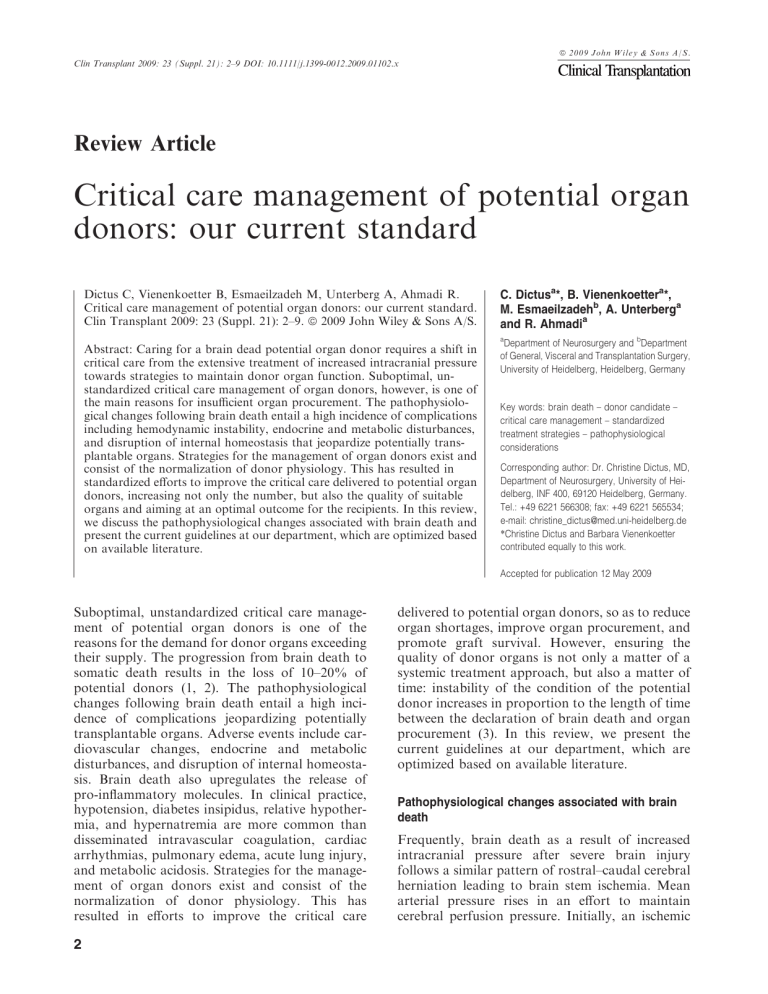
ª 2009 John Wiley & Sons A/S. Clin Transplant 2009: 23 (Suppl. 21): 2–9 DOI: 10.1111/j.1399-0012.2009.01102.x Review Article Critical care management of potential organ donors: our current standard Dictus C, Vienenkoetter B, Esmaeilzadeh M, Unterberg A, Ahmadi R. Critical care management of potential organ donors: our current standard. Clin Transplant 2009: 23 (Suppl. 21): 2–9. ª 2009 John Wiley & Sons A/S. C. Dictusa*, B. Vienenkoettera*, M. Esmaeilzadehb, A. Unterberga and R. Ahmadia a Abstract: Caring for a brain dead potential organ donor requires a shift in critical care from the extensive treatment of increased intracranial pressure towards strategies to maintain donor organ function. Suboptimal, unstandardized critical care management of organ donors, however, is one of the main reasons for insufficient organ procurement. The pathophysiological changes following brain death entail a high incidence of complications including hemodynamic instability, endocrine and metabolic disturbances, and disruption of internal homeostasis that jeopardize potentially transplantable organs. Strategies for the management of organ donors exist and consist of the normalization of donor physiology. This has resulted in standardized efforts to improve the critical care delivered to potential organ donors, increasing not only the number, but also the quality of suitable organs and aiming at an optimal outcome for the recipients. In this review, we discuss the pathophysiological changes associated with brain death and present the current guidelines at our department, which are optimized based on available literature. Department of Neurosurgery and bDepartment of General, Visceral and Transplantation Surgery, University of Heidelberg, Heidelberg, Germany Key words: brain death – donor candidate – critical care management – standardized treatment strategies – pathophysiological considerations Corresponding author: Dr. Christine Dictus, MD, Department of Neurosurgery, University of Heidelberg, INF 400, 69120 Heidelberg, Germany. Tel.: +49 6221 566308; fax: +49 6221 565534; e-mail: christine_dictus@med.uni-heidelberg.de *Christine Dictus and Barbara Vienenkoetter contributed equally to this work. Accepted for publication 12 May 2009 Suboptimal, unstandardized critical care management of potential organ donors is one of the reasons for the demand for donor organs exceeding their supply. The progression from brain death to somatic death results in the loss of 10–20% of potential donors (1, 2). The pathophysiological changes following brain death entail a high incidence of complications jeopardizing potentially transplantable organs. Adverse events include cardiovascular changes, endocrine and metabolic disturbances, and disruption of internal homeostasis. Brain death also upregulates the release of pro-inflammatory molecules. In clinical practice, hypotension, diabetes insipidus, relative hypothermia, and hypernatremia are more common than disseminated intravascular coagulation, cardiac arrhythmias, pulmonary edema, acute lung injury, and metabolic acidosis. Strategies for the management of organ donors exist and consist of the normalization of donor physiology. This has resulted in efforts to improve the critical care 2 delivered to potential organ donors, so as to reduce organ shortages, improve organ procurement, and promote graft survival. However, ensuring the quality of donor organs is not only a matter of a systemic treatment approach, but also a matter of time: instability of the condition of the potential donor increases in proportion to the length of time between the declaration of brain death and organ procurement (3). In this review, we present the current guidelines at our department, which are optimized based on available literature. Pathophysiological changes associated with brain death Frequently, brain death as a result of increased intracranial pressure after severe brain injury follows a similar pattern of rostral–caudal cerebral herniation leading to brain stem ischemia. Mean arterial pressure rises in an effort to maintain cerebral perfusion pressure. Initially, an ischemic Critical care management of potential organ donors mesencephalon results in parasympathetic activation clinically manifest with sinus bradycardia and hypotension. Subsequent pontine ischemia leads to sympathetic stimulation with superimposed hypertension (CushingÕs reflex) (4, 5). This is followed by the ‘‘autonomic storm’’, a phase of intensive sympathetic activity with massive catecholamine release, which is because of ischemia of the vagal cardiomotor nucleus in the medulla oblongata (6, 7), dramatically increasing myocardial work (8), and jeopardizing end organ blood flow. Finally, spinal cord sympathetic deactivation results in the loss of vasomotor tone with subsequent vasodilatation and impaired cardiac output. Together with vasopressin deficiency as a result of pituitary gland ischemia and subsequent diabetes insipidus, only a minority of potential organ donors are able to maintain hemodynamic stability without intensified critical care therapy (9–12). However, potential donor organs are endangered not only by ischemic damage, but also by reperfusion injury when the circulation is restored, leading to a generalized inflammatory response (13, 14). Damaged or necrotic brain tissue induces a release of plasminogen activator and thromboplastin with a risk of disseminated intravasal coagulopathy (15). Furthermore, loss of hypothalamic–pituitary function results in the loss of thermoregulation with subsequent hypothermia. Together with the massive release of catecholamines during the autonomic storm, this, in turn, can cause malfunction of platelets further deteriorating blood coagulation. A schematic overview of the pathophysiological changes associated with brain death is given in Fig. 1. Cardiovascular considerations Because of the pathophysiological changes described previously, hemodynamic instability is a major challenge in the treatment of brain dead potential organ donors. Hypertension is a rare event usually occurring during the phase of cerebral herniation itself and is therefore mostly self-limitating. In case of prolonged hypertension, short-acting substances such as urapidil, esmolol, or nitroprusside should be preferred (16). Hypotension, however, affects almost all patients after brain death (3, 17), and sustained hypotension may occur in 20 percent of donors, despite vasoactive-drug support (3). Because hypotension is associated with diminished blood and oxygen supply and, subsequently, with a decrease in donor organ function, it is essential to identify and treat putative causes. In severely brain-damaged patients, hypotension most frequently occurs because of hypovolemia related to traumatic blood loss, central diabetes insipidus, or osmotic therapy for increased intracranial pressure, but also because of the loss of sympathetic tone during cerebral herniation, giving rise to blunted vasomotor reflexes, vasodilatation, and impaired cardiac contractility. Therefore, a systematic approach is needed to achieve hemodynamic stability aiming at a mean arterial pressure (MAP) of ‡ 60 mmHg, a central venous pressure (CVP) of 6–10 mmHg, a urinary output of ‡ 1 mL/kg/h, and a left ventricular ejection fraction (LVEF) of ‡ 45% as advocated by the Crystal City Consensus Conference (18) and the United Network for Organ Sharing (UNOS). Baseline monitoring therefore should include arterial and central venous catheterization, complemented by repeated echocardiography if heart donation is considered. The initial treatment step consists in aggressive fluid replacement, which is usually performed with cristalloids such as lactated RingerÕs solution, normal (0.9%), or half normal (0.45%) saline solutions. In view of recent studies, hydroxyethyl starch can also be safely applied with respect to renal graft function to keep intravascular volume and colloid oncotic pressure within physiological ranges (19). Besides, in potential lung donors where a minimally positive fluid balance is associated with higher rates of lung procurement (20), colloid solutions are suitable to minimize the accumulation of pulmonary edema (21). In contrast, maintenance of kidney graft function requires aggressive volume replacement. Blood transfusion should be considered if the hemoglobin concentration is below 10 g/dL, or the hematocrit is below 30% (4, 18). If thresholds of hemodynamic stability are not achieved despite fluid resuscitation, extensive hemodynamic monitoring such as pulmonary artery catheter, echocardiography, or new devices to measure cardiac output (Pulscontour Continous Cardiac Output, PiCCO, PULSION Medical Systems, Munich, Germany) should be applied (22–25) to assess right- and left-sided cardiac filling pressures, cardiac output, and systemic vascular resistance (SVR). Under these circumstances, the administration of vasoactive drugs is indicated. In the past, dopamine has been the catecholamine of choice in doses of £ 10 lg/kg/min, but more recent studies have failed to support its formerly attributed beneficial effect on renal or hepatosplanchnic circulation (26, 27). Whenever hemodynamic stabilization requires dopamine doses of more than 10 lg/kg/min, addition of another inotrope such as norepinephrine or epinephrine is 3 Dictus et al. Fig. 1. Pathophysiological changes associated with brain death. recommended. Besides, catecholamines appear to have distinct immunomodulatory effects that may reduce inflammatory processes associated with brain death (28–30). However, indication for inotropes should be carefully thought over because intensive application of b-agonists can impair graft function of donor hearts by downregulation of breceptors. In this context, there has been a shift in vasoactive-drug therapy from catecholamines to arginine–vasopressin, which is usually applied for the treatment of central diabetes insipidus because of its antidiuretic effect but which, because of its additional vasopressor function, has also demonstrated a significant catecholamine-sparing effect without impairment of graft function (31, 32), and its early use in potential organ donors has been recommended by the American College of Cardiology (26, 33). Administration of hydrocortisone at a dose of 10 mg/h has been shown to enhance vascular reactivity in critically ill patients (34) and therefore appears to be another feasible option to spare catecholamines. Arrhythmias, another hemodynamic challenge in potential organ donors, are mainly attributable to brain stem ischemia and the myocardial injury caused by the autonomic storm during cerebral herniation and are therefore highly resistant to antiarrhythmic treatment (3, 35, 36). Ventricular arrhythmias are best treated by lidocaine or amiodarone, supraventricular arrhythmias by ami- 4 odarone (23). In bradyarrhythmias, anticholinergic drugs such as atropine are not effective because of the vagal break down during brain herniation; rather, administration of isoproterenol or epinephrine is recommended (23). Pulmonal considerations Neurogenic pulmonary edema, pneumonia, and intense inflammatory responses make successful lung procurement in brain dead potential organ donors challenging (37, 38). Critical care management in case of lung donation is very complex because all components of the hemodynamic model are affected. In this case, the American College of Cardiology has recommended a systolic blood pressure of 90–140 mmHg, a CVP of 8–12 mmHg, or a pulmonary capillary wedge pressure of 12–14 mmHg (33, 39). Often, it is necessary to take into consideration the antagonistic competing organ interests related to fluid resuscitation. A minimal volume strategy limits the development of extravascular lung water following brain-death-associated permeability changes and preserves the crucial PaO2/FiO2 gradient of at least 300 mmHg (40, 41). Recommendations for the mechanical ventilation are a tidal volume of 10– 12 mL/kg and a positive end-expiratory pressure (PEEP) of 5 cm H2O as well as a static airway pressure of ‡ 30 cm H2O to achieve highest arterial Critical care management of potential organ donors corticosteroids and the use of colloids have also shown benefits in the management of lung donors. Previously, only ideal lungs were transplanted into ideal recipients, but by reason of the number of deaths among patients on the waiting list for lung transplants, this approach has been challenged. Multiple authors have reported that recipients outcomes with less-than-ideal or ‘‘marginal’’ lungs are equivalent to the outcomes with ideal lungs. In these studies, aggressive pulmonary management, including strict regulation of ventilatory settings, moderate use of PEEP, frequent suctioning, inhalation of albuterol, use of bronchoscopy, a minimally positive fluid balance, and use of antibiotics were the key components that enabled the transplantation of marginal lungs with successful outcomes (43, 44). Renal considerations Fig. 2. Standardized critical care management of potential organ donors in our center. MAP, mean arterial blood pressure; CVP, central venous pressure; LVEF, left ventricular ejection fraction; T3, triiodothyronine. oxygen pressure (PaO2) with lowest fraction of inspiratory oxygen (39). The two most correctable causes of hypoxemia that preclude recovery of lungs for transplantation are atelectasis and excessive fluid replacement. To prevent atelectasis, to remove secretions and foreign bodies, and to isolate potential pathogens, bronchoscopy should be performed in all donors. This also helps to choose the best antibiotic therapy in donor and recipient, which is of extreme importance because bronchopneumonia is one of the most common reasons for rejecting lungs (37, 42). High-dose Brain death provokes both immunological and non-immunological damage to the kidneys, which may increase the rate of delayed allograft function, the risk of acute and chronic rejection, and the incidence of renal allograft nephropathy, and may decrease recipient survival (14, 37, 39, 45–47). Recent literature reports a beneficial immunomodulatory effect of catecholamines on donor kidney function (40, 48). However, vasopressor therapy with high doses of dopamine (> 10 lg/kg/min) or norepinephrine may compromise organ perfusion because of their vasoconstrictive mechanism of action, thus increasing the incidence of acute tubular necrosis and allograft failure (23, 49). On the other hand, epinephrine has been reported to improve systemic hemodynamic function and to maintain renal perfusion (23, 50–52). Although there is no consensus on the specific combination of catecholamines, combination therapy has been associated with a reduction in the rates of acute rejection after renal transplantation and with improved graft survival (23, 49, 53–55). Arginine– vasopressin, that has been shown to reduce the need for vasoactive drugs in potential organ donors, does not seem to exert deleterious shortterm or long-term effects on renal graft function in the recipient (23) and therefore appears to be a suitable alternative if catecholamines are to be avoided. Furthermore, to ensure adequate renal perfusion, colloids such as hydroxyethyl starch may also be used in recommended dosages, referring to recent studies that failed to show any impairment in immediate renal graft recipients as it was formerly thought (19, 56). Because autoregulation of renal blood flow and glomerular filtration declines below a systolic blood pressure of 5 Dictus et al. 80–90 mmHg, timely hemodynamic stabilization of potential donors is important to maintain adequate organ perfusion and diuresis. If urine output remains < 1 mL/kg/h after optimized hemodynamic management, diuretics such as furosemide or mannitol are used. Nephrotoxic drugs should be avoided, and corticosteroids are recommended to diminish immunological damage (14, 37). In case an angiography is performed, it is recommended to use acetylcysteine and bicarbonate to prevent the development of contrast nephropathy (39, 57–62). Hepatic considerations The liver seems to tolerate long periods of hypoperfusion because of its large physiological reserve. Furthermore, the immunological response is weak as it is a tolerogenic organ. Nevertheless, the inflammatory processes related to brain death and reperfusion injury to the liver lead to poor initial function of liver allografts (37, 39, 63–66). Independently associated with an increased rate of recipient death and retransplantation are ABO incompatibility, high donor serum sodium concentration (> 155 mM), longer cold ischemia time as well as large platelet transfusions during surgery and prolonged recipient prothrombin time (37, 39, 64, 67, 68). Presumably, high donor serum sodium concentrations promote the accumulation of idiogenic osmoles within the liver cells, which, after having been transplanted into recipients with relatively normal sodium levels, promote intracellular water accumulation, cell lysis, and death. By all means, correcting the donor serum sodium level below 155 mM, keeping the CVP between 8 and 10 mmHg, using a low PEEP to prevent hepatic congestion and restoring liver glycogen stores with adequate nutrition decreases the incidence of liver allograft loss (37, 39, 69). Endocrinological considerations Dysfunction of the posterior pituitary gland with low to undetectable levels of vasopressin occurs in up to 90% of adult and pediatric organ donors (7, 12, 35, 36, 70) and commonly results in central diabetes insipidus clinically manifest with polyuria (urinary output > 300 mL/h), serum sodium concentration > 150 mM, urine sodium concentration < 20 mM, serum osmolarity > 310 mosM, urine osmolarity > 300 mosM, and a specific urinary weight of < 1005. Diabetes insipidus is essential to treat because it has been linked with hemodynamic instability in organ donors (11, 12). Adequate treatment consists of volume replacement, and half normal saline solution (0.45%) or 6 5% solution of dextrose in water should be preferred to decrease serum sodium levels (16, 23), because hypernatremia in organ donors has been associated with impaired graft function, especially after liver transplantation (69). Moreover, one has to be aware of other causes of polyuria such as previous osmotic therapy for increased intracranial pressure, hyperglycemia or diuretic agents. Compensation of arginine–vasopressin deficiency in brain dead organ donors by arginine–vasopressin or 1-desamino-8-d-arginine– vasopressin (DDAVP; desmopressin) alone or in combination is well accepted. Because of the combined vasopressor and antidiuretic effect of arginine–vasopressin, it is suitable for both hormone replacement therapy and restoration of hemodynamic stability; however, the use of arginine–vasopressin at doses greater than 0.04 U/min may cause coronary, renal, and splanchnic vasoconstriction jeopardizing donor organ function (71). Desmopressin has an advantageous pharmacological profile because it specifically acts on the V2-vasopressin receptors, therefore exerting predominantly antidiuretic effects, and has an extended duration of action (6–20 h) (41). Deficiency of hormones regulated by the anterior pituitary gland including T3 (triiodothyronine), T4 (thyroxine), thyroid stimulation hormone, adrenocorticotropic hormone, and human growth hormone has been described inconsistently (72). There are hints from a large retrospective analysis of the Organ Procurement and Transplantation Network OPTN/UNOS database, which showed a significant improvement in organ procurement and an increased odd of a brain dead patient becoming an organ donor if treated with a triple hormonal therapy consisting of methylprednisolone, T3/T4, and vasopressin (73). Various other studies have demonstrated beneficial effects of hormonal therapy on the hemodynamically unstable organ donor with subsequent improvement of graft function (25, 74, 75), altogether leading to the implementation of hormonal resuscitation of hemodynamically unstable potential organ donors (left ventricular ejection fraction < 45%) with a combination of T3 (4 lg bolus, infusion at 3 lg/h), vasopressin (1 U bolus, infusion at 0.5–4 U/h; SVR 800–1200), methylprednisolone (15 mg/kg bolus), and insulin (> 1 U/h; blood glucose levels 120–180 mg/dL) in the UNOS standardized donor management protocol (18). Severe brain injury results in a stressassociated rise in serum cortisol and may therefore produce relative adrenal insufficiency (35). Together with a decrease in serum cortisol levels after loss of anterior pituitary gland function and the inflammatory processes associated with brain Critical care management of potential organ donors death (29, 76–78), treatment with corticosteroids has been proven to be beneficial in potential organ donors both because of their immunomodulatory effects and their stabilization of systemic vascular resistance with catecholamine-sparing effects (34). The optimal dose, however, remains uncertain. Hyperglycemia is another common event after brain death and arises from massive catecholamine release, infusion of dextrose-containing fluids, and peripheral insulin resistance. Because hyperglycemic damage to pancreatic beta cells is linked with graft dysfunction in pancreatic transplants (16, 79), strict control of blood glucose levels by means of an insulin infusion is essential to achieve euglycemia (80–150 mg/dL) (23). Supportive critical care Hypothermia Loss of hypothalamic thermoregulation following cerebral herniation, peripheral vasodilatation because of the deactivation of sympathetic tone resulting in increased heat emission and reduction in metabolic activity lead to the inability of keeping body temperature within the physiological range (poikilothermia) and, most frequently, to hypothermia (80). Because hypothermia may cause adverse events such as cardiac dysfunction, arrhythmias, deterioration of microcirculation and oxygen consumption, coagulopathy, or cold-induced diuresis, core body temperature should be maintained at ‡ 35C, e.g., by means of convective warming blankets or warming of fluids. because of central diabetes insipidus, excessive fluid replacement to ensure hemodynamic stability or the aftermath of osmotic diuresis with mannitol for the treatment of increased intracranial pressure. Because elevated sodium levels have been associated with higher rates of primary graft failure (36, 69), it is essential to compensate hypernatremia by infusing 5% dextrose solution in water or half normal saline (0.45%) as well as treating potential causes, e.g., hormonal replacement with arginine– vasopressin or desmopressin. Besides, maintenance of metabolic and respiratory acid–base balance has to be considered in potential organ donors. Respiratory alkalosis following hyperventilation during the treatment of increased intracranial pressure worsens tissue oxygenation so that normocapnia should be achieved. On the other hand, metabolic acidosis most likely resulting from an increase in metabolic activity because of a lack of T3 in potential organ donors (81) may worsen cardiac function necessitating correction with trometamol or sodium bicarbonate (16). Conclusion In summary, caring for a brain dead potential organ donor requires a shift in critical care therapy from the extensive treatment of increased intracranial pressure toward strategies to maintain donor organ function. A systematic and optimized critical care management (as summarized in fig. 2) increases not only the number, but also the quality of suitable organs, aiming at an optimal outcome for the recipients. Coagulopathy Conflicts of interest Because of the pathophysiological changes described previously, brain death is associated with an increased risk of disseminated intravasal coagulopathy one has to be aware of (15). Generally, accepted goals of therapy include an international normalized ratio (INR) of < 1.5 and a platelet count of > 50 000/mm3, and replacement of clotting factors with fresh frozen plasma and platelet transfusions should be adjusted to these goals; however, to date there are no conclusive evidence-based data available. CD and RA have no conflicts of interest. BV, ME and AU have not declared any conflicts of interest. Maintenance of electrolyte levels as well as metabolic and respiratory acid–base balance Disturbances in electrolyte levels, mainly hypernatremia (serum sodium level > 150 mM) and hypokalemia, occur frequently in brain dead potential organ donors and are a result of polyuria References 1. Lopez-Navidad A, Domingo P, Caballero F. Organ shortage: viability of potential organ donors and possible loss depend on health care workers who are responsible for the organ procurement program. Transplant Proc 1997: 29: 3614. 2. Grossman R. Early enteral formula administration. Crit Care Med 1995: 23: 436. 3. Nygaard CE, Townsend RN, Diamond DL. Organ donor management and organ outcome: a 6-year from a level 1 trauma center. J Trauma 1990: 30: 728. 4. Van Bakal AB. The cardiac transplant donor: identification, assessment, and management. Am J Med Sci 1997: 314: 153. 5. Novitzky D. Detrimental effects of brain death on the potential organ donor. Transplant Proc 1997: 29: 3770. 6. Novitzky D. Donor management: state of the art. Transplant Proc 1997: 29: 3773. 7 Dictus et al. 7. Tuttle-Newhall JE, Collins BH, Kuo PC, Schoeder R. Organ donation and treatment of the multi-organ donor. Curr Probl Surg 2003: 40: 266. 8. Shivarlkar B, Van Loon J, Wieland W et al. Variable effects of explosive or gradual increase of intracranial pressure on myocardial structure and function. Circulation 1993: 87: 230. 9. Carber C, Manyalich M, Valero R, Garcia-Fages LC. Timing used in the different phases of the organ procurement process. Transplant Proc 1992: 24: 22. 10. Kosieradzki M, Kuczynska J, Piwowarska J et al. Prognostic significance injury occurring in the kidney donor. Transplantation 2003: 75: 1221. 11. Lagiewska B, Pacholczyk M, Szostek M, Walaszewski J, Rowinski W. Hemodynamic and metabolic disturbances observed in brain-dead organ donors. Transplant Proc 1996: 28: 165. 12. Finfer S, Bohn D, Colpitts D, Cox P, Fleming F, Barker G. Intensive care management of pediatric organ donors and its effect on post transplant organ function. Intensive Care Med 1996: 22: 1424. 13. Van der Hoeven JA, Ter Horst GJ, Molema G et al. Effects of brain death and hemodynamic status on function and immunologic activation of the potential donor liver in the rat. Ann Surg 2000: 232: 804. 14. Kusaka M, Pratschke J, Wilhelm MJ et al. Activation of inflammatory mediators in rat renal isografts by donor brain death. Transplantation 2000: 69: 405. 15. Hefty TR, Cotterell LW, Fraser SC, Goodnight SH, Hatch TR. Disseminated intravascular coagulation in cadaveric organ donors. Incidence and effect on renal transplantation. Transplantation 1993: 55: 442. 16. Hoemme R, Neeser G. Organ donation. Anaesthesist 2007: 56: 1291. 17. Power BM, Van Heerden PV. The physiological changes associated with brain death-current concepts and implantations for treatment of the brain dead organ donor. Anaesth Intensive Care 1995: 23: 26. 18. Zaroff JG, Rosengard BR, Armstrong WF et al. Consensus conference report: maximizing use of organs recovered from the cadaver donor: cardiac recommendations March 28–29 2001, Crystal City, Va. Circulation 2002: 106: 836. 19. Deman A, Peeters P, Sennesael J. Hydroxyethyl starch does not impair immediate renal function in kidney transplant recipients: a retrospective, multicenter analysis. Nephrol Dial Transplant 1999: 14: 1517. 20. Reilly PM, Grossman M, Rosengard BRE. Lung procurement from solid organ donors: role of fluid resuscitation in procurement failures. Chest 1996: 110: 222S. 21. Rosengard BR, Feng S, Alfrey EJ et al. Report of the crystal city meeting to maximize the use of organs recovered from the cadaver donor. Am J Transplant 2002: 2: 701. 22. Hevesi ZG, Lopukhin SY, Angelini G, Coursin DB. Supportive care after brain death for the donor candidate. Int Anesthesiol Clin 2006: 44: 21. 23. Wood KE, Becker BN, Mccartney JG, DÕAlessandro AM, Coursin DB. Care of the potential organ donor. NEJM 2004: 351: 2730. 24. Wheeldom DR, Potter CD, Oduro A, Wallwork J, Large SR. Transforming the unacceptable donor: outcomes from the adoption of a standardized donor management technique. J Heart Lung Transplant 1995: 14: 734. 25. Potter CD, Wheeldon DR, Wallwork J. Functional assessment and management of heart donors: a rationale 8 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. for characterization and a guide to therapy. J Heart Lung Transplant 1995: 14: 59. Debaveye YA, Van den Berghe GH. Is there still a place for dopamine in the modern intensive care unit? Anesth Analg 2004: 98: 461. Marik PE, Mohedin M. The contrasting effects of dopamine and norepinephrine on systemic and splanchnic oxygen utilization in hyperdynamic sepsis. JAMA 1994: 272: 1354. Tilney NL, Paz D, Ames J, Gasser M, Laskowski I, Hancock WW. Ischemia-reperfusion injury. Transplant Proc 2001: 33: 843. Amado JA, Lopez-Espadas F, Vazquez-Barquero A et al. Blood levels of cytokines in brain-dead patients: relationship with circulating hormones and acute-phase reactants. Metabolism 1995: 44: 812. Stangl M, Zerkaulen T, Theodorakis J et al. Influence of brain death on cytokine release in organ donors and renal transplants. Transplant Proc 2001: 33: 1284. Iwai A, Sakano T, Uenishi M, Sugimoto H, Yoshioko T, Sugimoto T. Effects of vasopressin and cathecholamines on the maintenance of circulatory stability in braindead patients. Transplantation 1989: 48: 613. Katz K, Lawler J, Wax J, OÕConnor R, Nadkarni V. Vasopressin pressor effects in critically ill children during evaluation for brain death and organ recovery. Resuscitation 2000: 47: 33. Hunt SA, Baldwin J, Baumgartner W et al. Cardiovascular management of a potential heart donor: a statement from the transplantation committee of the American College of Cardiology. Crit Care Med 1996: 24: 1599. Marik PE, Varon J, Trask T. Management of head trauma. Chest 2002: 122: 699. Howlett TA, Keogh AM, Perry L, Touzel R, Rees LH. Anterior and posterior pituitary function in brain stem dead donors. A possible role for hormonal replacement therapy. Transplantation 1989: 47: 828. Gramm HJ, Meinhold H, Bickel U et al. Acute endocrine failure after brain death? Transplantation 1992: 54: 851. Shah VR. Aggressive management of multiorgan donor. Transplant Proc 2008: 40: 1087. Avlonitis VS, Fisher AJ, Kirby JA, Dark JH. Pulmonary transplantation: the role of brain death in donor lung injury. Transplantation 2003: 75: 1928. Kutsogiannis DJ, Pagliarello G, Doig C, Ross H, Shemie SD. Medical management to optimize donor organ potential: review of the literature. Can J Anaesth 2006: 53: 820. Wood KE, Coursin DB. Intensivists and organ donor management. Curr Opin Anaesthesiol 2007: 20: 97. Pennefather SH, Bullock RE, Dark JH. The effect of fluid therapy on alveolar arterial oxygen gradient in brain dead organ donors. Transplantation 1993: 56: 1418. Aziz TM, El-Gamel A, Saad RA, Migliore M, Campbell CS, Yonan NA. Pulmonary vein gas analysis for assessing donor lung function. Ann Thorac Surg 2002: 73: 1599. Gabbay E, Williams TJ, Griffiths AP et al. Maximizing the utilization of donor organ offered for lung transplantation. Am J Respir Crit Care Med 1999: 160: 265. Follette D, Rudich S, Bonacci C, Allen R, Hoso A, Albertson T. Importance of an aggressive multidisciplinary management approach to optimize lung donor procurement. Transplantation Proc 1999: 31: 169. Tanaka N. Radiologic-pathologic correlation of experimental bleomycin-induced pneumonitis. Nippon Iqaku Hoshasen Gakkai Zasshi 1993: 53: 1392. Critical care management of potential organ donors 46. Wilheim S, Maze M. Controversial issues in adult and paediatric ambulatory anaesthesia: is there a role for alpha-2 agonist in conscious sedation in adults and paediatric ambulatory surgical practice. Curr Opin Anaesthesiol 2000: 13: 619. 47. Postema S, Pattynama PM, van Rijswijk CS, Trimbos JB. Cervical carcinoma: can dynamic contrast enhanced MR imaging help predict tumor aggressiveness. Radiology 1999: 210: 217. 48. De Boer ML, Hu J, Kalvakolanu DV, Hasdav JD, Cross AS. INF gamma inhibits lipopolysaccharide-induced interleukin 1 beta in primary murine macrophages via a Stat 1 dependent pathway. J Interferon Cytokine Res 2001: 21: 485. 49. Van der Wounde FJ, Ferrario F. Renal involvement in ANCA associated systemic vasculitis. J Nephrol 1999: 12: 105. 50. Itoh M, Kuroda K. Impressions on 11th international conference on Nagative Strand Viruses. Uirusu 2000: 50: 319. 51. Zivna H, Zivny P, Navratil P et al. The role of cytokines and antioxidant status in graft quality prediction. Transplant Proc 1999: 31: 2094. 52. Nagareda T, Kinoshita Y, Tanaka A et al. Clinicopathology of kidneys from brain dead patients treated with vasopressin and epinephrine. Kidney Int 1993: 43: 1363. 53. Pratschke J, Wilhelm MJ, Kusaka M et al. Accelerated rejection of renal allograft from brain dead donors. Ann Surg 2000: 232: 263. 54. Schnuelle P, Berger S, de Boer J, Persijn G, van der Wounde FJ. Effects of catecholamine application to brain dead donors on graft survival in solid organ transplantation. Transplantation 2001: 72: 455. 55. Schnuelle P, Lorenzo D, Mueller A, Trede M, Van der wounde FJ. Donor catecholamine use reduces acute allograft rejection and improves graft survival after cadaveric renal transplantation. Kidney Int 1999: 56: 738. 56. Singer AC, Wong CS, Crowley DE. Differential enantioselective transformation of atropisomeric polychlorinated biphenyls by multiple bacterial strains with different including compounds. Appl Environ Microbiol 2002: 68: 5756. 57. Tepel M, van der Giet M, Schwarzfeld C, Laufer U, Liermann D, Zidek W. Prevention of radiographic contrast agent induced reductions in renal function by acetylcysteine. N Engl J Med 2000: 343: 180. 58. Efrati S, Dishy V, Averbukh M et al. The effect of Nacetylcycteine on renal function, nitric oxide and oxidative stress after angiography. Kidney Int 2003: 64: 2182. 59. Briguori C, Manganelli F, Scarpato P et al. Acetylcysteine and contrast agent associated nephrotoxicity. J Am Coll Cardiol 2002: 40: 298. 60. Diaz-Sandoval LJ, Kosowsky BD, Losordo DW. Acetylcysteine to prevent angiography related renal tissue injury (the APART trial). Am J Cardiol 2002: 89: 356. 61. Kay J, Chow WH, Chan TM et al. Acetylcysteine for prevention of acute deterioration of renal function following elective coronary angiography and intervention: a randomized controlled trial. JAMA 2003: 289: 553. 62. Merten GJ, Burgess WP, Rittase RA, Kennedy TP. Prevention of contrast induced nephropathy with sodium bicarbonate: an evidence based protocol. Crit Pathw Cardiol 2004: 3: 138. 63. Ploeg RJ, DÕAlessandro AM, Knechtle SJ et al. Risk factoers for primary dysfunction after liver transplantation – a multivariate analysis. Transplantation 1993: 55: 807. 64. Clavien PA, Harvey PR, Strasberg SM. Preservation and reperfusion injuries in liver allografts. An overview and synthesis of current studies. Transplantation 1992: 53: 957. 65. Brokelman W, Stel AL, Ploeg RJ. Risk factors for primary dysfunction after liver transplantation in the university of Wisconsin solution era. Transplant Proc 1999: 31: 2087. 66. Porte RJ, Ploeg RJ, Hansen B et al. Lonh term graft survival after liver transplantation in the UW era: late effects of cold ischemia and primary dysfunction. European Multicenter Study Group. Transpl Int 1998: 11(Suppl. 1): S164. 67. Figueras J, Busquets J, Grande L et al. The deleterious effect of donor high plasma sodium and extrended preservation in liver transplantation. A multivariate analysis. Transplantation 1996: 61: 410. 68. Gonzalez FX, Rimola A, Grande L et al. Predictive factors of early postoperative graft function in human liver transplantation. Hepatology 1994: 20: 565. 69. Totsuka E, Dodson F, Urakami A et al. Influence of high donor serum sodium levels on early postoperative graft function in human liver transplantation: effect of correction of donor hypernatremia. Kidney Transpl Surg 1999: 5: 421. 70. Sazontseva IE, Kozlov IA, Moisuc YG, Ermolenko AE, Afonin VV, Ilnitskiy VV. Hormonal response to brain death. Transplant Proc 1991: 23: 2467. 71. Holmes CL, Patel BM, Russell JA, Walley KR. Physiology of vasopressin relevant to management of septic shock. Chest 2001: 120: 989. 72. Novitzky D, Cooper DK, Reichart B. Hemodynamic and metabolic responses to hormonal therapy in brain dead potential organ donors. Transplantation 1987: 43: 852. 73. Rosendale JD, Kauffman HM, McBride MA et al. Aggressive pharmacologic donor management results in more transplanted organs. Transplantation 2003: 75: 482. 74. Jeevanandam V. Triiodothyronine: spectrum of use in heart transplantation. THYROID 1997: 7: 139. 75. Salim A, Vassiliu P, Velmahos GC et al. The role of thyroid hormone administration in potential organ donors. Arch Surg 2001: 136: 1377. 76. Pratschke J, Wilhelm MJ, Kusaka M et al. Brain death and its influence on donor organ quality and outcome after transplantation. Transplantation 1999: 67: 343. 77. Birks EJ, Burton PB, Owen V et al. Elevated tumor necrosis factor alpha and interleukin 6 in myocardium and serum of malfunctioning donor hearts. Circulation 2000: 102(Suppl. 3): III 52. 78. Nijboer WN, Schuurs TA, van der Hoeven JA et al. Effects of brain death on stress and inflammatory response in the human donor kidney. Transplant Proc. 2005 Jan– Feb: 37: 367–9. 79. Gores PF, Gillingham KJ, Dunn DL, Moudry-Munns KC, Najarian JS, Sutherland DE. Donor hyperglycemia as a minor risk factor and immunologic variables as major risk factors for pancreas allograft loss in a multivariate analysis of a single institution s experience. Ann Surg 1992: 215: 217. 80. Smith M. Physiologic changes during brain stem death lessons for management of the organ donor. J Heart Lung Transplant 2004: 23: S217. 81. Powner DJ, Hendrich A, Lagler RG, Ng RH, Madden RL. Hormonal changes in brain dead patients. Crit Care Med 1990: 18: 702. 9