years. • The prognosis of control group pts so treated was substantially improved, similar to that of pts originally assigned to MitraClip treatment. • However, nearly half of control group pts had died before becoming eligible for crossover at 2 years. • Heart failure patients appropriate for TEER with the MitraClip should therefore be identified and considered for treatment as early as possible. See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Conclusions and Implications (3) • Finally, despite the favorable risk:benefit profile of the MitraClip in this setting, adverse outcomes continued to accrue in both groups such that 91.5% of control group pts and 73.6% of device group pts had either died or been hospitalized for heart failure within 5 years. • These findings emphasize the need for further therapies to address the underlying left ventricular dysfunction in this high-risk population. See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. See Important Safety Information referenced within. ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only. Rx Only Important Safety Information MITRACLIP™ CLIP DELIVERY SYSTEM Indications for Use • The MitraClipTM G4 System is indicated for the percutaneous reduction of significant symptomatic mitral regurgitation (MR ≥ 3+) due to primary abnormality of the mitral apparatus [degenerative MR] in patients who have been determined to be at prohibitive risk for mitral valve surgery by a heart team, which includes a cardiac surgeon experienced in mitral valve surgery and a cardiologist experienced in mitral valve disease, and in whom existing comorbidities would not preclude the expected benefit from reduction of the mitral regurgitation. • The MitraClipTM G4 System, when used with maximally tolerated guideline-directed medical therapy (GDMT), is indicated for the treatment of symptomatic, moderate-to-severe or severe secondary (or functional) mitral regurgitation (MR; MR ≥ Grade III per American Society of Echocardiography criteria) in patients with a left ventricular ejection fraction (LVEF) ≥ 20% and ≤ 50%, and a left ventricular end systolic dimension (LVESD) ≤ 70 mm whose symptoms and MR severity persist despite maximally tolerated GDMT as determined by a multidisciplinary heart team experienced in the evaluation and treatment of heart failure and mitral valve disease. Label Contraindications The MitraClip G4 System is contraindicated in patients with the following conditions: Patients who cannot tolerate, including allergy or hypersensitivity to, procedural anticoagulation or post procedural anti-platelet regime; Patients with known hypersensitivity to clip components (nickel / titanium, cobalt, chromium, polyester), or with contrast sensitivity; Active endocarditis of the mitral valve; Rheumatic mitral valve disease; Evidence of intracardiac, inferior vena cava (IVC) or femoral venous thrombus Potential Complications and Adverse Events The following ANTICIPATED EVENTS have been identified as possible complications of the MitraClip G4 procedure: Allergic reactions or hypersensitivity to latex, contrast agent, anaesthesia, device materials (nickel / titanium, cobalt, chromium, polyester), and drug reactions to anticoagulation, or antiplatelet drugs, Vascular access complications which may require transfusion or vessel repair including: wound dehiscence, catheter site reactions, Bleeding (including ecchymosis, oozing, hematoma, hemorrhage, retroperitoneal hemorrhage), Arteriovenous fistula, pseudoaneurysm, aneurysm, dissection, perforation / rupture, vascular occlusion, Emboli (air thrombotic material, implant, device component); Peripheral Nerve Injury; Lymphatic complications; Pericardial complications which may require additional intervention, including: Pericardial effuse on, Cardiac tamponade, Pericarditis; Cardiac complications which may require additional interventions or emergency cardiac surgery, including: Cardiac perforation, Atrial septal defect; Mitral valve complications, which may complicate or prevent later surgical repair, including: Chordal entanglement / rupture, Single Leaflet Device Attachment (SLDA), Thrombosis, Dislodgement of previously implanted devices, Tissue damage, Mitral valve stenosis, Persistent or residual mitral regurgitation, Endocarditis; Cardiac arrhythmias (including conduction disorders, atrial arrhythmias, ventricular arrhythmias); Cardiac ischemic conditions (including myocardial infarction, myocardial ischemia, and unstable / stable angina); Venous thromboembolism (including deep vein thrombosis, pulmonary embolism, post procedure pulmonary embolism); Stroke / Cerebrovascular accident (CVA) and Transient Ischemic Attack (TIA); System organ failure: Cardio-respiratory arrest, Worsening heart failure, Pulmonary congestion, Respiratory dysfunction / failure / atelectasis, Renal insufficiency or failure, Shock (including cardiogenic and anaphylactic); Blood cell disorders (including coagulopathy, hemolysis, and Heparin Induced Thrombocytopenia (HIT)); Hypotension / hypertension; Infection including: Urinary Tract Infection (UTI), Pneumonia, Septicemia; Nausea / vomiting; Chest pain; Dyspnea; Edema; Fever or hyperthermia; Pain; Death; Fluoroscopy, Transesophageal echocardiogram (TEE) and Transthoracic echocardiogram (TTE) -related complications: Skin injury or tissue changes due to exposure to ionizing radiation, Esophageal irritation; Esophageal perforation, Gastrointestinal bleeding Source: ACC 2023 See Important Safety Information referenced within. CAUTION: This product is intended for use by or under the direction of a physician. Prior to use, reference the Instructions for Use, inside the product carton (when available) or at eifu.abbottvascular.com or at medical.abbott/manuals for more detailed information on Indications, Contraindications, Warnings, Precautions and Adverse Events. Illustrations are artist’s representations only and should not be considered as engineering drawings or photographs. Abbott 3200 Lakeside Dr., Santa Clara, CA. 95054 USA, Tel: 1.800.277.9902 TM Indicates a trademark of the Abbott Group of Companies www.structuralheart.Abbott ©2023 Abbott. All rights reserved. MAT-2301485 v1.0 | Item approved for U.S. use only.